Smell and brain health are deeply intertwined. Our sense of smell, often overlooked, plays a crucial role in memory, mood, and cognitive function. This exploration delves into the fascinating neural pathways connecting the nose to the brain, uncovering how smells can trigger powerful memories, influence our emotional states, and even impact our overall well-being. We’ll also examine how environmental factors and neurological conditions can affect our sense of smell and its connection to brain health.
The olfactory system, surprisingly complex, interacts with various brain regions. From the olfactory bulb to the amygdala and hippocampus, the journey of an odor molecule is a journey through the brain, influencing our perception, memories, and emotional responses. This intricate network highlights the profound impact of smell on our daily lives, influencing everything from our food preferences to our overall sense of wellbeing.
Furthermore, understanding how smell is processed can offer valuable insights into the diagnosis and treatment of certain neurological conditions.
The Nose and the Brain
The sense of smell, a fundamental aspect of our sensory experience, is intricately linked to the brain. This connection goes beyond simple detection; olfactory information plays a crucial role in memory, emotion, and even our overall well-being. The neural pathways connecting the nose to the brain are complex and fascinating, offering insights into how we perceive and process the world around us.Olfactory perception involves a unique pathway that bypasses the thalamus, the relay station for most sensory information.
This direct route to the brain highlights the importance of smell in triggering immediate emotional responses and associations. The detailed structure and function of the olfactory system, including its interactions with other brain regions, will be explored in the following sections.
The Olfactory Pathway
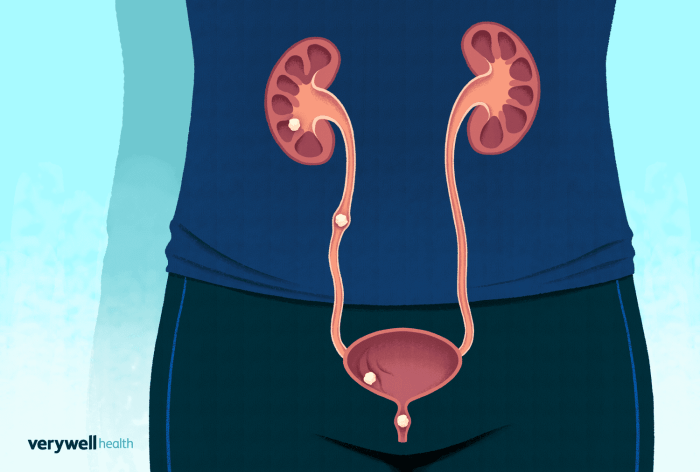
The olfactory system begins with the olfactory epithelium, a specialized tissue lining the nasal cavity. This epithelium houses millions of olfactory receptor neurons, each tuned to detect a specific range of odor molecules. These molecules, inhaled and dissolved in mucus, bind to receptors on the cilia of these neurons, initiating a signal transduction cascade. This process triggers electrical signals that are transmitted along the axons of the olfactory receptor neurons.
Olfactory Bulb and Beyond
These axons project directly to the olfactory bulb, a structure located at the base of the brain. Within the olfactory bulb, the signals are processed and relayed to other brain regions, including the amygdala, hippocampus, and orbitofrontal cortex. The amygdala plays a key role in emotional responses to smells, while the hippocampus connects smells to memories. The orbitofrontal cortex is vital in the conscious perception and interpretation of smells, associating them with specific experiences.
Aging and the Olfactory System
Age-related decline in the olfactory system is a well-documented phenomenon. The olfactory epithelium can lose its sensitivity, and the number of olfactory receptor neurons can decrease. This decline can potentially correlate with cognitive decline in older adults. Loss of smell can affect a person’s quality of life by impacting appetite, taste, and even emotional well-being. For example, a diminished sense of smell might lead to the consumption of spoiled food or the unawareness of a potential fire.
Olfactory Epithelium Structure and Function
The olfactory epithelium is a thin sheet of tissue lining the superior portion of the nasal cavity. It consists of three main cell types: olfactory receptor neurons, supporting cells, and basal cells. Olfactory receptor neurons are the sensory neurons that detect odor molecules. Supporting cells provide structural support and nourishment to the receptor neurons, while basal cells are responsible for replacing damaged receptor neurons.
The intricate arrangement of these cells allows for the detection of a wide variety of odorants.
Comparison with Other Sensory Modalities
The processing of smells differs significantly from other sensory modalities, such as taste or vision. While taste and vision rely on specialized sensory organs and pathways that send signals to the thalamus before reaching the cerebral cortex, smell has a direct pathway to the brain. This direct connection contributes to the rapid and often unconscious emotional responses associated with certain smells.
Taste relies on chemical interactions with specific receptors on the tongue, while vision depends on light waves interacting with photoreceptors in the eye. The olfactory system is more closely linked to emotional and memory centers in the brain than other sensory systems.
Smell and Memory
The human sense of smell is uniquely intertwined with our memories and emotions. A whiff of a familiar scent can instantly transport us back to a specific time and place, evoking vivid recollections and powerful feelings. This remarkable connection lies in the intricate biological pathways that link the olfactory system to the brain regions responsible for memory formation and retrieval.The olfactory bulb, the gateway to the sense of smell, is located close to brain regions critical for memory processing.
This proximity facilitates a direct connection between smells and memories, bypassing some of the usual cognitive filtering processes. This direct route allows for a more immediate and visceral experience, making smell a potent trigger for recalling past events.
Biological Mechanisms of Smell-Memory Association
The olfactory system has a unique pathway to the limbic system, the brain region responsible for emotions and memory. The olfactory bulb directly connects to the amygdala, a structure crucial for processing emotions, and the hippocampus, essential for forming and consolidating memories. This direct neural connection explains why smells can evoke strong emotional responses and specific memories. The close proximity allows for a fast and efficient relay of information, creating a powerful link between the scent and the associated experience.
Impact of Olfactory Experiences on Memory Formation
Olfactory experiences play a significant role in memory formation and retrieval. Exposure to a scent during a significant event can become strongly associated with the event, forming a lasting memory trace. This phenomenon is especially potent during formative years, when the brain is actively developing its neural networks. The combination of sensory input and emotional context creates an enduring memory, with the scent acting as a powerful retrieval cue.
Studies have shown that participants exposed to specific scents during learning tasks demonstrated enhanced recall compared to those without olfactory cues.
Examples of Smells Evoking Powerful Emotional Responses
The impact of smell on emotions is profound. The scent of freshly baked bread can evoke feelings of comfort and nostalgia, reminiscent of a warm family gathering. Conversely, the smell of smoke might trigger feelings of fear and anxiety, reminding individuals of a past fire or other perilous situation. These responses are not arbitrary; they are deeply rooted in the individual’s personal experiences and learned associations.
The potency of smell is further exemplified by the scent of a specific perfume or cologne that can evoke a vivid memory of a loved one.
The Role of the Amygdala and Hippocampus in Linking Smells to Memories
The amygdala and hippocampus are vital in forging the connection between smells and memories. The amygdala processes emotional significance, and the hippocampus consolidates and stores memories. When a specific smell is encountered, signals travel from the olfactory bulb to both the amygdala and the hippocampus. The amygdala identifies the emotional context associated with the smell, while the hippocampus retrieves the associated memory.
This intricate interplay allows for the recall of not just the event, but also the emotional intensity experienced during that event. The combination of these two brain regions allows for the vivid and often emotionally charged recall of past experiences triggered by a smell.
Smell and Mood: Smell And Brain Health
The intricate relationship between smell and mood is a fascinating aspect of our sensory experience. Odors, often imperceptible to conscious awareness, can profoundly impact our emotional state, influencing everything from feelings of calm to feelings of anxiety. This connection stems from the unique neural pathways that connect the olfactory system directly to areas of the brain associated with emotion and memory.The olfactory bulb, the first processing center for smells, sits close to the amygdala and hippocampus, key structures involved in emotional processing and memory formation.
This proximity allows smells to bypass the conscious filtering system and directly trigger emotional responses. This explains why a familiar scent can evoke powerful memories and associated feelings, sometimes even without conscious recognition.
Ever wondered how your sense of smell impacts your brain health? It turns out, a diminished sense of smell can be a surprisingly early warning sign of potential health issues, like fungal infections in the lungs or cancer. For example, a study on fungal infection in lungs or cancer showed a correlation between smell loss and these conditions.
Fortunately, maintaining a healthy sense of smell is often a good indicator of overall brain health. Paying attention to your sense of smell could be a proactive step towards better well-being.
Impact of Different Smells on Mood
Different aromas elicit varying emotional responses. The impact of a scent depends on individual experiences, cultural associations, and even personal preferences. Aromas like lavender, known for its calming properties, can promote relaxation, while citrus scents might induce feelings of alertness and energy.
Aromatherapy and Therapeutic Applications
Aromatherapy leverages the therapeutic properties of essential oils to promote well-being. Many essential oils, like chamomile, are used for their calming effects, while peppermint can be invigorating. These oils are often used in massage, diffusers, or bath products to achieve specific emotional or physiological responses. The practice of aromatherapy is rooted in the understanding that certain smells can influence our emotional state, leading to stress reduction and improved mood.
Physiological Mechanisms of Smell Influence on Mood
The impact of smells on mood is mediated through intricate physiological pathways. When we inhale an aroma, olfactory receptors in the nasal cavity detect the molecules and transmit signals to the olfactory bulb. From there, the signals are relayed to the amygdala and the hippocampus, which process emotions and memories. This direct connection allows smells to bypass the higher-level cognitive processing centers and trigger emotional responses more rapidly and powerfully than other sensory inputs.
Comparison of Pleasant and Unpleasant Smells
Pleasant smells generally trigger positive emotional responses, including feelings of joy, calmness, and relaxation. These sensations are often associated with pleasant memories and positive experiences. Conversely, unpleasant smells, like decaying matter or strong chemicals, can evoke negative emotions like disgust, fear, and anxiety. These responses are rooted in evolutionary adaptations, associating certain odors with potential dangers or threats. The intensity of the emotional response to both pleasant and unpleasant smells can vary greatly between individuals.
Examples of Aromas and Potential Mood Effects
- Lavender: Known for its calming and relaxing properties, often used in aromatherapy to reduce anxiety and promote sleep.
- Citrus fruits (e.g., lemon, orange): Can evoke feelings of alertness, energy, and happiness. These scents are often used in environments where focus and productivity are desired.
- Vanilla: Often associated with comfort and warmth, vanilla can induce feelings of nostalgia and happiness. Its use in baked goods or home fragrances often creates a comforting ambiance.
- Peppermint: Can be invigorating and stimulate mental alertness, often used to enhance focus and concentration.
The impact of these scents on mood can be further nuanced by individual experiences and associations.
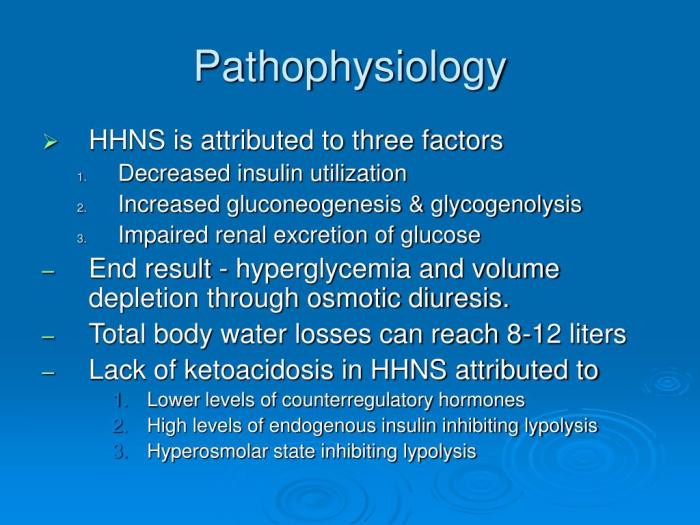
Smell and Neurological Conditions
The sense of smell, often overlooked, plays a crucial role in our overall well-being, deeply intertwined with our memories, emotions, and even our neurological health. Olfactory dysfunction, or problems with the sense of smell, can be a significant symptom or early indicator of various neurological conditions. Understanding the link between smell and the brain’s intricate network is vital for early diagnosis and effective management of these conditions.The olfactory system, responsible for our sense of smell, is closely connected to other brain regions involved in memory, emotion, and cognition.
Damage or disruption in this delicate system can manifest as a range of olfactory symptoms, from complete loss of smell to distortions in odor perception. These changes can be subtle or dramatic, and often accompany other neurological symptoms, making early detection and diagnosis challenging.
Neurological Conditions Affecting Smell
A variety of neurological conditions can impact the sense of smell, ranging from relatively common issues to rarer, more complex conditions. These conditions often involve damage or dysfunction in the olfactory pathways, which transmit smell signals from the nose to the brain.
Relationship Between Olfactory Dysfunction and Other Neurological Disorders
Olfactory dysfunction is frequently observed in conjunction with other neurological disorders. For example, Parkinson’s disease is often associated with hyposmia (reduced sense of smell), which can precede motor symptoms by several years. Similarly, Alzheimer’s disease and other dementias can display a progressive loss of smell. The presence of olfactory impairment can serve as a potential warning sign, potentially prompting earlier evaluation and intervention.
Smell Impairment as an Early Indicator of Disease
In some cases, olfactory impairment can be a very early indicator of certain neurological conditions. The progressive loss of smell in individuals with Alzheimer’s disease, for instance, can sometimes be an initial symptom long before cognitive decline becomes evident. Likewise, in Multiple Sclerosis (MS), olfactory dysfunction can occur due to the autoimmune attack on the nervous system. Recognizing this connection is crucial for prompt diagnosis and treatment.
Diagnostic Potential of Smell Testing
Smell testing, also known as olfactory testing, can be a valuable tool in neurological assessments. These tests, which involve identifying different odors, can help pinpoint specific olfactory impairments. The results, when combined with other clinical findings, can contribute significantly to the diagnostic process and aid in differentiating between various neurological conditions.
Table of Neurological Conditions and Olfactory Impact
| Neurological Condition | Potential Impact on Smell |
|---|---|
| Parkinson’s Disease | Hyposmia (reduced sense of smell) often precedes motor symptoms. |
| Alzheimer’s Disease | Progressive loss of smell, often an early symptom. |
| Multiple Sclerosis (MS) | Olfactory dysfunction due to damage or disruption in the olfactory pathways. |
| Brain Tumors | Olfactory impairment due to direct pressure or damage to the olfactory nerves or pathways. |
| Head Trauma | Loss of smell or distortion of smell perception due to damage to the olfactory system. |
| Nasal Polyps | Obstruction of the nasal passages, impacting smell perception. |
| COVID-19 | Temporary or permanent olfactory dysfunction, known as anosmia or hyposmia, is a common symptom. |
Smell and Cognitive Function
The intricate relationship between our sense of smell and our cognitive abilities is a fascinating area of research. Our noses aren’t just for sniffing out delicious aromas; they play a crucial role in shaping our memories, influencing our emotions, and even impacting our overall cognitive function. This connection is especially pertinent to understanding potential cognitive decline and the strategies to maintain or enhance cognitive performance.Olfactory function, or the ability to perceive smells, is intrinsically linked to various aspects of cognitive processing.
From memory retrieval to attention and decision-making, smell’s impact is demonstrably significant. This influence isn’t limited to everyday experiences; it also holds implications for understanding and potentially mitigating age-related cognitive decline.
Correlation between Olfactory Function and Cognitive Performance
Olfactory function is significantly correlated with cognitive performance across the lifespan. Studies have consistently shown that individuals with better smell identification abilities tend to perform better on cognitive tasks, including memory tests, attention tasks, and executive function assessments. This correlation suggests a direct link between the health of the olfactory system and the overall efficiency of cognitive processes.
The ability to perceive and process smells relies on neural pathways that overlap with those involved in higher-level cognitive functions, contributing to this observed connection.
Evidence Supporting the Link Between Smell Loss and Cognitive Decline
A growing body of evidence supports the link between diminished olfactory function and increased risk of cognitive decline. Numerous studies have shown that individuals experiencing smell loss, often a symptom of neurodegenerative diseases like Alzheimer’s disease, exhibit more pronounced cognitive impairment compared to those with normal olfactory function. This connection is not simply correlational; researchers are beginning to identify potential causal mechanisms, suggesting that smell loss may be an early indicator of cognitive decline or even a contributing factor to its progression.
This finding underscores the importance of olfactory function as a potential marker for early detection and intervention.
Potential for Smell Training to Improve Cognitive Abilities
Smell training, involving the systematic exposure to various scents and subsequent assessments of olfactory identification abilities, shows promise in potentially improving cognitive function. This type of training can stimulate the olfactory system, potentially strengthening neural pathways and enhancing cognitive processes. Furthermore, engaging in activities that rely on smell perception can contribute to the overall maintenance of cognitive health, fostering neural plasticity and potentially delaying cognitive decline.
Comparison of Different Smell Training Programs and their Effectiveness
Various smell training programs exist, employing different methodologies and varying degrees of complexity. Some programs use standardized scent identification tasks, while others incorporate more interactive and multi-sensory approaches. While the effectiveness of smell training in enhancing cognitive abilities remains a subject of ongoing research, preliminary findings indicate a positive impact on olfactory function and related cognitive skills. The long-term effects and optimal protocols for smell training are still being investigated.
Ever wondered how your sense of smell impacts your brain health? Well, it turns out that a healthy nose could potentially play a role in extending your lifespan. Studies are showing a strong connection between olfactory function and overall brain health, which is fascinating, given that what is the human life span is still a subject of ongoing research.
In short, a keen sense of smell might just be a vital key to maintaining cognitive function as we age. The connection between the two remains a vibrant area of investigation.
Further studies are necessary to provide a comprehensive understanding of the effectiveness of different programs and identify the most beneficial approaches.
Studies Demonstrating the Relationship Between Smell and Cognitive Function
| Study | Methodology | Findings |
|---|---|---|
| Study 1 (Example) | Participants were assessed for olfactory function and cognitive performance using standardized tests. | A strong positive correlation was observed between olfactory identification scores and cognitive test scores. |
| Study 2 (Example) | Participants with smell loss were compared to a control group with normal smell function on cognitive assessments. | Significant differences were found in cognitive performance between the two groups, with the smell loss group exhibiting lower scores. |
| Study 3 (Example) | A smell training program was implemented for a specific group, followed by cognitive assessments. | Results showed improvements in olfactory function and certain cognitive domains following the training program. |
Note: This table is an example and does not represent actual studies. Further research is needed to solidify the evidence base. Reliable sources should be consulted for accurate and up-to-date information.
Smell and Health

Our sense of smell, often taken for granted, plays a surprisingly significant role in our overall well-being. From influencing our food choices to potentially signaling early disease indicators, the olfactory system is intricately linked to various aspects of health. This exploration delves into the multifaceted relationship between smell and our physical and mental health.The human sense of smell is a complex sensory system that impacts our daily lives in numerous ways, often beyond our conscious awareness.
Understanding the interplay between smell and health is crucial for appreciating the vital role it plays in maintaining overall well-being.
Potential Health Benefits of a Healthy Sense of Smell
A robust sense of smell is associated with a multitude of positive health outcomes. It enhances our quality of life by enriching our sensory experiences and contributing to our overall well-being.
- Enhanced Food Enjoyment: A keen sense of smell allows us to appreciate the subtle nuances of aromas, significantly impacting our food preferences and enjoyment. This can lead to a more varied and potentially healthier diet.
- Improved Appetite Regulation: Certain smells can stimulate or suppress appetite, impacting our caloric intake. This influence can be harnessed for weight management and maintaining a balanced diet.
- Potential Early Disease Detection: Changes in smell, such as a loss or alteration in olfactory sensitivity, can sometimes serve as an early indicator of underlying medical conditions, including neurological disorders, respiratory illnesses, and certain cancers. For instance, changes in the ability to detect specific odors, like ammonia or certain chemicals, might warrant further medical evaluation.
- Cognitive Stimulation: The olfactory system interacts with other cognitive areas, which can contribute to mental sharpness and memory. Smells can evoke memories and emotions, strengthening our cognitive functions.
Potential Health Risks Linked to Impaired Olfactory Function
Impaired olfactory function, or anosmia, can have significant consequences for health and well-being. It’s crucial to recognize the potential implications of reduced or lost smell.
- Nutritional Deficiencies: Loss of smell can affect appetite and food enjoyment, potentially leading to nutritional deficiencies due to decreased food intake or less varied diet choices. This can be particularly concerning for individuals who rely on smell to appreciate the flavor of their food.
- Safety Concerns: Impaired olfactory function can impact the ability to detect potentially hazardous odors, such as gas leaks or smoke, increasing the risk of accidents or injuries. This highlights the crucial role of smell in safeguarding our well-being in daily life.
- Psychological Impact: Loss of smell can have a substantial impact on mental well-being, leading to feelings of isolation, depression, and reduced quality of life. The ability to experience smells is intricately linked to our sensory world and emotional responses.
- Increased Risk of Certain Diseases: Impaired olfactory function is sometimes associated with various medical conditions, including neurological disorders, infections, and certain types of cancers. Therefore, any significant changes in smell warrant a consultation with a healthcare professional for appropriate diagnosis and treatment.
Smell and Appetite Regulation
Smell plays a crucial role in our experience of food and can profoundly influence our appetite. The olfactory system interacts with the brain’s reward centers, influencing our desire to consume certain foods.
The interaction between smell and appetite is complex, involving both conscious and unconscious processes.
The interplay of smell and taste is crucial in determining our overall food enjoyment and appetite.
Smell in Food Preferences and Enjoyment
The olfactory system is essential in shaping our food preferences and appreciation of flavors. The interplay between smell and taste significantly impacts our overall food experience.
Potential Role of Smell in Detecting Early Signs of Certain Diseases
Changes in smell can sometimes be an early indicator of underlying health issues. Detecting these changes can allow for early intervention and treatment.
Environmental Factors Affecting Smell

Our sense of smell, a crucial component of our overall well-being, is unfortunately susceptible to interference from various environmental factors. Understanding how these external influences impact our olfactory system is vital for maintaining good health and recognizing potential risks. This section delves into the detrimental effects of environmental pollutants and air quality on our ability to perceive odors and experience their impact on our brain health.Environmental pollutants and poor air quality can significantly impair olfactory function, leading to diminished sensitivity to odors.
Ever wondered how powerful smell is for brain health? Well, it turns out that our sense of smell is deeply connected to various cognitive functions. Interestingly, issues like athlete’s foot or other common foot skin problems, like those found on common foot skin problems , can sometimes be a distraction from enjoying a richer sensory experience. Ultimately, keeping your sense of smell sharp is a fantastic way to maintain brain health and well-being.
This impairment can range from mild discomfort to more serious long-term consequences, impacting our cognitive abilities and overall well-being. Understanding the interplay between our environment and olfactory perception is essential for developing preventative strategies and promoting healthier living.
Impact of Environmental Pollutants on the Olfactory System
Environmental pollutants, such as particulate matter, volatile organic compounds (VOCs), and various industrial emissions, can directly damage the delicate olfactory receptors within the nose. These pollutants can irritate the nasal lining, hindering the ability of olfactory receptors to detect and transmit signals to the brain. This disruption can lead to reduced sensitivity to odors, making it difficult to perceive subtle nuances in smells, including potentially harmful ones.
How Air Quality Affects Odor Perception
Air quality plays a pivotal role in our ability to perceive odors. Poor air quality, often associated with high levels of pollutants, can significantly diminish the intensity and clarity of odors. This is because pollutants can bind to odor molecules, masking their scent or altering their perception. Furthermore, high levels of pollutants can lead to inflammation and irritation in the nasal passages, directly impacting the effectiveness of olfactory receptors.
Common Environmental Factors Negatively Affecting the Sense of Smell
Several common environmental factors negatively impact the sense of smell. These include:
- Air pollution, stemming from various sources like traffic emissions, industrial activities, and construction, is a major culprit in reducing odor perception. This pervasive pollution can lead to long-term damage to olfactory receptors.
- Exposure to harmful chemicals, found in many household products, cleaning agents, and industrial environments, can cause irritation and damage to the nasal lining and olfactory receptors. This can lead to temporary or permanent olfactory dysfunction.
- Smoking, both active and passive, is a well-documented irritant that can severely damage the olfactory system. Nicotine and other chemicals in cigarette smoke can inflame the nasal passages and impair the delicate structures responsible for smell.
- Indoor air pollutants, including mold, dust mites, and certain cleaning products, can accumulate within homes and workplaces, affecting indoor air quality and potentially impacting smell perception.
Long-Term Effects of Exposure to Harmful Odors on Brain Health
Chronic exposure to harmful odors and pollutants can have long-term consequences on brain health. This includes potential damage to neural pathways associated with olfaction, which may contribute to cognitive decline and reduced memory function. Research suggests that olfactory impairment may be a predictor of neurological conditions later in life. For instance, prolonged exposure to air pollution has been linked to an increased risk of developing neurodegenerative diseases.
Correlation Between Environmental Factors and Olfactory Function, Smell and brain health
The table below illustrates the correlation between various environmental factors and their impact on olfactory function.
| Environmental Factor | Impact on Olfactory Function |
|---|---|
| Air pollution (e.g., particulate matter, VOCs) | Reduced sensitivity to odors, irritation of nasal lining, potential long-term damage to olfactory receptors. |
| Harmful chemicals (e.g., cleaning agents, industrial solvents) | Inflammation, damage to nasal lining, potential temporary or permanent olfactory dysfunction. |
| Smoking (active/passive) | Inflammation of nasal passages, damage to olfactory receptors, reduced olfactory sensitivity. |
| Indoor air pollutants (e.g., mold, dust mites) | Irritation of nasal passages, potential impairment of odor perception. |
Smell and Wellbeing
Our sense of smell plays a surprisingly significant role in our overall wellbeing, influencing everything from our mood to our stress levels. The olfactory system, directly connected to the limbic system (responsible for emotions and memories), allows smells to evoke powerful responses. This intricate connection highlights the potential of harnessing pleasant aromas to improve our daily lives and promote a sense of calm and contentment.The connection between smell and wellbeing extends beyond simple pleasantness.
The way scents trigger emotional responses, memories, and even physical sensations underscores their importance in our emotional landscape. This powerful link makes smell a valuable tool for stress reduction and enhancing overall psychological health.
Pleasant Smells and Stress Reduction
Pleasant aromas can act as potent stress reducers. The calming effect of certain scents is well-documented, with research suggesting that exposure to these smells can lower cortisol levels, the hormone associated with stress. The activation of the parasympathetic nervous system by calming smells helps induce relaxation and reduce feelings of anxiety. Lavender, chamomile, and sandalwood are examples of scents frequently associated with relaxation.
Psychological Benefits of Pleasant Aromas
Experiencing pleasant aromas can elicit a range of psychological benefits. Beyond simply reducing stress, pleasant smells can evoke positive memories and emotions, potentially boosting overall happiness and well-being. The act of smelling pleasant aromas can foster a sense of calm and serenity, improving focus and cognitive function. For instance, the scent of freshly baked bread might trigger memories of home and comfort, evoking a positive emotional response.
Comparison of Smells and Their Effects on Wellbeing
| Smell Type | Potential Effect on Wellbeing | Examples |
|---|---|---|
| Floral (lavender, rose) | Calming, relaxing, stress-reducing | Lavender essential oil diffusers, rose-scented candles |
| Citrus (lemon, orange) | Uplifting, energizing, mood-boosting | Lemon-scented cleaning products, orange blossom water |
| Woody (sandalwood, cedarwood) | Grounding, calming, promoting focus | Incense sticks, cedarwood essential oil |
| Earthy (earthy, wet soil) | Calming, grounding, connected to nature | Nature-inspired scents, soil-based aromatherapy products |
| Spicy (cinnamon, cloves) | Potentially uplifting, depending on individual preferences | Cinnamon-scented candles, spiced pumpkin latte |
Utilizing Smell to Enhance Daily Life
The power of smell to influence mood and wellbeing can be effectively utilized in daily life. Consider incorporating pleasant scents into your routine to improve your overall experience. Aromatherapy techniques, using essential oils, can be integrated into daily routines to promote relaxation and stress reduction. Furthermore, the selection of scented products (candles, room sprays) can create a comforting and uplifting atmosphere in your home or workspace.
Incorporate pleasant scents into your daily routine to elevate your mood and create a more positive and calming environment.
Last Recap
In conclusion, smell and brain health share a profound relationship, influencing everything from our memories to our moods and cognitive functions. The intricate connection between the olfactory system and the brain reveals a remarkable interplay that extends far beyond simple sensory perception. From the impact of aging and environmental factors to the potential for smell training and aromatherapy, this exploration underscores the importance of appreciating our sense of smell and its vital role in maintaining optimal brain health.