Calf strain muscle spasm of the leg is a common injury, often resulting from overuse or improper form during exercise. This comprehensive guide explores the intricacies of this condition, from its anatomical underpinnings to effective treatment and preventative measures. We’ll delve into the specific muscles involved, the causes, symptoms, diagnosis, and recovery strategies, offering insights into potential complications and long-term management.
Understanding the anatomy of the calf muscles and their intricate interplay is crucial for grasping the mechanics of a calf strain. This understanding will empower you with the knowledge to better protect yourself and effectively manage the condition should it arise.
Definition and Anatomy
A calf strain, often resulting in a muscle spasm of the leg, is a common injury affecting the muscles of the lower leg. It typically involves a tear or stretch in the calf muscles, ranging in severity from a minor to a significant injury. Proper understanding of the anatomy and types of strains is crucial for effective diagnosis and treatment.
Calf Muscle Groups Involved
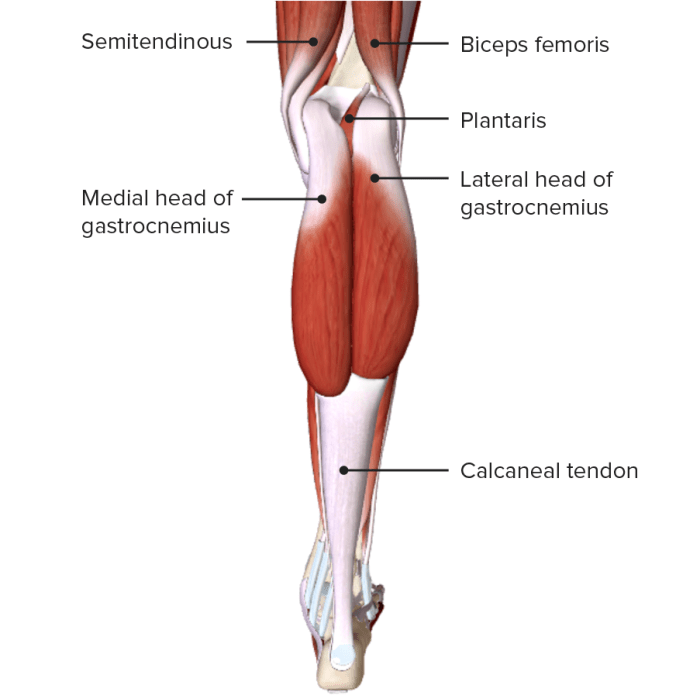
The calf muscles, primarily responsible for plantar flexion (pointing the foot downwards), are comprised of two major muscle groups: the gastrocnemius and the soleus. These muscles work synergistically to generate powerful movements of the ankle and foot. Understanding the specific anatomical locations and functions of these muscles is essential for recognizing the potential sites of injury.
Anatomical Description and Function of Calf Muscles
| Muscle Name | Location | Function | Possible Injury Sites |
|---|---|---|---|
| Gastrocnemius | Located on the posterior (back) aspect of the lower leg, forming the bulk of the calf. Composed of two heads, medial and lateral. | Primary plantar flexor of the foot. Also assists in knee flexion. | Commonly injured at the muscle-tendon junction or within the muscle belly, especially the medial head. |
| Soleus | Located deep to the gastrocnemius, also on the posterior aspect of the lower leg. A larger muscle, it is situated further down the leg. | Secondary plantar flexor of the foot. Crucial for maintaining posture and stability during prolonged standing. It is more active in prolonged plantar flexion. | Often injured at the muscle-tendon junction, similar to the gastrocnemius. Less frequently injured than the gastrocnemius due to its deeper location. |
| Plantaris | A small, thin muscle located deep to the gastrocnemius. | Plays a minor role in plantar flexion and knee flexion. | Rarely injured on its own but can be involved in larger calf injuries. |
Types of Calf Strains
Calf strains are typically categorized into three grades, reflecting the severity of the injury:
- Grade 1 Strain: This involves a minor tear or stretch in the muscle fibers. Symptoms include mild pain, tenderness, and slight swelling. The affected individual may experience some difficulty with activities involving the calf muscles. The muscle might feel slightly warm to the touch. Recovery time is typically relatively short, ranging from a few days to a couple of weeks, depending on the individual’s activity level and adherence to treatment.
This grade often responds well to conservative treatment.
- Grade 2 Strain: This involves a partial tear in the muscle fibers. Pain, swelling, and bruising are more significant than in a Grade 1 strain. There might be a noticeable loss of strength and function in the affected leg. The individual may have difficulty bearing weight. Recovery time for a Grade 2 strain is usually longer, potentially ranging from a few weeks to several months.
Physical therapy and rehabilitation are often necessary to regain full function. It’s important to note that the severity of symptoms can vary based on the individual’s unique anatomy and lifestyle.
- Grade 3 Strain: This represents a complete rupture or tear of the muscle fibers. The injury is extremely painful, and significant swelling and bruising are common. The affected area may feel unstable or give way, making weight-bearing difficult or impossible. Recovery time is typically the longest, potentially exceeding several months or even requiring surgical intervention. This grade typically involves complete loss of function in the affected muscle group, with the individual unable to perform normal activities involving the calf.
That nagging calf strain muscle spasm is a real pain, isn’t it? It can be tough to pinpoint the exact cause, but sometimes underlying conditions like high blood pressure play a role. Understanding the connection between conditions like these and calf muscle spasms is crucial. For example, if you’re curious about how diabetes might contribute to high blood pressure, check out this helpful resource on does diabetes cause high blood pressure.
Regardless of the root cause, consistent stretching and rest are key to recovery from calf strain muscle spasm.
Causes and Risk Factors
Calf strains, unfortunately, are a common ailment among athletes and weekend warriors alike. Understanding the underlying causes and risk factors is crucial for prevention and effective treatment. This knowledge empowers individuals to take proactive steps to safeguard their calf muscles and avoid injury.A thorough comprehension of the mechanisms behind calf strains allows individuals to make informed decisions about their training routines and lifestyle choices.
By identifying potential triggers, individuals can implement strategies to mitigate their risk and promote overall well-being.
Common Causes of Calf Strains
Various factors can contribute to the development of calf strains. Overexertion during physical activities, particularly those involving sudden increases in intensity or duration, is a frequent culprit. Rapid changes in direction or forceful movements can also strain the calf muscles. In some cases, the strain might stem from inadequate stretching or warm-up routines, which can compromise the muscle’s flexibility and resilience.
Insufficient rest between training sessions also plays a role, as it allows the muscles insufficient time to recover and rebuild.
Risk Factors for Calf Strains
Several risk factors heighten the susceptibility to calf strains. Individuals with pre-existing muscle imbalances or weaknesses in the calf muscles are more prone to injury. A history of previous calf strains also significantly increases the risk of recurrence. Furthermore, inadequate warm-up routines and poor training techniques, such as improper form during exercises, can contribute to the likelihood of a calf strain.
Underlying medical conditions, like certain neurological disorders or circulatory issues, can also influence the risk.
Potential Contributing Factors
Several factors can exacerbate the risk of calf strains. Poor training techniques, such as using improper form during exercises, can place excessive stress on the calf muscles, increasing the likelihood of injury. Inadequate warm-up routines fail to prepare the muscles for the demands of exercise, making them more vulnerable to strain. A lack of sufficient rest between training sessions allows insufficient time for muscle recovery and repair, increasing the risk of injury.
Finally, certain underlying medical conditions, such as neurological disorders or circulatory issues, can also impact the muscles’ ability to handle stress, thus increasing the risk of strain.
Comparison of Causes and Risk Factors
| Cause | Description | Risk Factor |
|---|---|---|
| Overexertion | Pushing the muscles beyond their capacity during exercise. | High-intensity workouts, sudden increases in training volume. |
| Inadequate Warm-up | Insufficient preparation of muscles for activity. | Lack of stretching, skipping dynamic movements. |
| Poor Training Techniques | Incorrect form during exercises, leading to uneven stress on muscles. | Improper technique, lack of professional guidance. |
| Previous Injury | History of calf strain or other related injuries. | Weakened or vulnerable muscle tissue. |
Preventative Measures for Calf Strains
Implementing preventive measures can significantly reduce the risk of calf strains. These measures address various contributing factors, allowing individuals to actively manage their risk.
| Prevention | Description | Example |
|---|---|---|
| Proper Warm-up | Preparing the muscles for exercise through dynamic stretches and light cardio. | Walking, jogging, calf raises, and static stretching. |
| Gradual Progression | Increasing training intensity and duration gradually. | Incrementally increasing the weight lifted or running distance. |
| Rest and Recovery | Allowing adequate time for muscle repair and regeneration. | Sufficient sleep and rest days between workouts. |
| Strengthening Exercises | Targeting specific muscles to enhance their strength and resilience. | Exercises like calf raises, and other leg strengthening exercises. |
Symptoms and Diagnosis
Understanding the symptoms and diagnostic methods for a calf strain is crucial for prompt and accurate treatment. A thorough assessment allows healthcare professionals to differentiate this injury from other conditions and initiate the appropriate course of action. Proper diagnosis helps avoid unnecessary delays in recovery and potential complications.
Typical Symptoms of a Calf Strain
Calf strains manifest with a range of symptoms, varying in intensity depending on the severity of the injury. Pain is the most prominent symptom, often localized to the affected muscle group. The pain can be sharp or dull, and it may worsen with activity or stretching. Tenderness and swelling are also common, particularly in the area of the injury.
Muscle spasms, or involuntary contractions, might also occur as a protective mechanism. These spasms can further intensify the pain and limit movement.
Differentiating a Calf Strain from Other Leg Injuries
Accurate diagnosis involves distinguishing a calf strain from other leg injuries that may present with similar symptoms. A thorough physical examination, including palpation of the affected area, helps determine the precise location of pain and tenderness. Comparing the symptoms with those of other potential injuries, such as shin splints, compartment syndrome, or a hamstring strain, can be helpful in narrowing down the diagnosis.
A detailed history of the injury, including the mechanism of injury and the type of activity performed before the onset of symptoms, can further assist in differentiating calf strains from other conditions.
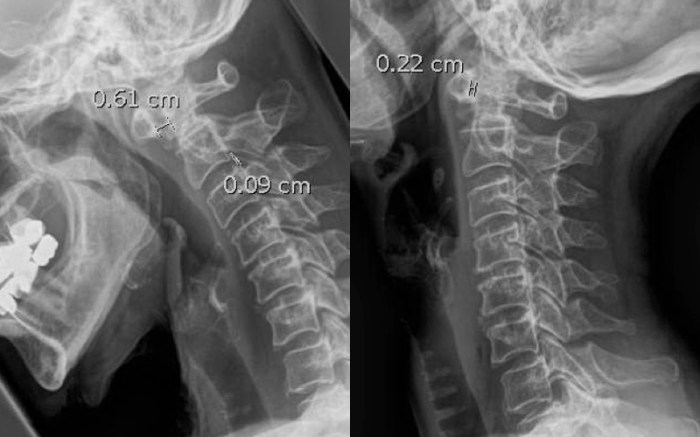
Methods Used to Diagnose a Calf Strain
The diagnostic process for a calf strain typically involves a combination of methods. A physical examination is essential, allowing the healthcare professional to assess the range of motion, palpate the affected area for tenderness, and identify any visible signs of swelling or bruising. This examination can help determine the extent of the injury and guide further investigation. Imaging tests, such as ultrasound or MRI, might be employed to provide a more detailed view of the soft tissues in the affected area.
These imaging techniques can reveal the extent of muscle damage, the presence of any tears, and the involvement of surrounding structures.
Common Symptoms and Severity, Calf strain muscle spasm of the leg
| Symptom | Description | Severity |
|---|---|---|
| Pain | Localized aching or sharp pain in the calf muscle. | Mild, Moderate, Severe |
| Tenderness | Increased sensitivity to touch in the calf muscle. | Mild, Moderate, Severe |
| Swelling | Accumulation of fluid in the calf area. | Mild, Moderate, Severe |
| Muscle Spasms | Involuntary contractions of the calf muscle. | Mild, Moderate, Severe |
Imaging Techniques Used in Diagnosing Calf Strains
| Imaging Technique | Benefits | Limitations |
|---|---|---|
| Ultrasound | Provides real-time images of soft tissues, including muscles and tendons. Relatively inexpensive and readily available. | May not show subtle tears or damage in deeper structures. Image quality can be affected by body habitus. |
| MRI | Detailed images of soft tissues, revealing tears, edema, and other structural abnormalities with high accuracy. Provides a comprehensive assessment of the entire calf region. | More expensive than ultrasound. May not be readily available in all locations. Requires the patient to lie still for an extended period. |
Treatment and Management
A calf strain, or muscle tear in the calf, demands prompt and appropriate treatment to minimize pain, promote healing, and prevent long-term complications. Effective management hinges on a multi-faceted approach addressing immediate pain relief, restoring function, and preventing future injuries. Early intervention significantly improves recovery outcomes.
Immediate Treatment Strategies
Initial care focuses on alleviating pain and preventing further damage. Crucially, the RICE protocol (Rest, Ice, Compression, Elevation) forms the cornerstone of immediate management. Following these steps promptly can significantly reduce swelling and pain, promoting faster healing.
RICE Protocol
- Rest: Avoid activities that aggravate the injury. This crucial step allows the injured muscles to begin the healing process without further stress. Complete rest is paramount in the initial 24-48 hours to allow the tissues to repair. Examples include avoiding running, jumping, or any activities that put stress on the affected leg.
- Ice: Applying ice packs to the affected area for 15-20 minutes at a time, every 2-3 hours, reduces inflammation and pain. Wrap the ice pack in a thin towel to prevent direct skin contact, which can cause frostbite. The application of ice constricts blood vessels, thereby limiting swelling.
- Compression: Using elastic bandages to compress the injured area helps control swelling. Ensure the bandage is snug but not too tight, as this could restrict blood flow. Appropriate compression reduces swelling and supports the injured tissue.
- Elevation: Keeping the injured leg elevated above the heart helps reduce swelling by promoting the drainage of fluid away from the affected area. This position helps minimize the accumulation of blood and fluids in the injured region. Elevating the leg can be achieved by resting on pillows.
Other Relevant Treatment Methods
Beyond RICE, over-the-counter pain relievers like ibuprofen or naproxen can help manage pain and inflammation. In severe cases, a doctor may prescribe stronger pain medications. Proper pain management is crucial for patient comfort and to allow for adequate rest. Physical therapy, discussed further below, is essential for restoring strength and function to the injured area.
Role of Physical Therapy
Physical therapy plays a vital role in rehabilitation, guiding patients through exercises that progressively strengthen the calf muscles and improve flexibility. A physical therapist designs a tailored program to address the specific needs of each individual, ensuring that exercises gradually increase in intensity to promote healing and prevent re-injury. This includes targeted strengthening exercises, stretching routines, and gait training to help the patient regain full range of motion and function.
Conservative vs. Surgical Treatment Approaches
Conservative treatment, which includes RICE, pain medication, and physical therapy, is often the first line of treatment for most calf strains. Surgery is typically reserved for severe or complex cases, such as complete tears or those that don’t respond to conservative methods. Surgical intervention might be necessary to repair significant muscle or tendon damage. Conservative methods offer a less invasive option, but success depends on the severity and type of injury.
Proper Warm-up Routine
A proper warm-up routine before exercising the leg muscles helps prepare the tissues for the demands of activity, reducing the risk of injury. The warm-up should gradually increase the blood flow to the muscles and increase their flexibility. This includes activities like light cardio, such as walking or jogging, and dynamic stretches, such as leg swings, hamstring stretches, and calf raises.
A comprehensive warm-up can significantly reduce the risk of a calf strain.
Prevention and Rehabilitation: Calf Strain Muscle Spasm Of The Leg
Preventing calf strains requires proactive measures to maintain muscle health and flexibility. A comprehensive approach focusing on warm-up, gradual progression, and targeted exercises is crucial for reducing the risk of injury. Rehabilitation, when a strain occurs, involves a structured program to restore strength and function, minimizing long-term impact.
Strategies for Preventing Calf Strains
Proper warm-up and cool-down routines, along with gradual increases in exercise intensity, significantly reduce the risk of calf strains. Maintaining flexibility and strength in the calf muscles through regular stretching and targeted exercises is essential for injury prevention. Avoiding sudden movements or overexertion, particularly when starting a new exercise routine, is also important.
- Consistent Stretching: Regular stretching, incorporating static and dynamic stretches, improves flexibility in the calf muscles. This enhances the range of motion, reducing the risk of strains during activities that demand high levels of movement.
- Gradual Progression: Increasing exercise intensity and duration gradually is vital. Rushing into intense workouts without proper preparation can strain the calf muscles. A gradual approach allows the muscles to adapt and strengthens them progressively.
- Proper Footwear: Wearing appropriate footwear, especially during activities like running or jumping, provides necessary support and cushioning. Supportive shoes help maintain proper alignment and reduce the risk of injury.
Importance of Warm-up and Cool-down Routines
Warm-up routines prepare the muscles for physical activity, increasing blood flow and flexibility. Cool-down routines gradually reduce the heart rate and blood flow, preventing muscle stiffness and soreness. Both are crucial for preventing injuries, particularly calf strains.
- Warm-up: Warm-up activities, such as light cardio and dynamic stretching, increase blood flow to the muscles. This prepares them for the demands of the activity, reducing the risk of strains.
- Cool-down: Cool-down activities, such as static stretching, help reduce muscle tension and soreness. This process facilitates recovery and reduces the risk of delayed-onset muscle soreness (DOMS).
Importance of Gradual Increases in Exercise Intensity
Progressive overload, a principle of training, involves gradually increasing the demands placed on the muscles. This allows the body to adapt and build strength and endurance without exceeding the capacity of the muscles, which can lead to strains.
- Avoid sudden increases: Sudden increases in exercise intensity, duration, or frequency significantly increase the risk of muscle strain. A gradual increase in workload allows the body to adapt and prevents excessive stress on the muscles.
- Listen to your body: Pay attention to any pain or discomfort. If you experience pain, stop the activity and rest. Rest is crucial for muscle recovery and prevents further injury.
Appropriate Exercises for Rehabilitation and Strengthening
Rehabilitation exercises focus on restoring strength and flexibility in the affected calf muscles. A structured program of targeted exercises, tailored to the individual’s specific needs and recovery stage, is essential.
| Exercise Type | Description | Instructions |
|---|---|---|
| Calf Raises | Strengthens the gastrocnemius and soleus muscles. | Stand with feet shoulder-width apart. Raise up onto the balls of your feet, then lower back down. |
| Heel Drops | Stretches the calf muscles. | Stand with feet shoulder-width apart. Lower your heels towards the ground, maintaining a straight back. |
| Toe Raises | Strengthens the anterior tibialis muscle. | Stand with feet shoulder-width apart. Raise up onto your toes, then lower back down. |
| Seated Calf Raises | Strengthens calf muscles, while offering a support system for lower back. | Sit on a chair, place your feet flat on the floor, and lift your heels off the ground, slowly. |
| Standing Calf Raises with Resistance Band | Increases the intensity of calf raises. | Use a resistance band around the balls of your feet. Perform calf raises. |
Potential Complications
A calf strain, while often treatable with rest and proper care, can lead to more serious issues if ignored or mishandled. Understanding potential complications is crucial for prompt and effective management. Ignoring pain and continuing activity can exacerbate the injury, potentially resulting in long-term problems. Proactive management is key to minimizing these risks.Untreated or poorly managed calf strains can lead to chronic issues that affect daily activities and quality of life.
Delayed or inadequate treatment can prolong healing time, increase the risk of re-injury, and even contribute to the development of more significant problems. Early intervention and consistent rehabilitation are essential to prevent these complications.
Long-Term Effects of Untreated Calf Strains
Chronic pain and stiffness are common long-term effects of untreated calf strains. This persistent discomfort can significantly impact mobility and daily tasks. The injured area may also become prone to recurring spasms or tightness. Furthermore, improper healing can lead to the development of scar tissue, which can restrict normal muscle function and potentially affect the range of motion in the affected leg.
Recognizing Signs of Potential Chronic Problems
It’s vital to be aware of the signs that indicate a calf strain might be developing into a chronic issue. Monitoring for changes in pain intensity, duration, and location is critical. If pain persists beyond the typical healing timeframe or if new symptoms emerge, such as swelling, discoloration, or a noticeable change in the muscle’s shape, it’s important to seek medical attention.
Experiencing a calf strain muscle spasm? It’s super frustrating, right? While focusing on the recovery process, did you know that similar muscle tightness can sometimes stem from issues with CPAP therapy? Understanding the causes and treatment of CPAP gas buildup can be helpful for overall well-being, especially if you’re experiencing related muscle discomfort. For in-depth information on this, check out this great resource: the causes and treatment of cpap gas.
Regardless of the cause, proper rest, stretching, and potentially professional guidance are key to getting your calf muscles back to optimal health.
The earlier you identify these signs, the sooner you can implement appropriate treatment strategies.
Possible Consequences of Ignoring a Calf Strain
Ignoring a calf strain can have several negative consequences, ranging from decreased athletic performance to a greater risk of more serious injuries. Prolonged discomfort can lead to reduced mobility and a decreased ability to perform daily activities. Furthermore, ignoring the pain might lead to the injury becoming more severe, requiring extensive treatment and potentially resulting in long-term functional limitations.
Table of Signs of Potential Chronic Problems
| Sign | Description | Potential Implications |
|---|---|---|
| Persistent pain (beyond 6-8 weeks) | Pain that continues despite appropriate rest and treatment. | Possible development of chronic pain syndrome, reduced mobility, and functional limitations. |
| Swelling or inflammation | Continued swelling or redness in the calf area. | Indicates ongoing inflammation, potentially leading to chronic issues. |
| Muscle weakness or atrophy | Noticeable reduction in muscle strength or size in the affected calf. | Reduced ability to perform activities requiring calf muscle strength, potentially leading to re-injury. |
| Changes in skin sensation (e.g., numbness, tingling) | Altered sensation in the calf area. | Could indicate nerve involvement and warrants immediate medical evaluation. |
| Limited range of motion | Difficulty flexing or extending the ankle or knee. | Indicates restricted joint mobility and potential for chronic stiffness. |
Case Studies and Examples
Calf strains, ranging from mild discomfort to debilitating injuries, can significantly impact an individual’s daily activities. Understanding real-world examples of diagnosis, treatment, and recovery is crucial for both patients and healthcare professionals. This section delves into case studies, highlighting how various factors influence the severity and recovery process of calf strains.Case studies and examples are not intended to be a substitute for professional medical advice.
Always consult with a qualified healthcare provider for diagnosis and treatment of any medical condition.
Case Study: A Runner’s Calf Strain
A 28-year-old marathon runner presented with sudden sharp pain in their right calf during a training run. The pain intensified with plantar flexion (pointing the toes downward) and was accompanied by swelling and tenderness along the calf muscle. Physical examination revealed a localized tenderness and limited range of motion in the affected area. Imaging (ultrasound or MRI) confirmed a grade II calf strain, involving partial tearing of the muscle fibers.
Treatment included rest, ice, compression, and elevation (RICE). Physical therapy, focusing on stretching, strengthening exercises, and proprioceptive training, was initiated to restore muscle function and prevent recurrence. The runner followed the prescribed recovery plan meticulously and gradually returned to running after 6 weeks, demonstrating a successful recovery.
Dealing with a calf strain and muscle spasms in your leg can be incredibly painful. One potential natural remedy to explore is magnesium L-threonate, which some studies suggest may help with muscle relaxation. To find the right dosage for your needs, be sure to check out this helpful resource on magnesium l threonate dosage. While magnesium might help, it’s crucial to remember that proper rest and physical therapy are still essential components of recovery from a calf strain muscle spasm.
Factors Affecting Severity
Several factors contribute to the varying degrees of calf strain severity. Training volume and intensity, prior injury history, and the individual’s overall fitness level play a crucial role. A runner who consistently exceeds their training limits is more susceptible to a severe strain compared to someone who maintains a moderate training schedule. Also, individuals with a history of ankle sprains or other lower leg injuries may be at higher risk due to compromised tissues and reduced flexibility.
Sample Recovery Plan for a Calf Strain
A typical recovery plan for a calf strain generally involves the following phases:
- Phase 1 (Acute Phase): Rest, ice, compression, and elevation (RICE) are paramount during the first 48-72 hours to reduce inflammation and pain. Over-the-counter pain relievers may be used to manage discomfort. A physical therapist or physician can advise on the appropriate RICE protocol.
- Phase 2 (Rehabilitation Phase): Gentle range-of-motion exercises and light stretching are introduced as tolerated. As pain subsides, strengthening exercises targeting the calf muscles and surrounding tissues are progressively incorporated. This phase aims to restore muscle function and flexibility.
- Phase 3 (Return to Activity): Gradual return to activities like running, jumping, or other sports is crucial. The individual should start with low-impact activities and gradually increase the intensity and duration of workouts as tolerated. This phase emphasizes avoiding overexertion to prevent re-injury.
Factors Contributing to Successful Recovery
A successful recovery from a calf strain depends on several key factors:
- Adherence to the prescribed treatment plan: Strict adherence to the recommended rest, ice, compression, elevation (RICE), and rehabilitation exercises is crucial for optimal healing.
- Proper nutrition and hydration: Adequate protein intake supports muscle repair, while sufficient hydration aids in tissue recovery.
- Early and appropriate medical intervention: Seeking timely medical advice and following a prescribed treatment plan can significantly reduce recovery time and prevent complications.
- Progressive rehabilitation exercises: Gradual progression of exercises is essential to avoid overexertion and promote a safe and effective recovery.
- Mental well-being: Maintaining a positive mindset and avoiding stress or anxiety is crucial for a smooth recovery process.
- Appropriate footwear and training surfaces: Selecting appropriate footwear and training surfaces can help prevent re-injury by providing adequate support and cushioning.
Illustrations and Visual Aids
Visual aids play a crucial role in understanding and effectively managing calf strain. Detailed images and diagrams can clarify complex anatomical structures, proper treatment techniques, and the progression of rehabilitation. This section provides comprehensive visual representations to aid in the comprehension of calf strain, from its anatomy to management strategies.
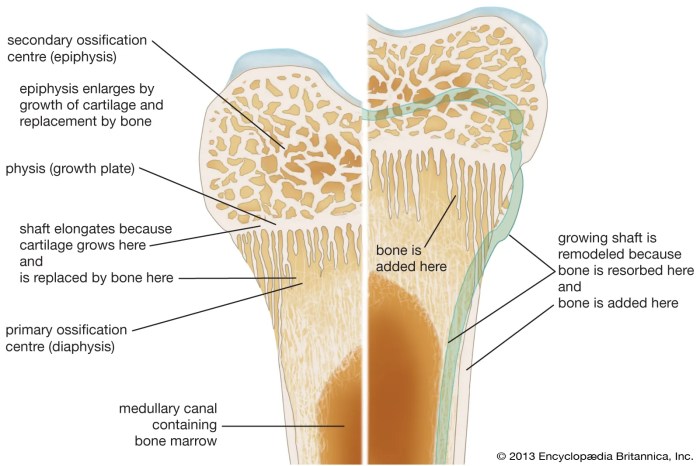
Cross-Section of the Lower Leg
A detailed cross-section of the lower leg reveals the intricate arrangement of muscles, tendons, and ligaments. The image should clearly highlight the gastrocnemius and soleus muscles, which are the primary muscles of the calf. These muscles are positioned strategically in relation to the Achilles tendon, the large band of tissue connecting the calf muscles to the heel bone.
The image should also depict the surrounding connective tissues, such as the fascia, which can be affected in cases of strain. Proper visualization of these structures aids in understanding the potential areas of injury and the mechanisms of strain.
Proper Application of Ice Packs
Visualizing the proper application of ice packs is essential for effective pain management. The image should depict a cold pack wrapped in a thin cloth or towel, applied directly to the affected calf area. The cold pack should cover the injured region without applying excessive pressure. The image should demonstrate the appropriate duration of application, typically 15-20 minutes at a time, with a 1-hour break between applications.
A clear image showcasing the ice pack’s placement, covering the area of the strain, is crucial.
Correct Technique for Stretching the Calf Muscles
Proper stretching techniques are vital for regaining flexibility and preventing future strains. The image should show a person performing a calf stretch. The image should clearly illustrate the correct posture, emphasizing the importance of maintaining a straight back and not bending forward. The foot should be kept flat on the ground. The image should clearly demonstrate the stretch, emphasizing the range of motion required without pushing too far to avoid pain.
The duration of the stretch should be emphasized, generally holding the stretch for 20-30 seconds, and repeating several times daily.
Grades of Calf Strains
Understanding the severity of a calf strain is crucial for appropriate treatment. A diagram illustrating the different grades of calf strains is essential. The diagram should visually represent the varying degrees of muscle damage, from mild (grade 1) to severe (grade 3). Grade 1 strains may show minor muscle tears, while grade 3 strains involve significant tearing of the muscle fibers.
The diagram should use clear labeling and color coding to distinguish each grade, helping to visually differentiate the severity levels of the injury.
Rehabilitation Program for Calf Strains
A visual representation of a rehabilitation program for calf strains should include a series of exercises, progressively increasing in intensity and complexity. The image should depict a progression of exercises, from basic range-of-motion exercises to more advanced exercises focusing on strength and flexibility. The progression should be clearly indicated, with each exercise demonstrated to aid in understanding the steps involved.
The diagram should emphasize the importance of gradually increasing the intensity and duration of exercises to prevent further injury.
Concluding Remarks

In conclusion, calf strain muscle spasm of the leg, while often painful and disruptive, is manageable with appropriate care. By understanding the causes, symptoms, and treatment options Artikeld in this guide, you can significantly reduce your risk of injury and ensure a swift and complete recovery. Remember prevention is key, so prioritize proper warm-up routines, gradual intensity increases, and appropriate exercise techniques.