RSV and rash symptoms link and treatment is a crucial topic for parents and caregivers. Understanding the connection between Respiratory Syncytial Virus (RSV) and skin rashes can help in early diagnosis and appropriate management. This comprehensive guide explores the various types of rashes associated with RSV, their symptoms, potential causes, diagnostic methods, treatment strategies, and preventative measures.
Rashes can manifest in different ways, ranging from mild to severe, and their appearance can vary depending on the underlying cause. This guide delves into the intricate relationship between RSV and rashes, providing a thorough understanding of the symptoms, potential complications, and available treatment options.
Introduction to Rashes and Related Symptoms
Rashes are a common skin condition characterized by changes in the skin’s appearance, texture, or color. They can range from mild and temporary to severe and persistent, and can be caused by a variety of factors. Understanding the different types of rashes, their associated symptoms, and the role of the immune system in skin reactions is crucial for proper diagnosis and treatment.
This information can help you better understand your own skin health and the health of those around you.Rashes are often accompanied by other symptoms, such as itching, pain, or fever. The severity of these symptoms can vary greatly depending on the underlying cause and the individual’s response. The immune system plays a critical role in skin reactions.
When the immune system encounters a foreign substance or an irritant, it can trigger an inflammatory response in the skin, leading to the development of a rash.
RSV and rash symptoms can sometimes be tricky to pinpoint, but thankfully, treatment options are readily available. While a rash isn’t always directly linked to RSV, it can be a symptom of other underlying conditions. For example, similar symptoms can sometimes mimic rheumatoid arthritis in the neck, a condition that requires careful diagnosis and specialized care. Rheumatoid arthritis in the neck can present with discomfort and stiffness, so understanding the differences is crucial.
Ultimately, proper diagnosis and treatment for RSV and rash symptoms rely on a doctor’s evaluation.
Types of Rashes
Rashes can manifest in various ways, including maculopapular, vesicular, and pustular eruptions. Maculopapular rashes appear as flat, discolored spots (macules) that may be accompanied by small, raised bumps (papules). Vesicular rashes involve small blisters filled with fluid, often seen in viral infections. Pustular rashes are characterized by pus-filled blisters. Understanding the specific type of rash can help narrow down potential causes.
Common Symptoms of Rashes
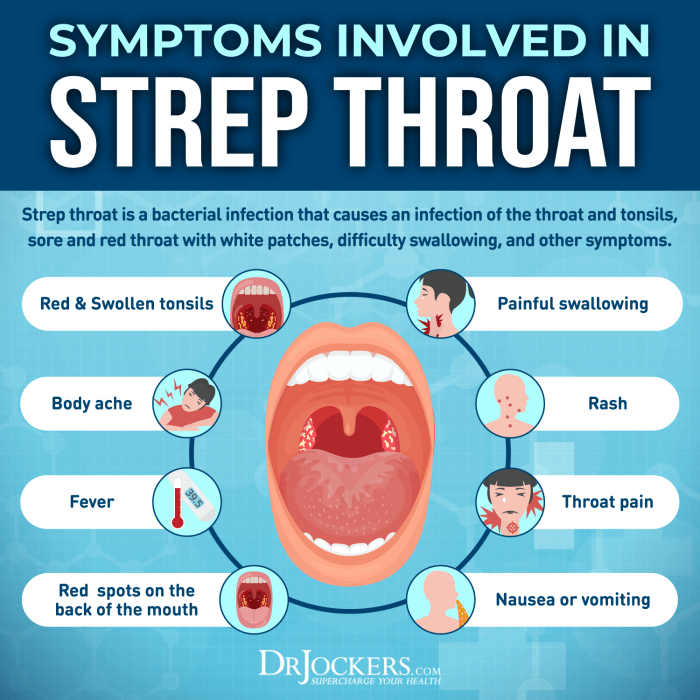
Common symptoms associated with rashes include itching, pain, redness, swelling, and fever. Itching is often a prominent symptom, causing discomfort and leading to scratching. Pain can range from mild to severe, depending on the cause of the rash. Redness and swelling are visible signs of inflammation, while fever can indicate a more serious underlying condition.
Immune System’s Role in Skin Reactions
The immune system is crucial in protecting the body from pathogens and harmful substances. When the immune system detects a foreign invader, it triggers a cascade of reactions, including the release of inflammatory mediators that can lead to skin reactions, such as rashes. The immune system’s response to allergens or irritants can also cause rashes. These reactions vary in intensity, and factors such as genetics and pre-existing conditions can influence the severity of the skin response.
Rash Types, Symptoms, and Potential Causes
| Rash Type | Common Symptoms | Possible Causes |
|---|---|---|
| Maculopapular | Flat, discolored spots (macules), small raised bumps (papules), itching, redness | Viral infections (e.g., measles, rubella), allergic reactions, drug reactions, some bacterial infections |
| Vesicular | Small blisters filled with fluid, itching, pain, redness | Viral infections (e.g., chickenpox, herpes), allergic reactions, certain skin conditions (e.g., eczema) |
| Pustular | Pus-filled blisters, itching, pain, redness, swelling | Bacterial infections (e.g., impetigo), some skin conditions (e.g., acne), drug reactions |
Understanding the Link Between RSV and Rashes
RSV, or Respiratory Syncytial Virus, is a common viral infection that primarily affects the respiratory system. While it’s most known for causing congestion, coughing, and breathing difficulties, it can sometimes be associated with skin reactions, manifesting as rashes. Understanding the connection between RSV and rashes is crucial for accurate diagnosis and appropriate management.Rashes in children can stem from a variety of factors, including viral infections, allergic reactions, and even certain medications.
Identifying the specific cause of a rash is essential for guiding treatment and preventing further complications. In some instances, RSV infection can trigger a secondary skin reaction, which often appears as a characteristic rash. It’s important to differentiate between RSV symptoms and rash symptoms to provide the most effective care.
Common Causes of Rashes in Children
Several factors can contribute to the development of rashes in children. Viral infections, such as chickenpox, measles, and rubella, are known to produce distinctive skin eruptions. Bacterial infections can also cause rashes, as can allergic reactions to food, medications, or environmental triggers. Skin irritations from contact with certain substances or physical trauma can also result in a rash.
Additionally, some underlying medical conditions can manifest as skin rashes.
How RSV Infection Can Lead to Skin Reactions
RSV infection, while primarily targeting the respiratory system, can sometimes trigger a secondary skin reaction. This may occur due to the body’s immune response to the virus, leading to inflammation and skin irritation. The exact mechanism through which RSV leads to rashes isn’t fully understood in all cases. However, in some instances, the immune response to the virus can cause inflammation and subsequent skin eruptions.
This can also be a symptom of other infections, and a doctor’s assessment is critical to determining the precise cause.
Comparison of RSV Symptoms and Rash Symptoms
Identifying the specific symptoms associated with RSV is crucial for accurate diagnosis and treatment. RSV typically presents with respiratory symptoms, such as runny nose, congestion, coughing, and sometimes difficulty breathing. Rashes, on the other hand, manifest as skin eruptions, varying in appearance depending on the cause. Rashes can be accompanied by other symptoms, such as itching, fever, or swelling.
Careful observation of both respiratory and skin symptoms is vital for accurate diagnosis.
Table Contrasting Common Symptoms of RSV and Various Rash Types, Rsv and rash symptoms link and treatment
| Symptom Category | RSV | Viral Rash (e.g., Measles) | Allergic Rash (e.g., Contact Dermatitis) |
|---|---|---|---|
| Respiratory Symptoms | Runny nose, congestion, cough, difficulty breathing | Possible fever, cough, runny nose, body aches | None |
| Skin Symptoms | Possible, but usually not prominent | Distinctive rash, often with spots or blisters | Redness, itching, localized rash at contact site |
| Other Symptoms | Fever, body aches, fatigue | Fever, body aches, fatigue, possible eye redness | Itching, swelling, localized redness, and discomfort |
Identifying and Differentiating Rash Types Associated with RSV

RSV, or Respiratory Syncytial Virus, often presents with various symptoms beyond respiratory issues. A rash can sometimes accompany the infection, though it’s not a common presentation. Understanding the potential types and characteristics of these rashes can aid in proper diagnosis and management. Knowing how a rash develops can also help distinguish it from other conditions.Identifying the specific type of rash associated with RSV can be challenging, as it often shares characteristics with other viral or allergic skin conditions.
Accurate identification relies on a thorough evaluation by a healthcare professional, considering the overall clinical picture, including other symptoms, and the patient’s medical history.
Potential Rash Types Associated with RSV
A variety of rashes can potentially be linked to RSV. The exact nature of the rash can vary considerably, depending on the individual and the severity of the infection. Some potential characteristics, however, are more common than others.
Characteristics of Rashes
The appearance and distribution of the rash can provide clues about its possible cause. A maculopapular rash, characterized by flat, red spots or slightly raised bumps, is one potential type. These spots might be scattered across the body or concentrated in specific areas. Alternatively, the rash could manifest as a petechial rash, presenting tiny red or purple spots that don’t blanch (fade) when pressed.
Sometimes, a morbilliform rash, resembling measles, can develop, characterized by a slightly raised, red rash that may be accompanied by small bumps or spots. In rarer instances, a purpuric rash, with larger purple or red spots, may occur. The texture of the rash might range from smooth to slightly rough or bumpy. The progression of these rashes can also vary; some may appear quickly, while others might develop gradually over several days.
Typical Rash Progression
The rash’s progression often coincides with the overall course of the RSV infection. The rash typically appears alongside other symptoms, such as fever, runny nose, and cough. The rash itself usually does not cause significant discomfort or pain, though its appearance may be concerning. The duration of the rash generally aligns with the duration of the RSV infection, resolving as the infection subsides.
Summary Table
| Rash Type | Characteristics | Potential Link to RSV |
|---|---|---|
| Maculopapular | Flat, red spots or slightly raised bumps, scattered or concentrated. | Possible, but not definitive. |
| Petechial | Tiny red or purple spots that do not blanch with pressure. | Possible, but not definitive. Requires further evaluation. |
| Morbilliform | Measles-like rash, slightly raised red rash with small bumps or spots. | Possible, but not definitive. Requires further evaluation. |
| Purpuric | Larger purple or red spots. | Possible, but not definitive. Requires immediate medical attention. |
Methods for Diagnosing RSV-Related Rashes
Pinpointing the cause of a rash, especially when linked to respiratory illnesses like RSV, requires a multi-faceted approach. A thorough understanding of the patient’s symptoms, medical history, and exposure factors is crucial. This often involves a combination of clinical assessments and diagnostic tests to accurately identify the presence of RSV and determine if the rash is a direct consequence or merely coincidental.
Confirming RSV Infection
Accurate diagnosis of RSV relies on a combination of clinical observation and laboratory tests. The presence of typical RSV symptoms, such as runny nose, cough, fever, and wheezing, significantly increases the suspicion of an RSV infection. These symptoms, combined with the timing and characteristics of the rash, can provide crucial clues for diagnosis.
Identifying Rash Types
Visual assessment of the rash is an essential component of diagnosis. The type, location, appearance, and evolution of the rash can provide valuable insights into its potential causes. Different rash types associated with RSV can manifest in various ways, ranging from subtle maculopapular eruptions to more pronounced, widespread erythematous patches. The rash’s characteristics, such as its color, texture, and distribution, can provide clues about its etiology.
RSV and rashes can be tricky, right? Figuring out the connection between symptoms and treatment can be confusing. While researching the best ways to handle those pesky symptoms, I stumbled across some interesting information about whether pickles contribute to weight loss, which I thought was quite intriguing! Are pickles good for weight loss ? It’s important to note that this doesn’t mean pickles are the cure-all, but it’s fascinating to see how various foods can impact our health.
Ultimately, a doctor’s guidance is essential for proper RSV and rash symptom management.
The doctor will meticulously document these details for proper diagnosis and treatment.
Diagnostic Tests
Several diagnostic tests can aid in confirming RSV infection and identifying associated rash types. Nasal swabs, a common procedure, collect respiratory secretions for laboratory analysis. The presence of RSV in these samples is a strong indicator of an infection.
- Nasal Swab: This is a straightforward procedure involving the collection of a sample from the nasal passages. The collected sample is then sent to a laboratory for analysis to detect the presence of RSV. The speed and accuracy of this method are valuable in timely intervention.
- Blood Tests: While less frequently used for initial diagnosis, blood tests can sometimes help identify inflammatory markers, indicative of an infection. Elevated levels of certain proteins can suggest an immune response, which can assist in distinguishing between various causes of the rash.
Physical Examination
A comprehensive physical examination is crucial for assessing the patient’s overall condition. The doctor will carefully examine the rash, noting its characteristics, location, and distribution. This visual evaluation helps determine the extent of the rash and the potential causes. Simultaneously, the doctor will assess other signs and symptoms, including the severity of the respiratory illness, the presence of other complications, and any other unusual findings.
- Rash Evaluation: The physician will closely examine the rash, noting its morphology, distribution, and any associated symptoms. This includes looking at the rash’s size, shape, color, and any accompanying signs like itching or tenderness.
- Systemic Assessment: The physician will conduct a thorough evaluation of the patient’s overall health, including respiratory status, temperature, and any other related symptoms. This holistic approach helps in pinpointing potential underlying conditions or complications.
Treatment Strategies for RSV-Associated Rashes
RSV, or respiratory syncytial virus, often presents with various symptoms, including rashes. While a rash itself isn’t directly treated with RSV medications, managing the underlying infection and the associated symptoms is crucial. Effective treatment focuses on alleviating discomfort and preventing complications.Addressing RSV-associated rashes involves a multifaceted approach, recognizing that the rash is a symptom of the viral infection, not a primary condition.
Symptom management plays a critical role in ensuring patient comfort and preventing secondary infections. The appropriate medications are selected based on the severity of symptoms and the specific rash type.
Treatment Options for RSV Infection
Effective treatment for RSV infection prioritizes symptom management rather than a cure for the virus itself. Supportive care is key, aiming to alleviate symptoms and prevent complications. This includes adequate hydration, rest, and over-the-counter medications for fever and discomfort.
Importance of Symptom Management for Rashes
Symptom management for rashes associated with RSV focuses on soothing the skin and reducing inflammation. This often involves applying cool compresses or using gentle, hypoallergenic moisturizers to maintain skin integrity. Avoiding harsh soaps and irritating fabrics is also essential. The goal is to minimize itching and discomfort while allowing the rash to resolve naturally as the RSV infection subsides.
RSV and rash symptoms can be tricky, and figuring out the connection and treatment can be a real headache. While there’s no direct link between RSV and the best birth control, understanding the different symptoms is crucial for effective management. If you’re looking for more information on what birth control options are available and which might be the best fit for your needs, check out this helpful resource: what is the best birth control.
Ultimately, proper diagnosis and treatment for RSV-related rashes still rely on consulting a healthcare professional.
Appropriate Medications for Symptom Relief
Several medications can provide symptom relief for RSV-related rashes. Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage fever and body aches. Antihistamines can be used to reduce itching, particularly if the rash is itchy. In some cases, topical corticosteroids might be prescribed by a doctor to reduce inflammation if the rash is severe or accompanied by significant discomfort.
It’s important to remember that these medications should only be used as directed by a healthcare professional.
Comparison of Treatment Approaches for Various Rash Types
| Rash Type | Treatment Approach | Key Considerations |
|---|---|---|
| Maculopapular Rash (flat, slightly raised spots) | Gentle skin care, cool compresses, over-the-counter antihistamines, and pain relievers as needed. | Monitor for signs of infection, avoid harsh soaps or scrubbing. |
| Vesicular Rash (small blisters) | Gentle skin care, avoiding scratching to prevent further irritation, and over-the-counter antihistamines, pain relievers. | Keep blisters covered to prevent infection, maintain good hygiene. |
| Erythematous Rash (reddened skin) | Cool compresses, gentle moisturizers, and oral antihistamines if itching is present. | If the rash is widespread or accompanied by high fever, consult a healthcare professional. |
| Petechial Rash (small red spots due to bleeding) | Monitor closely for progression. Seek immediate medical attention if the rash worsens or is accompanied by other concerning symptoms. | This type of rash requires prompt medical evaluation to rule out more serious underlying conditions. |
Home Care and Prevention

Managing RSV and its associated rashes at home involves a multifaceted approach focusing on symptom relief and preventing further complications. This section provides practical guidance for soothing skin irritations, managing respiratory symptoms, and taking steps to prevent the spread of the virus. Proper home care can significantly improve comfort and recovery time.Effective home care for rashes involves recognizing the type of rash and tailoring treatment accordingly.
Identifying the specific cause of the rash is crucial for selecting appropriate home remedies and avoiding potential exacerbations. Preventive measures are equally important to minimize the risk of RSV infection and subsequent skin reactions.
Home Care for Rashes
Home care for rashes associated with RSV often focuses on soothing the affected skin and managing any accompanying discomfort. Gentle cleansing, avoiding harsh soaps, and applying cool compresses can alleviate itching and inflammation. Moisturizers can help restore skin hydration and prevent dryness, a common issue with skin irritations. Keeping the affected area clean and dry is essential to prevent secondary infections.
Preventing RSV Infection
Preventing RSV infection is paramount to avoiding the development of associated rashes. Hand hygiene plays a critical role in limiting the spread of the virus. Frequent handwashing with soap and water, especially after touching surfaces or objects in shared environments, is highly recommended. Encouraging the practice of good hygiene in children is crucial to prevent the transmission of RSV in families and communities.
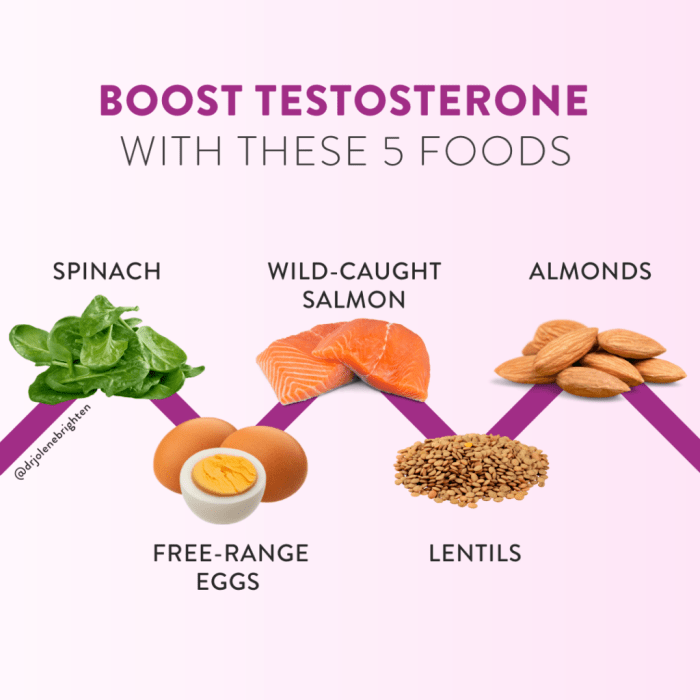
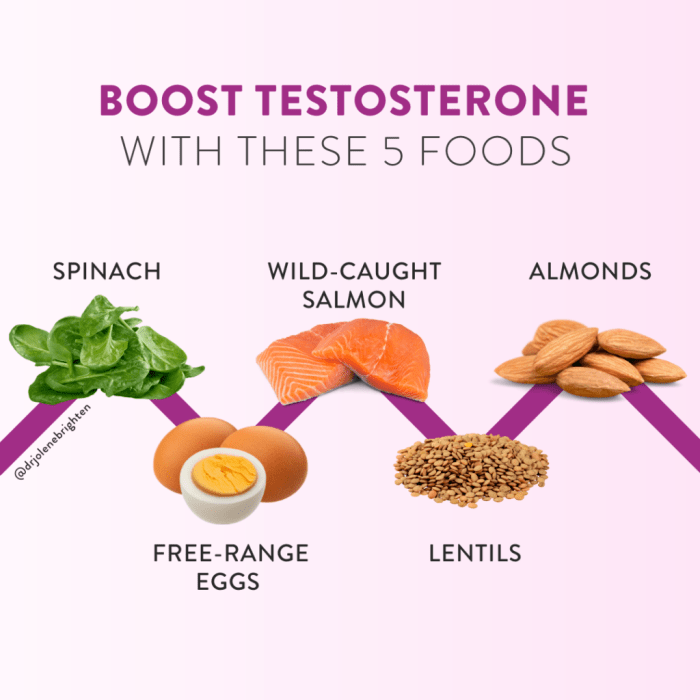
Disinfecting frequently touched surfaces can also help minimize the risk of transmission. Maintaining a healthy immune system through a balanced diet and adequate rest further strengthens the body’s defense mechanisms against RSV.
Managing Symptoms at Home
Managing symptoms at home, including respiratory issues and skin discomfort, is crucial for ensuring comfort and facilitating recovery. Using cool compresses can soothe irritated skin, offering temporary relief from itching and inflammation. Moisturizing creams and lotions can maintain skin hydration, preventing dryness and cracking, and promoting healing. Adequate hydration by encouraging the intake of fluids helps thin secretions and aid in recovery.
Ensuring adequate rest and a calm environment promotes overall well-being.
Home Remedies for RSV-Related Rashes (Table)
| Home Remedy | Potential Effectiveness | Important Considerations |
|---|---|---|
| Cool Compresses | Generally effective in reducing itching and inflammation. | Apply for short durations to avoid skin irritation. |
| Oatmeal Baths | Potentially soothing for skin irritation; may reduce itching. | May not be suitable for all skin types; avoid excessive use. |
| Aloe Vera Gel | May provide soothing and moisturizing effects. | Ensure the aloe vera is pure and free from irritants. |
| Calamine Lotion | Can help soothe itching and irritation. | May stain fabrics; avoid contact with eyes. |
| Moisturizing Creams/Lotions | Essential for maintaining skin hydration. | Select a fragrance-free, hypoallergenic formula. |
Complications and When to Seek Medical Attention
RSV, while often a mild illness, can sometimes lead to more serious complications, particularly in vulnerable individuals. Understanding the potential complications and knowing when to seek medical attention is crucial for ensuring a positive outcome. Early intervention can significantly reduce the severity of these complications and prevent long-term health problems.
Potential Complications of RSV-Related Rashes
RSV-related rashes, though generally harmless, can sometimes signal underlying conditions or complications. These can range from minor discomfort to more significant issues. Some individuals might experience secondary infections, such as bacterial skin infections, which can worsen the rash and require specific treatment. In rare cases, a severe rash can indicate a more serious illness requiring immediate medical attention.
Severity of Complications and Their Impact
The severity of complications varies greatly depending on several factors, including the age and overall health of the individual, the presence of pre-existing conditions, and the type of rash. Infants, young children, and those with weakened immune systems are at higher risk of developing complications. The impact can range from discomfort and inconvenience to potentially life-threatening conditions.
When to Seek Immediate Medical Attention for Rash Symptoms
Prompt medical attention is crucial when certain signs and symptoms associated with RSV-related rashes emerge. These signs can vary based on the individual’s overall health.
- A rash that spreads rapidly or covers a large area of the body.
- A rash accompanied by high fever, persistent or worsening body aches, or difficulty breathing.
- A rash that appears in conjunction with other concerning symptoms, such as lethargy, decreased appetite, or difficulty swallowing.
- A rash that shows signs of infection, such as pus-filled blisters, open sores, or increased redness and swelling.
- A rash that does not respond to home remedies within a reasonable timeframe, or shows worsening signs.
Signs Indicating Urgent Medical Care
Certain signs indicate a need for immediate medical care. Early intervention is crucial in these situations to prevent further complications.
- Difficulty breathing or shortness of breath, especially in infants and young children.
- Bluish discoloration of the skin (cyanosis), particularly around the lips and fingertips.
- Severe or persistent headache.
- Confusion or disorientation.
- Seizures or convulsions.
Important Considerations
It is essential to remember that this information is for general knowledge and does not substitute professional medical advice. Always consult a healthcare provider for accurate diagnosis and treatment of any rash or illness, especially in children. A healthcare professional can assess the individual’s specific situation and provide personalized guidance. Early intervention and appropriate medical care are key to managing RSV-related rashes effectively and minimizing potential complications.
Illustrations of RSV-Related Rash Types
RSV infections, while primarily affecting the respiratory system, can sometimes manifest with skin rashes. Understanding the various types of rashes associated with RSV can aid in early diagnosis and appropriate management. Recognizing these patterns can help distinguish RSV from other viral infections that might also present with skin manifestations.Recognizing the appearance, distribution, and progression of these rashes is crucial for accurate diagnosis and appropriate management.
The rash’s characteristics can provide valuable clues about the underlying cause and potential complications. This section will detail the common rash types linked to RSV, highlighting their distinct features and patterns.
Maculopapular Rash
Maculopapular rashes are characterized by flat, discolored spots (macules) that may evolve into slightly raised bumps (papules). These rashes often appear as a diffuse, reddish or pinkish eruption across the body, particularly on the trunk and extremities. The spots are typically small, ranging from a few millimeters to about a centimeter in diameter. They can appear in a scattered pattern or be clustered together.
The distribution of the rash is usually symmetrical, meaning it affects similar areas on both sides of the body.
Morbilliform Rash
Morbilliform rashes, resembling measles, are characterized by small, flat, reddish-purple spots that coalesce to form a more extensive, blotchy rash. The rash often begins on the face, typically behind the ears, and then spreads downwards to the neck, trunk, and extremities. The rash may have a slightly rough texture. The spots can vary in size, but generally, they are smaller than the macules in a maculopapular rash.
This rash often appears in crops, meaning new spots emerge over a period of hours or days.
Petechial Rash
Petechiae are tiny, pinpoint-sized, purplish-red spots that do not blanch (fade) when pressed. They are caused by bleeding under the skin. A petechial rash associated with RSV may appear in clusters, often on the lower extremities and/or the trunk. The distribution of the rash may be diffuse or localized. This rash type is less common in RSV infections and warrants careful evaluation by a healthcare professional.
Their presence should prompt immediate medical attention, as they may indicate a more severe condition.
Urticarial Rash (Hives)
Urticarial rashes, commonly known as hives, are characterized by raised, itchy welts that vary in size and shape. They are typically erythematous (reddish) and surrounded by a pale area. The welts may appear anywhere on the body, but they often involve the face, neck, or trunk. The rash can change location and shape rapidly. Hives can be associated with RSV, but they are more frequently linked to other allergic reactions or conditions.
It’s important to note that while hives themselves aren’t typically a serious complication of RSV, the itching and discomfort they cause can be bothersome.
Final Review: Rsv And Rash Symptoms Link And Treatment
In conclusion, recognizing the link between RSV and rashes is vital for timely intervention. Early diagnosis, appropriate treatment, and preventive measures can significantly reduce the severity of symptoms and complications. By understanding the various types of rashes, their characteristics, and the diagnostic process, individuals can effectively manage RSV-related skin conditions. This comprehensive guide aims to equip readers with the knowledge to navigate this often challenging situation.











![21 Best Low Sodium Snacks [Dietitian Approved] - The Geriatric Dietitian Sodium sodium or salt sodium functions sodium and diet](https://healthytipp.com/wp-content/uploads/2025/06/sodium-chloride-ionic-bond-formation-nacl-structure-sodium-and-chlorine-atom-chemical-reaction-electron-transfer-electrostatic-attraction-force-2T10E8C-1.jpg)