Menopause and joint pain often go hand-in-hand, creating a complex interplay of symptoms and underlying mechanisms. This exploration delves into the physiological changes during menopause that can affect joints, examining the types of pain experienced, and exploring the connection between hormonal fluctuations and discomfort. We’ll also look at diagnosis, treatment strategies, and crucial lifestyle recommendations to navigate this challenging period.
Understanding the link between fluctuating hormones and joint health is key to managing this common experience. We’ll cover the biological mechanisms behind the pain, the role of estrogen, and potential inflammatory processes. Different types of joint pain and their unique characteristics will be discussed, along with how they compare to other conditions like osteoarthritis. This will help you recognize the specific symptoms you may be experiencing.
Overview of Menopause and Joint Pain
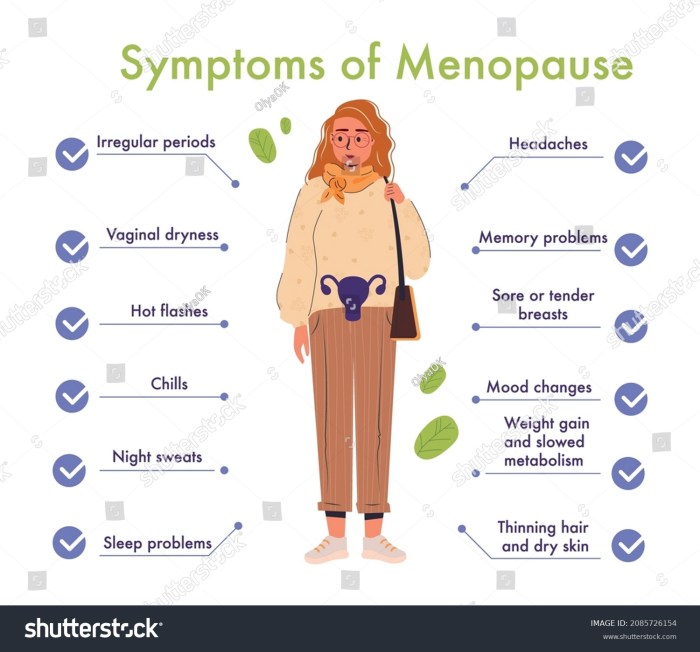
Menopause, a natural biological process marking the end of a woman’s reproductive years, brings about significant changes in the body. These changes can manifest in various ways, including joint pain, which often accompanies the hormonal shifts associated with this transition. Understanding the relationship between menopause and joint pain is crucial for managing symptoms and improving overall well-being.The physiological changes during menopause, primarily the decline in estrogen levels, play a pivotal role in the development of joint pain.
Estrogen is crucial for maintaining bone density and joint health. Decreased estrogen levels can lead to increased bone loss (osteoporosis), making bones more fragile and susceptible to fractures. This, in turn, can lead to joint pain and stiffness. Furthermore, the hormonal fluctuations can affect the production of synovial fluid, the lubricating fluid in joints. Reduced synovial fluid can lead to decreased joint mobility and increased friction, contributing to discomfort and pain.
Physiological Changes and Their Impact on Joints
The decline in estrogen levels during menopause directly impacts bone density and joint health. Estrogen plays a vital role in maintaining healthy bones, and its decrease can lead to increased bone loss. This bone loss makes the bones more fragile and prone to fractures, leading to pain and stiffness in joints. The decreased production of synovial fluid, the lubricating fluid in joints, further contributes to discomfort.
Reduced lubrication can cause increased friction between joint surfaces, exacerbating pain and limiting movement. These hormonal shifts can also influence the inflammatory response in the body, potentially contributing to joint pain.
Menopause and joint pain can be a real drag, impacting everything from simple movements to overall comfort. Sometimes, the discomfort extends beyond the joints, manifesting as a paronychia infection around the nails, a tricky issue that can add to the woes of those experiencing menopause and joint pain. It’s a good idea to keep an eye on these related symptoms to better understand your body’s responses during this phase.
Common Types of Joint Pain Experienced During Menopause
Women experiencing menopause may encounter various types of joint pain. Common forms include aching, stiffness, and soreness, often felt in the hips, knees, and hands. These sensations can range from mild discomfort to severe pain, impacting daily activities and quality of life. Pain may also manifest as a feeling of warmth or swelling around the affected joints.
Relationship Between Hormonal Fluctuations and Joint Discomfort
The fluctuating levels of hormones, particularly estrogen, directly correlate with the experience of joint discomfort during menopause. As estrogen levels decrease, the body’s ability to maintain healthy bones and joints is compromised. This results in increased bone loss, reduced synovial fluid production, and potential inflammatory responses, all contributing to joint pain and stiffness.
Comparison of Menopause and Joint Pain Symptoms
| Menopause Symptom | Description | Joint Pain Symptom | Description |
|---|---|---|---|
| Hot flashes | Sudden sensations of warmth, often accompanied by sweating, typically affecting the upper body. | Stiffness | A feeling of tightness or immobility in the joints, often experienced in the morning or after periods of inactivity. |
| Night sweats | Excessive sweating during sleep. | Aching | A dull, persistent pain in the joints, often described as a deep soreness. |
| Mood swings | Changes in emotional state, including irritability and anxiety. | Soreness | A feeling of tenderness or discomfort in the joints, often triggered by movement or pressure. |
| Vaginal dryness | Decreased lubrication and moisture in the vaginal area. | Swelling | An increase in the size of the joint, often accompanied by warmth and tenderness. |
Underlying Mechanisms of Joint Pain
Menopause brings about a cascade of hormonal changes, and unfortunately, this often translates into various physical discomforts, including joint pain. Understanding the intricate biological mechanisms behind this connection is crucial for managing the symptoms effectively and improving overall well-being. This exploration delves into the complex interplay between estrogen, inflammation, bone density, and joint health during this significant life transition.Estrogen plays a multifaceted role in maintaining healthy joints.
Menopause and joint pain can be a real pain point, literally! It’s often tricky to pinpoint the exact cause, especially when considering other potential conditions like multiple sclerosis. While researching the differences in signs of MS in women versus men can offer a helpful comparison for understanding the symptoms, it’s important to remember that joint pain during menopause is often a common symptom, sometimes mimicking other conditions.
signs of ms in women vs men are certainly worth a look, but ultimately, a doctor’s diagnosis is crucial for proper management of any health concerns.
It acts as a crucial regulator of various physiological processes within the body, including those that impact joint function. Its anti-inflammatory properties contribute to a smoother, less painful joint experience. When estrogen levels decline during menopause, this delicate balance is disrupted, potentially leading to an increased risk of joint pain and other related issues.
Role of Estrogen in Joint Health, Menopause and joint pain
Estrogen’s influence on joint health extends beyond its direct anti-inflammatory effects. It’s involved in maintaining the integrity of cartilage, the smooth tissue that cushions joints. Adequate estrogen levels contribute to cartilage’s resilience and ability to withstand stress. This cushioning effect is essential for preventing friction and pain during movement. Decreased estrogen levels can result in thinning or weakening of cartilage, leading to joint pain and stiffness.
Potential Inflammatory Processes
Inflammation is a key player in the development of joint pain during menopause. The decline in estrogen levels can trigger inflammatory responses in the joints. This inflammatory process can lead to the breakdown of cartilage and the development of pain, swelling, and stiffness. Chronic inflammation can also contribute to the progression of joint problems over time. The exact mechanisms by which estrogen regulates inflammation are still under investigation.
Connection Between Bone Density Changes and Joint Pain
Bone density changes associated with menopause are directly linked to joint pain. As estrogen levels decrease, bone density often diminishes, increasing the risk of osteoporosis and fractures. These fractures can directly impact joints, causing pain and instability. Furthermore, the weakening of bones can increase the likelihood of micro-fractures in the surrounding joint structures, which can also contribute to pain and discomfort.
These micro-fractures are often asymptomatic but can still impact the overall health and function of the joint.
Correlation Between Estrogen Levels and Joint Health Markers
| Estrogen Level | Joint Health Marker | Impact |
|---|---|---|
| Low | Bone Density | Decreased |
| Low | Cartilage Thickness | Thinning |
| Low | Inflammation Markers | Increased |
The table above highlights the negative correlation between declining estrogen levels and key joint health markers. A decrease in estrogen directly impacts bone density, leading to thinner cartilage, and triggers an increase in inflammatory markers. These factors combine to increase the risk of joint pain and discomfort during menopause.
Types and Symptoms of Joint Pain
Menopause brings a host of physical changes, and joint pain is a common complaint among women experiencing this transition. Understanding the different types of joint pain and their associated symptoms can help women manage their discomfort and seek appropriate medical advice. This section delves into the various forms of joint pain linked to menopause, highlighting the affected areas and distinguishing symptoms.
Types of Menopausal Joint Pain
Various types of joint pain can manifest during menopause, each with its own characteristics. These types of pain can be influenced by hormonal fluctuations and other factors, including underlying conditions.
Symptoms of Osteoarthritis
Osteoarthritis is a common form of arthritis characterized by the breakdown of cartilage within joints. Symptoms typically develop gradually over time, often beginning with mild discomfort and progressing to more significant pain. Early stages may involve stiffness and pain that improves with movement. As the condition advances, pain may persist even after activity. Characteristic symptoms include stiffness, particularly in the morning, and creaking or grinding sounds in the affected joints.
Pain can be aggravated by weight-bearing activities and may worsen with age. The progression of osteoarthritis varies significantly from person to person.
Symptoms of Menopausal-Related Joint Pain
Menopausal-related joint pain often mimics other conditions, making diagnosis challenging. Symptoms may include achy, diffuse pain, stiffness, and tenderness, particularly in the morning or after periods of inactivity. These symptoms may be accompanied by swelling and warmth around the affected joints. The pain may be intermittent and vary in intensity. It’s crucial to note that menopausal-related joint pain is not always severe or debilitating.
Comparison of Osteoarthritis and Menopausal Joint Pain
While both osteoarthritis and menopausal joint pain can cause discomfort, there are key differences in their symptoms. Osteoarthritis pain is often more localized to specific joints, like the knees, hips, or hands, and is typically associated with stiffness, creaking, and grinding. Menopausal-related joint pain, on the other hand, may be more diffuse, affecting multiple joints and accompanied by tenderness, swelling, and warmth.
The pain from menopausal-related joint pain may also be influenced by hormonal fluctuations, sometimes flaring up during specific phases of the menstrual cycle.
Table of Joint Pain Types and Symptoms
| Type of Joint Pain | Affected Joint Areas | Common Symptoms |
|---|---|---|
| Osteoarthritis | Knees, hips, hands, spine | Pain, stiffness, creaking, grinding, swelling, reduced range of motion |
| Menopausal-related joint pain | Multiple joints, often diffuse | Achy pain, stiffness, tenderness, swelling, warmth, intermittent pain, pain influenced by hormonal fluctuations |
Diagnosis and Evaluation
Navigating joint pain during menopause can feel like a puzzle with missing pieces. Understanding the diagnostic process and evaluation methods is crucial for pinpointing the cause and developing an effective management plan. This involves a thorough assessment of your symptoms, medical history, and physical examination, alongside appropriate imaging studies.Accurate diagnosis relies on a multi-faceted approach that considers the interplay of menopausal hormonal changes and potential underlying conditions.
This process ensures the most appropriate treatment strategy is selected, leading to a better quality of life.
Diagnostic Process for Menopausal Joint Pain
The diagnostic process for menopausal joint pain starts with a comprehensive evaluation. This involves a detailed discussion of your symptoms, including the location, intensity, duration, and any factors that seem to exacerbate or alleviate the pain. The evaluation also considers the presence of any other symptoms associated with menopause, such as hot flashes, sleep disturbances, or mood changes.
Methods for Evaluating Severity and Location of Pain
Evaluating the severity and location of the pain is a critical aspect of the diagnosis. This is accomplished through standardized pain scales, such as the Visual Analog Scale (VAS), which allows you to rate the pain intensity on a numerical scale. The location of the pain is meticulously mapped to pinpoint the affected joints. This information is vital for understanding the potential causes and guiding the subsequent diagnostic steps.
Specific joint areas (e.g., hands, knees, hips) are assessed to correlate pain with potential underlying conditions.
Importance of Medical History and Physical Examination
A detailed medical history is essential to identify potential risk factors and pre-existing conditions that might contribute to the joint pain. This includes a review of any previous injuries, surgeries, or medical conditions, as well as family history of joint disorders. A thorough physical examination, including range of motion testing and palpation of affected joints, allows the healthcare professional to assess joint tenderness, swelling, and any signs of inflammation.
This information helps distinguish between various causes of joint pain and narrows down the possibilities.
Role of Imaging Techniques (X-rays, MRIs) in the Diagnosis
Imaging techniques, such as X-rays and MRIs, can provide valuable information about the structure and condition of the affected joints. X-rays are useful for detecting bone abnormalities, such as fractures, osteoarthritis, or joint space narrowing. MRI scans provide a more detailed view of soft tissues, including cartilage, tendons, and ligaments, which can be helpful in identifying inflammation or other soft tissue injuries.
The use of these imaging modalities is tailored to the specific symptoms and concerns raised during the initial evaluation.
Flowchart Illustrating the Diagnostic Pathway for Menopausal Joint Pain
A typical diagnostic pathway for menopausal joint pain might follow this general flow:
| Step | Action |
|---|---|
| 1 | Detailed patient history and physical examination |
| 2 | Assessment of pain severity and location using standardized scales |
| 3 | Consideration of potential risk factors and pre-existing conditions |
| 4 | Review of laboratory tests (e.g., blood tests) if indicated |
| 5 | Imaging studies (X-rays, MRIs) if necessary |
| 6 | Referral to a specialist (e.g., rheumatologist) if indicated |
| 7 | Diagnosis and treatment plan |
This flowchart represents a generalized approach and may vary depending on individual cases. The key is to take a comprehensive and tailored approach to accurately diagnose the cause of joint pain and provide the most appropriate treatment plan.
Management and Treatment Strategies
Navigating menopausal joint pain requires a multifaceted approach, combining various strategies for optimal management. Addressing this discomfort involves understanding the interplay of hormonal changes and lifestyle factors, tailoring treatment to individual needs and preferences. Successful strategies often encompass both non-pharmacological interventions and, when necessary, the use of medications.Effective management of menopausal joint pain encompasses a holistic strategy. It is crucial to remember that pain experiences differ significantly among individuals.
Thus, a personalized approach, integrating lifestyle adjustments and medical interventions, is key to achieving optimal outcomes.
Non-Pharmacological Interventions
Lifestyle modifications play a significant role in managing menopausal joint pain. These interventions, often complementary to medical treatments, focus on promoting overall well-being and reducing pain triggers.
- Regular Exercise:
- Dietary Modifications:
- Weight Management:
- Stress Management Techniques:
Maintaining a regular exercise routine is crucial for maintaining joint health and mobility. Aerobic activities, such as brisk walking, swimming, or cycling, improve cardiovascular health and strengthen muscles supporting joints. Strength training exercises, such as weightlifting or resistance band workouts, build muscle mass, which provides additional support and reduces stress on joints. Choosing activities that are enjoyable and sustainable is vital for long-term adherence.
A balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can positively impact joint health. Limiting processed foods, refined sugars, and excessive saturated fats may help reduce inflammation. Adequate intake of essential nutrients, including calcium and vitamin D, is important for maintaining bone health, which is often affected during menopause.
Maintaining a healthy weight is crucial for reducing stress on joints. Excess weight puts extra pressure on weight-bearing joints like knees and hips, potentially exacerbating pain. A balanced diet and regular exercise are vital for achieving and maintaining a healthy weight.
Chronic stress can contribute to muscle tension and pain. Incorporating stress-reducing activities, such as yoga, meditation, or deep breathing exercises, can be beneficial in managing joint discomfort. These techniques promote relaxation and reduce overall tension in the body.
Pharmacological Interventions
Medications can play a vital role in managing menopausal joint pain, particularly when non-pharmacological interventions are insufficient. These interventions are typically prescribed by a healthcare professional.
- Over-the-Counter Pain Relievers:
- Prescription Pain Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help reduce inflammation and pain. However, these medications should be used cautiously and in accordance with recommended dosages to avoid potential side effects.
In cases of severe or persistent joint pain, prescription-strength pain relievers may be necessary. These medications are typically prescribed by a physician and should be used as directed.
Hormone Therapy Options
Hormone therapy (HT), also known as hormone replacement therapy (HRT), may be considered for managing menopausal joint pain, particularly when it is associated with other menopausal symptoms. However, it’s crucial to discuss the potential benefits and risks with a healthcare professional.
- Potential Benefits:
- Potential Risks:
HT can potentially alleviate joint pain by addressing hormonal imbalances associated with menopause. Some studies suggest that estrogen may have anti-inflammatory properties that can reduce joint pain.
HT carries potential risks, including an increased risk of blood clots, stroke, and certain types of cancer. Therefore, careful consideration of the risks and benefits is essential before initiating HT.
Comparison of Treatment Options
| Treatment Option | Description | Potential Benefits | Potential Risks |
|---|---|---|---|
| Exercise | Regular physical activity, including aerobic and strength training. | Improved joint mobility, reduced inflammation, weight management. | Potential for minor injuries if not performed correctly; may exacerbate pain if intensity is too high initially. |
| Dietary Modifications | Focus on anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids. | Reduced inflammation, improved overall health. | May require significant dietary adjustments; may not address all pain. |
| Weight Management | Maintaining a healthy weight through diet and exercise. | Reduced stress on weight-bearing joints. | Requires lifestyle changes; may not address underlying pain mechanisms. |
| Stress Management Techniques | Practices like yoga, meditation, and deep breathing. | Reduced muscle tension, improved mood, potential pain reduction. | May not be effective for all individuals; may require professional guidance. |
| Over-the-Counter Pain Relievers | NSAIDs such as ibuprofen or naproxen. | Effective pain relief and inflammation reduction. | Potential for stomach upset, kidney problems, or bleeding risks. |
| Prescription Pain Medications | Stronger pain relievers prescribed by a doctor. | Significant pain relief for severe cases. | Potential for more serious side effects, such as liver damage or digestive issues. |
| Hormone Therapy | Estrogen-based therapy. | Potential relief of joint pain related to hormonal imbalances. | Increased risk of blood clots, stroke, and certain types of cancer. |
Lifestyle Recommendations
Navigating menopause often means embracing new strategies for maintaining overall well-being, including joint health. This crucial period brings about hormonal shifts that can impact various bodily functions, and understanding how lifestyle choices can mitigate the discomfort associated with menopausal joint pain is key. Implementing healthy habits can significantly improve quality of life during this transition.Adopting a proactive approach to joint health involves incorporating specific dietary choices, regular exercise, and stress management techniques.
A holistic strategy that addresses these key areas can create a supportive environment for your body during menopause.
Dietary Guidelines for Reducing Inflammation
A balanced diet plays a pivotal role in managing inflammation, a key factor in menopausal joint pain. Focus on foods rich in anti-inflammatory compounds and nutrients essential for bone health.
- Prioritize fruits and vegetables:
- Embrace healthy fats:
- Include bone-building foods:
- Limit processed foods, sugar, and unhealthy fats:
Berries, leafy greens, and colorful vegetables provide vitamins, minerals, and antioxidants that combat inflammation. Include a variety of these in your daily meals for optimal benefits.
Omega-3 fatty acids, found in fatty fish like salmon, flaxseeds, and chia seeds, possess potent anti-inflammatory properties. These fats contribute to overall joint health.
Calcium-rich foods like dairy products, leafy greens, and fortified plant-based milks are crucial for maintaining bone density, which is vital as bone loss can be accelerated during menopause. Include them regularly in your meals.
These foods can exacerbate inflammation. Reducing intake of processed foods, sugary drinks, and saturated fats can significantly contribute to better joint health.
Dietary Guidelines for Promoting Bone Health
Strong bones are essential for preventing fractures and supporting joint function. A diet rich in calcium and vitamin D is crucial during menopause to combat bone loss.
- Prioritize calcium intake:
- Supplement with vitamin D:
- Include vitamin K-rich foods:
Calcium is the cornerstone of strong bones. Include dairy products, leafy greens, and fortified foods in your diet. Dairy products such as milk, yogurt, and cheese are excellent sources.
Vitamin D is essential for calcium absorption. Exposure to sunlight, consuming fatty fish, and supplements can help meet your daily needs. Consult a healthcare professional for appropriate dosage recommendations.
Vitamin K plays a role in bone metabolism and can help prevent bone loss. Leafy greens, such as kale and spinach, are excellent sources.
Importance of Regular Exercise and Physical Activity
Regular physical activity strengthens muscles, supports joint mobility, and boosts overall well-being. Maintaining a regular exercise routine can help mitigate joint pain and stiffness.
- Engage in low-impact exercises:
- Include strength training:
- Maintain flexibility and balance:
Activities like walking, swimming, and cycling are gentle on the joints while effectively improving cardiovascular health and muscle strength. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
Strengthening muscles around joints can provide crucial support and stability. Incorporate exercises that target major muscle groups, such as squats, lunges, and resistance band workouts. Consult with a physical therapist for safe and effective exercises tailored to your individual needs.
Ugh, menopause and those pesky joint aches! It’s a real drag, isn’t it? Finding relief can be tough, but did you know massage therapy helps relieve pain? Massage therapy helps relieve pain by targeting those sore spots and improving circulation, potentially easing the discomfort associated with menopause and joint pain. So, maybe it’s time to book that massage appointment and see if it helps with those pesky achy joints!
Yoga, Pilates, and tai chi are excellent for improving flexibility, balance, and reducing stiffness. These activities can significantly improve overall joint health and prevent falls.
Stress Management Techniques and Their Impact on Joint Health
Chronic stress can negatively impact the body, including joint health. Effective stress management strategies can contribute to reducing inflammation and promoting overall well-being.
- Practice relaxation techniques:
- Engage in activities you enjoy:
- Prioritize sleep:
Techniques like deep breathing exercises, meditation, and progressive muscle relaxation can help reduce stress hormones and promote relaxation.
Hobbies, spending time with loved ones, or pursuing interests can serve as powerful stress relievers.
Adequate sleep is essential for physical and mental restoration. Establish a regular sleep schedule and create a conducive sleep environment to promote better sleep quality.
Lifestyle Recommendations for Women Experiencing Menopausal Joint Pain
- Maintain a balanced diet rich in anti-inflammatory foods and bone-building nutrients.
- Engage in regular low-impact exercise and strength training to support joint health.
- Prioritize stress management techniques to reduce inflammation and promote overall well-being.
- Stay hydrated by drinking plenty of water throughout the day.
- Maintain a healthy weight to reduce stress on joints.
- Consider consulting a healthcare professional for personalized recommendations.
A Healthy Diet to Support Joint Health During Menopause
A healthy diet tailored for joint health during menopause emphasizes whole foods and nutrient-rich ingredients.
| Food Group | Specific Foods | Benefits |
|---|---|---|
| Fruits and Vegetables | Berries, leafy greens, colorful vegetables | High in antioxidants and vitamins, reducing inflammation. |
| Protein Sources | Lean meats, poultry, fish, beans, lentils | Essential for muscle repair and overall health. |
| Healthy Fats | Fatty fish, avocados, nuts, seeds | Rich in omega-3 fatty acids, promoting anti-inflammatory effects. |
| Dairy/Alternatives | Milk, yogurt, cheese, fortified plant-based alternatives | Excellent sources of calcium and vitamin D, crucial for bone health. |
| Whole Grains | Brown rice, quinoa, whole-wheat bread | Provide essential nutrients and fiber for overall health. |
This comprehensive dietary approach, incorporating a wide variety of nutrient-rich foods, supports overall health and well-being during menopause, particularly concerning joint health.
Prevention Strategies
Menopause’s impact on joint health can be mitigated through proactive strategies. Understanding the underlying mechanisms and risk factors allows for the development of preventative measures, particularly during pre-menopause and throughout life. A healthy lifestyle, encompassing diet, exercise, and stress management, plays a crucial role in reducing the risk of joint pain during this transition.Maintaining a healthy weight and adopting a balanced diet rich in essential nutrients is paramount for overall well-being and joint health.
Regular exercise, including strength training and low-impact activities, strengthens muscles that support joints, improving stability and reducing stress on them. Effective stress management techniques, such as mindfulness and yoga, can also contribute to overall well-being and reduce inflammation, potentially minimizing joint discomfort.
Maintaining a Healthy Lifestyle Throughout Life
A healthy lifestyle isn’t just about preventing joint pain during menopause; it’s about fostering long-term well-being. Prioritizing a balanced diet with adequate calcium and vitamin D is crucial for bone health, reducing the risk of osteoporosis, a condition often linked to joint pain. Regular physical activity, including weight-bearing exercises, helps maintain bone density and strengthens muscles surrounding joints, making them more resilient to stress.
Managing stress effectively, through techniques like meditation or spending time in nature, helps reduce inflammation throughout the body, potentially easing joint discomfort.
Preventive Measures During Pre-menopause
Implementing preventative measures during pre-menopause can significantly reduce the likelihood of experiencing joint pain later. This period offers a window of opportunity to establish healthy habits that will benefit joint health long-term. Maintaining a healthy weight through a balanced diet and regular exercise is vital during this stage. Regular check-ups with a doctor are important for early detection and management of any potential risk factors.
Early intervention for conditions like vitamin D deficiency or early signs of arthritis can significantly reduce the impact on joint health during menopause.
Role of Early Detection and Management of Risk Factors
Early detection and management of risk factors are essential in preventing or mitigating joint pain during menopause. Regular medical check-ups, including blood tests to assess hormone levels and bone density scans, can help identify potential issues early on. Addressing any identified deficiencies, such as vitamin D or calcium, through dietary changes or supplementation, can significantly impact bone health and joint health.
If conditions like osteoarthritis or rheumatoid arthritis are suspected, early diagnosis and appropriate management can slow disease progression and minimize joint pain. This proactive approach can lead to better long-term outcomes and improved quality of life.
Summary of Preventative Actions
Implementing a comprehensive approach to joint health throughout life is key to minimizing the impact of menopause on joint health. A balanced diet, regular exercise, and effective stress management are cornerstones of this strategy. Early detection and management of risk factors, like vitamin deficiencies or early signs of arthritis, are critical during pre-menopause. These preventative actions, when combined with a holistic approach to health and well-being, can significantly reduce the likelihood and severity of joint pain during menopause.
Summary: Menopause And Joint Pain
Navigating menopause and joint pain requires a multifaceted approach that blends medical guidance with lifestyle choices. This discussion has highlighted the intricate relationship between hormonal shifts and joint health, emphasizing the importance of accurate diagnosis and tailored treatment plans. By understanding the underlying mechanisms, recognizing symptoms, and implementing effective management strategies, women can effectively cope with the challenges of menopausal joint pain and maintain a good quality of life.
Remember, seeking professional medical advice is essential for personalized care.