Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being.
Understanding the specific needs of those living with ankylosing spondylitis is paramount. This comprehensive guide will empower you with the knowledge and tools to develop a tailored exercise plan that prioritizes your individual needs and goals, promoting both physical and mental well-being.
Ankylosing Spondylitis: Understanding the Condition and Management
Ankylosing spondylitis (AS) is a chronic inflammatory condition primarily affecting the spine and sacroiliac joints. Characterized by inflammation and stiffness, AS can lead to significant pain and reduced mobility over time. Understanding the nature of this disease, its progression, and the crucial role of exercise is vital for effective management.
Finding the right exercises for ankylosing spondylitis can be tricky, but incorporating regular walking into your routine is a fantastic way to start. Studies show that physical activity, like walking, can significantly reduce symptoms and improve overall well-being. This is especially important since walking cuts depression risk , a key factor for managing the emotional aspects of this condition.
So, as you explore different exercises for ankylosing spondylitis, remember that simple activities like walking can have a powerful impact.
Defining Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis that primarily targets the spine and sacroiliac joints. Inflammation in these areas causes pain, stiffness, and, over time, fusion of the vertebrae. This fusion, or ankylosis, can restrict movement and posture, impacting daily activities.
Common Symptoms of Ankylosing Spondylitis
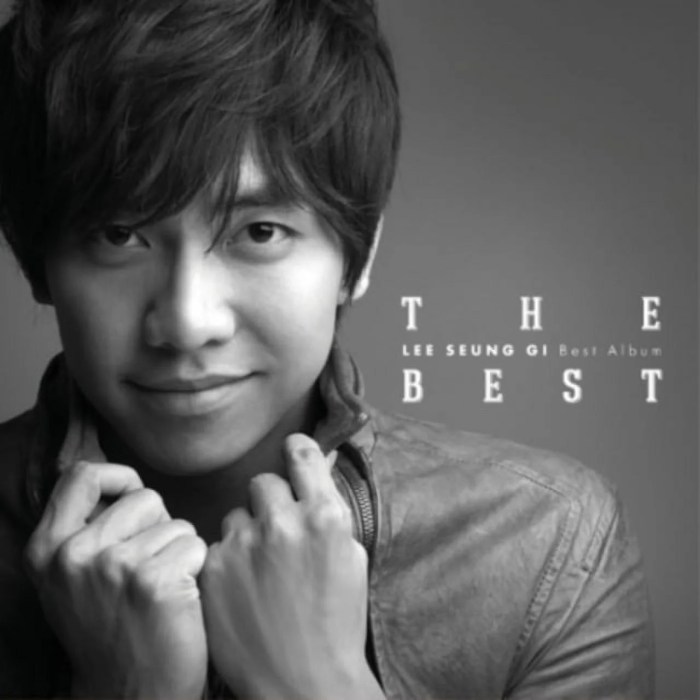
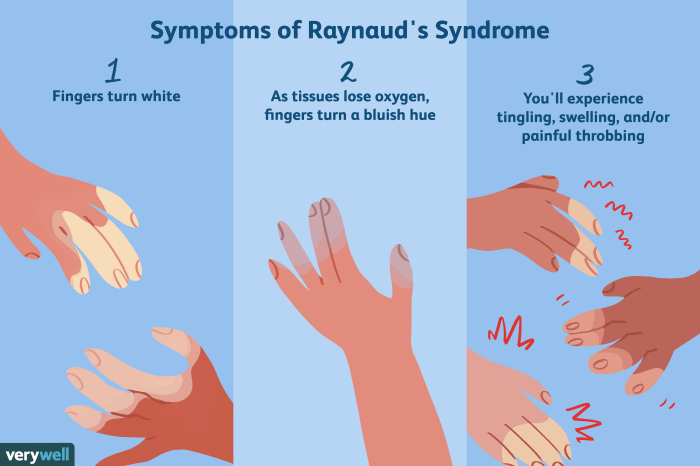
Symptoms of AS often begin subtly, making early diagnosis challenging. Common symptoms include:
- Low back pain, typically starting insidiously and worsening over time.
- Stiffness, particularly in the morning or after periods of inactivity.
- Pain and stiffness in the sacroiliac joints, located at the base of the spine.
- Limited range of motion in the spine, affecting flexibility and posture.
- Pain and stiffness in the hips, shoulders, and other joints in more advanced stages.
These symptoms can vary significantly in severity from person to person, and some individuals may experience more severe symptoms than others.
Typical Progression of Ankylosing Spondylitis
The progression of AS is highly variable. Some individuals experience a gradual increase in symptoms over many years, while others may experience a more rapid progression. Early intervention and appropriate management strategies can significantly slow the progression of the disease.
- Early stages often feature intermittent pain and stiffness, particularly in the morning.
- As the disease progresses, pain and stiffness become more persistent and widespread.
- Over time, the inflammation can lead to fusion of the vertebrae, resulting in reduced spinal mobility and posture changes.
It’s crucial to recognize that the progression is not uniform, and individual experiences vary greatly.
The Role of Exercise in Managing Ankylosing Spondylitis
Regular exercise plays a vital role in managing AS, helping to maintain joint mobility, improve flexibility, and reduce pain. A carefully designed exercise program can help individuals maintain a healthy lifestyle and manage the condition effectively.
- Maintaining a consistent exercise routine can help strengthen muscles supporting the spine and improve posture.
- Aerobic exercise can help improve cardiovascular health and overall well-being.
- Flexibility exercises are essential to maintain spinal mobility and prevent stiffness.
The Importance of Personalized Exercise Programs
Given the diverse range of symptoms and responses to treatment in individuals with AS, personalized exercise programs are crucial. Generic exercise routines may not be effective or safe for everyone.
- A healthcare professional, such as a physical therapist specializing in AS, should develop a personalized exercise plan tailored to the individual’s specific needs and abilities.
- The plan should consider the individual’s pain levels, current physical limitations, and overall health.
- Regular monitoring and adjustments to the program are essential to ensure its effectiveness and safety.
This personalized approach ensures that exercise is both beneficial and safe for each individual with AS.
Types of Exercises for Ankylosing Spondylitis
Finding the right exercise routine is crucial for managing ankylosing spondylitis (AS). Consistent physical activity can significantly improve flexibility, strength, and overall well-being, helping to alleviate pain and stiffness. Understanding the different types of exercises and their suitability for various stages of the disease is key to creating a personalized and effective management plan.Understanding the specific types of exercises tailored for AS is essential for developing a comprehensive management strategy.
This approach involves targeting areas affected by the condition, considering the varying stages of the disease, and emphasizing low-impact activities to minimize stress on the joints.
Exercise Types Suitable for Ankylosing Spondylitis
A structured exercise program should be tailored to individual needs and disease progression. Choosing appropriate exercises can significantly improve quality of life for those with AS.
| Exercise Type | Description | Benefits | Precautions |
|---|---|---|---|
| Gentle Stretching | Involves slow, controlled movements to increase flexibility and range of motion in the spine and surrounding joints. | Improves posture, reduces stiffness, and enhances overall mobility. | Avoid sudden or forceful movements. Listen to your body and stop if you feel sharp pain. |
| Aerobic Exercise (Low-Impact) | Activities like walking, swimming, cycling, or using an elliptical trainer. | Improves cardiovascular health, strengthens muscles, and boosts endurance. | Choose activities that do not put excessive stress on the spine. Start slowly and gradually increase intensity. |
| Strengthening Exercises | Focuses on building core and back strength to support the spine and reduce pain. These can include exercises like planks, bridges, and seated rows. | Improves posture, stability, and overall strength. | Avoid exercises that cause significant pain or discomfort. Use proper form to prevent injury. |
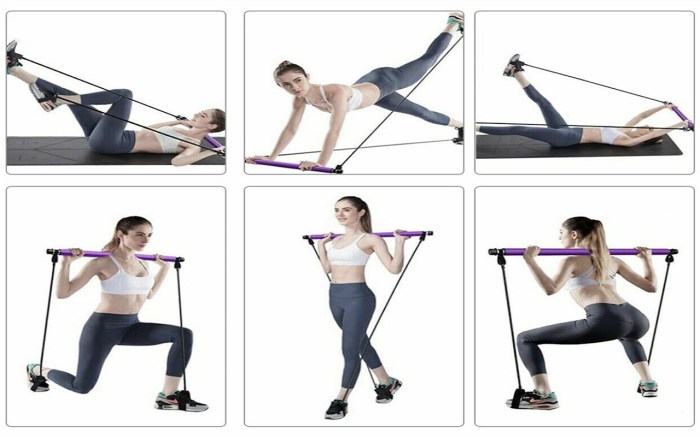
| Yoga and Pilates | Gentle movements and postures that improve flexibility, balance, and core strength. | Enhances spinal mobility, improves posture, and promotes relaxation. | Adapt poses to accommodate individual needs and limitations. Avoid poses that cause excessive stress on the spine. |
| Tai Chi | A series of slow, flowing movements that enhance balance, flexibility, and mindfulness. | Improves posture, balance, and reduces stress. | Beginners should start with simpler forms and gradually increase complexity. |
Targeting Specific Areas Affected by AS
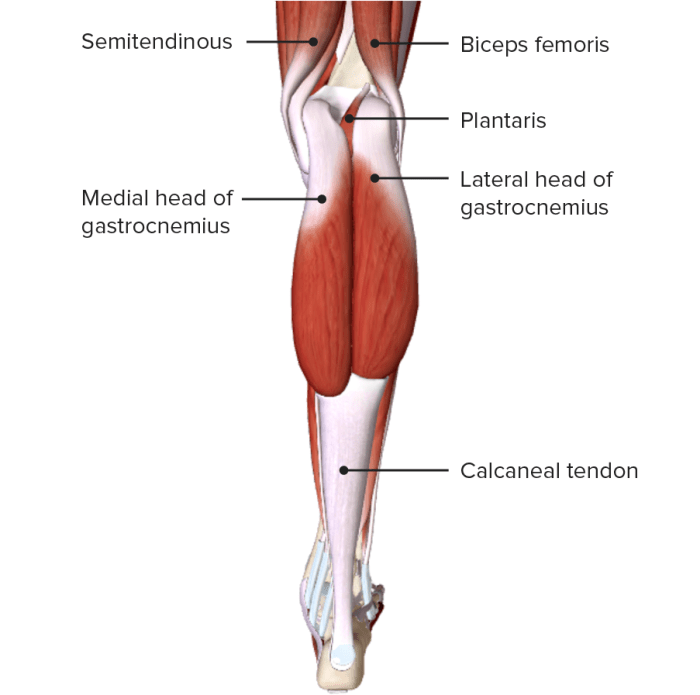
Specific exercises can be focused on areas commonly affected by AS, such as the spine, hips, and shoulders. Exercises that target these regions can help to maintain flexibility and strength. Gentle spinal stretches, hip openers, and shoulder rotations can help maintain a healthy range of motion.
Staying active is crucial for managing ankylosing spondylitis, and specific exercises can really help. But sometimes, alongside the physical discomfort, you might experience a migraine without aura – a debilitating headache type. Understanding what a migraine without aura is can be helpful in connecting potential symptoms and figuring out the best approach to managing your overall health, especially when considering exercises for ankylosing spondylitis, like gentle stretching and swimming, which can be very beneficial for pain relief.
Finding the right balance between exercise and managing potential health complications is key. what is a migraine without aura A good physical therapist can guide you on the best exercise program for your needs.
Comparing Exercise Modalities
Different exercise modalities can offer varying levels of benefit in managing AS. For instance, low-impact aerobic exercises, like swimming, can improve cardiovascular health without putting excessive stress on the spine. Strengthening exercises, on the other hand, help to build muscle support around the spine, which can reduce pain and improve stability. Yoga and Pilates routines offer a holistic approach by combining stretching, strengthening, and mindfulness practices.
Importance of Low-Impact Exercises
Low-impact exercises are particularly important for individuals with AS due to the potential for joint inflammation and pain. Activities like swimming, walking, and cycling put less stress on the spine and joints, allowing for continued participation without exacerbating existing symptoms.
Examples of Exercises for Different Stages
The choice of exercises should be adapted to the individual’s stage of AS. For example, in the early stages, gentle stretching and low-impact aerobics can be beneficial to maintain flexibility and overall health. As the disease progresses, a more tailored approach involving strengthening exercises, yoga, or Pilates might be needed to address specific areas of weakness or pain.
Exercise Routines and Programs
Finding the right exercise routine is crucial for managing ankylosing spondylitis (AS). Consistency and appropriate progression are key to achieving pain relief, maintaining mobility, and improving overall well-being. This section Artikels sample routines for different fitness levels, emphasizing modifications and progressions to ensure safety and effectiveness.Understanding your current fitness level and any specific limitations is vital before starting any new exercise program.
Consult with your healthcare provider or a physical therapist to tailor a program that aligns with your individual needs and goals. Remember, listen to your body and adjust the routines as necessary.
Finding the right exercises for ankylosing spondylitis can be tricky, but consistency is key. It’s fascinating how our bodies work, and while the genetics of eye color genetics of eye color are influenced by similar complex biological factors, the physical impact of these exercises on spinal mobility is the crucial focus for those with this condition. Ultimately, tailored exercises are essential for managing the symptoms and improving overall well-being.
Beginner Exercise Routine
This routine focuses on building a foundation of movement and flexibility, gradually introducing core strengthening exercises.
- Warm-up (5-10 minutes): Gentle cardiovascular activities like walking, arm circles, and leg swings. This prepares the body for more strenuous activity and reduces the risk of injury.
- Core Exercises (10-15 minutes): Plank variations (on knees or forearms), bird-dog exercises, and pelvic tilts. These exercises strengthen the core muscles, which are essential for posture and spinal stability.
- Stretching (15-20 minutes): Focus on spinal stretches like spinal twists, forward folds, and gentle back extensions. Hold each stretch for 20-30 seconds, emphasizing controlled movements. Avoid bouncing or forcing the stretch.
- Cool-down (5-10 minutes): Slow down the cardiovascular activity, returning to gentle movements like walking and deep breathing. This helps the body recover and reduces muscle soreness.
Intermediate Exercise Program
This routine builds upon the beginner’s program, incorporating more challenging exercises and modifications for increasing intensity and range of motion.
- Warm-up (10-15 minutes): Increase the intensity of the warm-up, potentially adding light jogging or cycling. This will help prepare the body for more advanced exercises.
- Core Exercises (15-20 minutes): Introduce advanced plank variations, Russian twists, and bicycle crunches. Gradually increase the duration and repetitions of each exercise.
- Stretching (20-25 minutes): Incorporate more dynamic stretches, such as arm swings and leg swings, to improve flexibility and range of motion. Hold static stretches for 30-60 seconds.
- Cool-down (10-15 minutes): Continue with gentle cardiovascular activity and static stretches to aid in muscle recovery and reduce the risk of post-exercise stiffness.
Advanced Exercise Program
This routine is designed for individuals with a higher fitness level, incorporating more challenging exercises and specific modifications for potential issues.
- Warm-up (15-20 minutes): Include activities like jumping jacks, high knees, and butt kicks. This prepares the body for more intense exercise.
- Core Exercises (20-30 minutes): Perform advanced exercises such as weighted planks, medicine ball slams, and hanging leg raises. These exercises target core strength and stability.
- Stretching (25-30 minutes): Include yoga poses that target specific areas of stiffness or pain. Focus on holding stretches for a longer duration (60-90 seconds).
- Cool-down (15-20 minutes): Engage in activities like walking and gentle stretching, emphasizing relaxation and recovery.
Incorporating Flexibility Exercises into Daily Routines
Regular flexibility exercises are essential for managing AS. Incorporate stretches into your daily routine, even if it’s just for a few minutes.
- Chair Stretches: Simple stretches can be performed while sitting in a chair. Forward bends, side stretches, and shoulder rolls can be incorporated throughout the day.
- Standing Stretches: Standing stretches, like torso twists and leg stretches, can be done during work breaks or while waiting in line.
- Activities to Adapt: Activities like swimming, walking, and cycling can be adapted for use in exercise programs. Consult with your physical therapist for suitable modifications.
Exercise Considerations for Specific Needs
Adjusting exercise routines for ankylosing spondylitis (AS) requires careful consideration of individual needs. Different levels of mobility, pain sensitivities, and flare-ups necessitate modifications to maintain progress and prevent setbacks. Understanding these factors allows for personalized programs that support both physical and emotional well-being.Tailoring exercises to specific needs is crucial for optimal results and injury prevention. This involves adjusting intensity, duration, and type of exercise based on individual capabilities and limitations.
Understanding how to modify exercises for different needs ensures that the exercises remain beneficial and safe.
Modifying Exercises for Varying Mobility and Flexibility
Individual differences in mobility and flexibility are significant factors in exercise design. Those with limited range of motion need modifications to avoid strain and potential injury. For example, instead of full forward bends, partial bends or stretches against a wall or with a chair can be used to maintain flexibility without excessive stress. Gentle, controlled movements are paramount.
Progressive increases in range of motion are essential but must be gradual to prevent setbacks.
Managing Pain During Exercise Sessions
Pain management is crucial during exercise sessions. Listen to your body; stop if pain increases significantly. Using heat packs or ice before and after exercise can help reduce pain and inflammation. Employing pain-relieving medication as prescribed by a healthcare professional can also be helpful. Proper warm-up and cool-down routines are essential to prevent sudden pain spikes.
Adjusting Exercise Routines Based on Flare-ups or Exacerbations
Flare-ups and exacerbations are common in AS. During these periods, it’s essential to modify or temporarily suspend exercise routines. Listen to your body, and reduce the intensity, duration, or type of exercise. Rest and gentle stretching, like gentle range of motion exercises, may be more appropriate. Consult with a healthcare professional to determine the best course of action.
Consider incorporating activities that can help manage stress, such as meditation or relaxation techniques, to support overall well-being during flare-ups.
Preventing Injuries During Exercise
Injury prevention is paramount in an exercise program for AS. Warm-up adequately before any exercise session. Proper form is critical; avoid pushing yourself beyond your limits. Using supportive equipment, such as a chair or wall for balance, can be helpful for exercises requiring stability. Listen to your body and avoid pushing through pain.
Cool down thoroughly after each session to aid in muscle recovery.
The Role of Rest and Recovery in Exercise Programs, Exercises for ankylosing spondylitis
Rest and recovery are just as important as exercise itself. Adequate rest allows the body to repair and rebuild tissues, promoting overall health and well-being. Establish a regular sleep schedule, ensuring sufficient sleep. Include rest days into your exercise routine to avoid overexertion. Pay attention to signs of fatigue and adjust accordingly.
Listen to your body’s signals and prioritize rest when needed. Adequate rest, along with proper nutrition, aids in faster recovery and reduces the risk of injury.
Exercise and Lifestyle Integration
Embarking on an exercise program for ankylosing spondylitis (AS) is a crucial step toward managing the condition effectively. However, exercise alone isn’t sufficient. Integrating a healthy lifestyle alongside your exercise routine is paramount for long-term well-being and symptom control. This approach fosters a holistic approach to managing AS, recognizing the intricate connection between physical activity, nutrition, and overall health.Maintaining a consistent exercise routine is vital for managing AS symptoms.
However, it’s equally important to create a lifestyle that complements and supports this routine. This holistic approach recognizes that AS isn’t just a physical condition but one that impacts various aspects of daily life, requiring a multi-faceted approach to effective management.
Strategies for Integrating Exercise into Daily Routines
Successful exercise integration hinges on consistency and practicality. Finding activities you enjoy and can incorporate seamlessly into your daily schedule is key. This may involve scheduling exercise blocks, incorporating physical activity into your commute, or finding ways to be more active throughout the day. Small, consistent efforts add up over time, leading to significant improvements in overall health and well-being.
Scheduling exercise blocks in your daily planner and viewing them as appointments helps establish routine.
Importance of Maintaining a Healthy Lifestyle Alongside Exercise Programs
A healthy lifestyle, encompassing proper nutrition, adequate sleep, and stress management, is essential for optimizing the benefits of exercise programs. Nutrition provides the fuel for your body to recover and repair, while adequate sleep allows for muscle repair and overall restoration. Stress management techniques, such as meditation or yoga, can help reduce inflammation and promote a sense of calm, which can significantly impact AS symptoms.
Relationship Between Exercise, Nutrition, and Managing Ankylosing Spondylitis
Nutrition plays a significant role in managing AS. A balanced diet rich in fruits, vegetables, and whole grains can help reduce inflammation and provide essential nutrients for optimal health. Avoiding processed foods, sugary drinks, and excessive saturated fats is crucial for reducing potential inflammatory triggers. The right nutrition fuels your body to recover and adapt to the demands of exercise, further enhancing your overall health and well-being.
Role of Support Groups and Physical Therapists in Exercise Programs
Support groups provide a valuable network of individuals who understand the challenges of living with AS. Sharing experiences, advice, and encouragement with others facing similar conditions can be empowering and motivating. Physical therapists are crucial in developing tailored exercise programs and providing guidance on proper form and technique. They can assess individual needs and create personalized routines, minimizing the risk of injury and maximizing the effectiveness of exercise.
Lifestyle Factors Affecting Ankylosing Spondylitis and Recommendations
| Lifestyle Factor | Impact on AS | Recommendations | Examples |
|---|---|---|---|
| Nutrition | Poor nutrition can exacerbate inflammation and reduce energy levels, negatively impacting exercise adherence and overall well-being. | Focus on a balanced diet rich in fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and excessive saturated fats. | Include fruits and vegetables in every meal, choose lean protein sources, and opt for whole-grain breads and cereals. |
| Sleep | Adequate sleep is crucial for muscle repair and recovery, reducing inflammation, and improving overall mood. Insufficient sleep can worsen fatigue and increase pain. | Aim for 7-9 hours of quality sleep per night. Establish a regular sleep schedule and create a relaxing bedtime routine. | Create a calming bedtime routine, ensure your bedroom is dark and quiet, and avoid screens before bed. |
| Stress Management | Stress can exacerbate inflammation and pain, making it harder to adhere to an exercise program. | Incorporate stress-reducing activities such as yoga, meditation, or spending time in nature. | Practice deep breathing exercises, engage in hobbies, or spend time in nature to promote relaxation. |
| Hydration | Proper hydration is vital for joint health and overall function. Dehydration can worsen pain and stiffness. | Drink plenty of water throughout the day, and adjust intake based on activity levels. | Carry a water bottle and sip on water regularly throughout the day. |
Exercise for Specific Body Parts
Staying active is crucial for managing Ankylosing Spondylitis, and targeted exercises for specific body parts can significantly improve your quality of life. This section delves into exercises designed to enhance spinal mobility, strengthen core muscles, improve shoulder and hip flexibility, and build overall body strength and endurance. Proper form and safety are paramount, so follow the instructions carefully.Effective exercise programs for Ankylosing Spondylitis require a tailored approach.
Understanding how to exercise specific body parts safely and effectively is key to managing pain and stiffness while building strength and improving overall function.
Improving Spinal Mobility and Flexibility
Maintaining spinal mobility is essential for preventing stiffness and pain associated with Ankylosing Spondylitis. Gentle stretching and specific exercises can help improve flexibility and range of motion.
- Cat-Cow Pose: Begin on your hands and knees. Inhale, arch your back like a cow, dropping your belly towards the floor, and tilting your head back. Exhale, round your spine like a cat, tucking your chin towards your chest. Repeat 10-15 times. This exercise gently mobilizes the spine and improves spinal extension and flexion.
- Spinal Rotations: Sit or stand tall. Slowly rotate your torso from side to side, keeping your core engaged and maintaining a controlled movement. Repeat 10-15 times per side. This helps increase spinal rotation and flexibility.
- Knee-to-Chest Stretches: Lie on your back. Gently pull one knee towards your chest, holding for 20-30 seconds. Repeat with the other leg. This stretches the hamstrings and lower back, enhancing flexibility in the lumbar spine.
Strengthening Core Muscles
A strong core provides stability and support for the spine, helping to reduce pain and improve posture.
- Plank: Hold a plank position, supporting your body weight on your forearms and toes. Maintain a straight line from head to heels. Hold for 15-30 seconds, gradually increasing the duration as your strength improves. This strengthens the core, including the abdominal muscles, back muscles, and shoulders.
- Bird Dog: Start on your hands and knees. Extend one arm forward and the opposite leg backward, keeping your body in a straight line. Hold for a few seconds, then return to the starting position and repeat with the other arm and leg. Repeat 10-15 times per side. This strengthens the deep core muscles and stabilizes the spine.
- Crunches: Lie on your back with knees bent and feet flat on the floor. Engage your core and slowly lift your head and shoulders off the floor. Lower yourself back down slowly. Repeat 10-15 times. This targets the abdominal muscles and helps improve core strength.
Targeting Shoulder and Hip Flexibility
Maintaining flexibility in the shoulders and hips is crucial for overall body movement and reducing pain.
- Shoulder Stretches: Reach one arm across your body, using your opposite hand to gently pull on your extended arm. Hold for 20-30 seconds. Repeat with the other arm. This improves shoulder mobility and reduces tightness.
- Hip Flexor Stretches: Stand with one leg forward and the other leg back. Bend your front knee and keep your back knee on the floor. Hold for 20-30 seconds. Repeat with the other leg. This targets the hip flexors, important for maintaining mobility.
- Figure-Four Stretch: Lie on your back. Cross one ankle over the opposite knee and gently pull on the bent knee towards your chest. Hold for 20-30 seconds. Repeat with the other leg. This stretches the hips and glutes, enhancing flexibility and reducing stiffness.
Improving Overall Body Strength and Endurance
Building overall body strength and endurance can significantly improve your ability to manage daily activities and reduce fatigue.
- Wall Push-Ups: Stand facing a wall with your hands shoulder-width apart on the wall. Slowly move your body towards the wall, bending your elbows until your chest nearly touches the wall. Push yourself back to the starting position. Repeat 10-15 times. This exercise builds upper body strength and endurance.
- Walking: A simple yet effective exercise. Start with short walks and gradually increase the duration and distance as tolerated. Walking improves cardiovascular health and strengthens leg muscles.
- Swimming: A low-impact exercise that can improve cardiovascular health and build overall body strength. Consult with your physician before starting a swimming program.
Exercise and Medications

Understanding how exercise interacts with medications for ankylosing spondylitis (AS) is crucial for optimizing treatment and managing the condition effectively. This interplay can significantly impact the effectiveness of medications and requires careful consideration. Properly managing exercise routines in conjunction with medication regimens is vital for overall well-being and symptom control.Medication adherence and exercise are both essential components of an AS management plan.
However, the effects of exercise on medication efficacy, and vice-versa, are not always straightforward. Careful monitoring and adjustments are often necessary to ensure the best possible outcomes.
Impact of Exercise on Medication Effectiveness
Exercise can influence the effectiveness of medications for AS by enhancing their absorption, distribution, or metabolism. Certain medications might be more effective when coupled with specific exercise routines, potentially leading to reduced inflammation and improved mobility. Conversely, some exercises might interact negatively with medication, potentially increasing side effects or diminishing the therapeutic benefits.
Medication Interactions with Exercise
Specific medications used for AS can have various side effects that impact exercise routines. For instance, some medications might cause fatigue, muscle weakness, or gastrointestinal issues, which could limit the intensity or duration of exercise sessions. Careful consideration of these potential interactions is crucial for tailoring exercise programs.
Adjusting Exercise Routines Based on Medication Side Effects
Medication side effects can significantly impact exercise routines. For example, if a medication causes fatigue, exercise sessions should be shorter and less intense. If a medication causes gastrointestinal distress, adjustments to the timing of exercise in relation to meals might be needed. It is also essential to modify the intensity and type of exercise based on the individual’s tolerance and experience.
Successful Exercise Programs Implemented by Individuals on Medication
Several individuals with AS have successfully implemented exercise programs while on medication. A common example is a patient who initially experienced increased fatigue with a specific medication. They adjusted their routine by exercising at lower intensities and shorter durations. They also prioritized rest days to manage fatigue effectively. This led to sustained adherence to the exercise program and improved overall well-being.
Another example might be a patient who found that morning exercise helped to minimize gastrointestinal discomfort caused by their medication.
Tips for Communication with Healthcare Professionals Regarding Exercise Routines
Open communication with healthcare professionals is essential when managing exercise routines alongside medication. Patients should inform their doctors about any changes to their exercise program, any new or worsening side effects, and any adjustments they make to their medication dosage. This allows healthcare professionals to monitor the impact of exercise on medication effectiveness and provide personalized guidance. This collaborative approach helps optimize the management of AS.
Exercise and Preventing Complications: Exercises For Ankylosing Spondylitis
Staying active is crucial for managing ankylosing spondylitis (AS). Beyond improving flexibility and range of motion, regular exercise plays a vital role in preventing potential complications associated with the condition. A proactive approach to exercise can significantly enhance the quality of life for individuals living with AS.Exercise, when appropriately tailored, can mitigate the risk of various complications arising from AS, including osteoporosis, cardiovascular issues, and spinal deformities.
Understanding the interplay between exercise and these potential complications is essential for developing a comprehensive management strategy.
Potential Complications of Ankylosing Spondylitis and Exercise Mitigation
AS can lead to a range of complications. These complications can significantly impact quality of life, making preventative measures through exercise crucial. Regular exercise can help in reducing the severity of these complications.
- Osteoporosis: A common complication of AS, osteoporosis is characterized by reduced bone density, increasing the risk of fractures. Weight-bearing exercises, such as walking, jogging, and stair climbing, stimulate bone formation, helping to maintain bone density and reducing the risk of fractures. Resistance training, using weights or resistance bands, also strengthens bones, further enhancing bone health.
- Cardiovascular Issues: AS can increase the risk of cardiovascular problems. Aerobic exercises, such as swimming, cycling, and brisk walking, improve cardiovascular fitness, reducing the risk of heart disease, stroke, and high blood pressure. Consistent cardiovascular activity helps maintain a healthy heart and circulation, mitigating potential cardiovascular complications.
- Spinal Deformities: Over time, AS can lead to spinal deformities, potentially causing pain and mobility issues. Specific exercises, such as stretching and core strengthening, can help maintain spinal alignment and flexibility, reducing the risk of developing these deformities. Regular movement helps to counteract the effects of stiffness and maintain a healthy range of motion.
Reducing the Risk of Osteoporosis Through Exercise
Maintaining bone density is essential for preventing fractures and other complications related to osteoporosis. Exercise plays a key role in this process.Weight-bearing exercises are particularly effective in stimulating bone growth and increasing bone density. Examples include brisk walking, jogging, stair climbing, and dancing. These activities force the bones to work against gravity, encouraging bone formation. Resistance training, utilizing weights or resistance bands, also strengthens bones, further enhancing bone health.
A balanced diet rich in calcium and vitamin D, coupled with regular exercise, creates a comprehensive strategy for bone health.
Exercise and Cardiovascular Health
Cardiovascular health is vital for overall well-being, and AS patients need to be particularly mindful of their cardiovascular health. Exercise plays a crucial role in maintaining healthy cardiovascular function.Aerobic exercises, such as swimming, cycling, and brisk walking, significantly improve cardiovascular fitness. These activities strengthen the heart muscle, improve blood circulation, and help regulate blood pressure. Consistent cardiovascular activity helps maintain a healthy heart and circulation, reducing the risk of heart disease, stroke, and high blood pressure.
Monitoring heart rate during exercise and adjusting intensity as needed is vital to prevent strain on the heart.
Preventing Spinal Deformities Through Exercise
Maintaining spinal health is crucial in managing AS. Regular exercise can significantly contribute to preventing spinal deformities.Specific exercises focused on stretching and core strengthening are vital in maintaining spinal alignment and flexibility. These exercises help to counteract the stiffness associated with AS and maintain a healthy range of motion. Yoga, Pilates, and tai chi are examples of exercises that can help improve flexibility and core strength, contributing to spinal health.
By maintaining flexibility and strength, spinal deformities can be prevented or mitigated.
Monitoring Exercise Intensity and Duration
Proper monitoring of exercise intensity and duration is essential for preventing injuries and maximizing the benefits of exercise.
It is crucial to start slowly and gradually increase the intensity and duration of exercises over time.
Listening to the body’s signals is paramount. Rest and recovery are equally important as exercise. Consult with a healthcare professional or physical therapist to develop a personalized exercise plan that is appropriate for individual needs and fitness levels. Regular monitoring allows for adjustments to the exercise plan, ensuring safety and effectiveness. Overexertion can be detrimental and should be avoided.
Final Wrap-Up
In conclusion, managing ankylosing spondylitis through exercise is a personalized journey. By understanding the different types of exercises, creating suitable routines, and integrating them into a healthy lifestyle, you can effectively manage symptoms, improve your quality of life, and prevent complications. Remember that consistency, proper form, and listening to your body are key. This guide serves as a valuable resource, but always consult your healthcare provider for personalized advice.