Leg cramps at night can be incredibly disruptive, jolting you awake with sudden, sharp pain. This post dives deep into understanding these nocturnal muscle spasms, exploring the possible causes, risk factors, and effective home remedies. We’ll also look at when it’s time to seek medical attention for persistent or severe leg cramps. Night leg cramps…
Coping When Loved One Doesnt Recognize You
Coping when loved one doesnt recognize you – Coping when a loved one doesn’t recognize you is a deeply challenging experience, filled with a spectrum of emotions and complex situations. This journey explores the emotional toll of such a situation, from the initial shock and confusion to the potential long-term impact on the relationship. We’ll…
Does Watermelon Trigger Migraines? A Deep Dive
Does watermelon trigger migraines? This intriguing question delves into the potential connection between this refreshing summer fruit and the debilitating headaches of migraines. We’ll explore the nutritional profile of watermelon, the characteristics of migraines, and the scientific understanding of food-related triggers, examining potential mechanisms and individual sensitivities. The discussion will also touch upon how watermelon…
Biotin for Hair Growth A Deep Dive
Biotin for hair growth is a topic of considerable interest, and for good reason. This exploration delves into the fascinating world of biotin, examining its role in supporting not only healthy hair but also overall bodily functions. We’ll uncover the science behind biotin’s impact on hair follicle health, analyze supplementation strategies, and explore factors that…
Type 2 Diabetes in Black and Brown People A Deep Dive
Type 2 diabetes in black and brown people is a critical health issue demanding attention. This exploration delves into the significant prevalence rates and the unique risk factors impacting these communities. We’ll examine the challenges in diagnosis, the need for culturally appropriate management strategies, and the role of social determinants of health in shaping these…
Niacin Overdose Risks Explained
Risks of too much niacin can be serious, affecting your health in various ways. Understanding the potential dangers of excessive niacin intake is crucial for maintaining optimal well-being. This comprehensive guide delves into the various forms of niacin, its role in the body, and the risks associated with consuming too much. We’ll explore potential symptoms,…
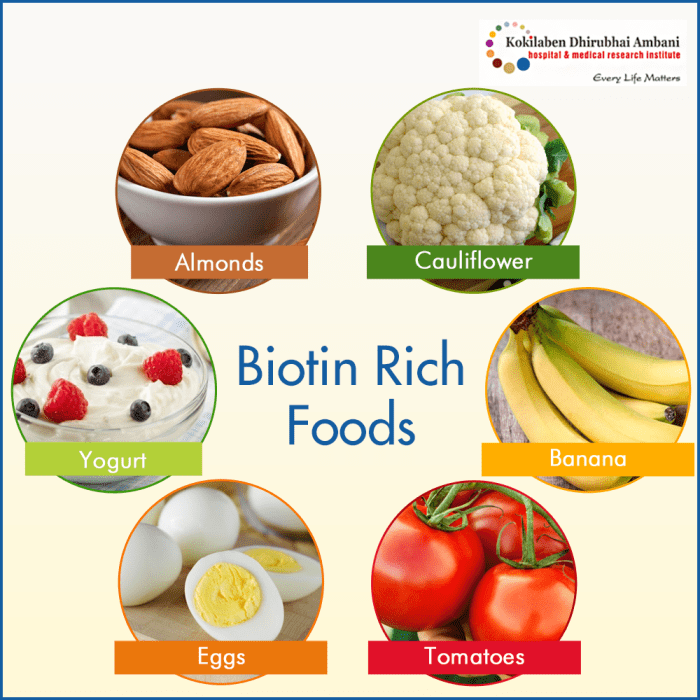
Eye Injections for AMD A Comprehensive Guide
Eye injections for AMD offer a potential lifeline for those struggling with age-related macular degeneration. This guide delves into the intricacies of these treatments, exploring the different types of AMD, the medications used in eye injections, and the procedures involved. We’ll also discuss the potential benefits, risks, and post-injection care. Understanding the specifics of eye…
Purified vs Distilled Water A Deep Dive
Purified vs distilled water is a common topic of debate, especially for those concerned about the quality of their drinking water. This in-depth look will explore the differences between these two types of water, examining their purification methods, chemical composition, health implications, applications, cost, environmental impact, and more. We’ll delve into the science behind each…
What is Palliative Care A Comprehensive Guide
What is palliative care? It’s a specialized approach to care that focuses on improving the quality of life for people facing serious illnesses. Unlike curative care, which aims to cure disease, palliative care aims to provide comfort and support, both for the patient and their loved ones. This comprehensive guide explores the various aspects of…
Should You Put Mouthwash in Your Water Flosser?
Should you put mouthwash in your water flosser? This intriguing question sparks a fascinating debate about enhancing oral hygiene. Adding mouthwash to your water flosser might seem like a logical next step, but is it actually beneficial, or could it introduce unwanted complications? Let’s dive deep into the potential benefits, risks, and practical considerations of…