Macular telangiectasia eye disease is a condition affecting the macula, a crucial part of the retina responsible for sharp central vision. This comprehensive look explores the various types, symptoms, causes, and potential impacts on daily life. We’ll delve into the complexities of diagnosis, treatment options, and the vital role of research in improving outcomes for those affected.
Understanding the intricacies of this eye disease requires an exploration of its different forms, such as types 1 and 2, each with its own unique characteristics. This detailed examination will reveal the nuances in symptoms and progression, equipping you with the knowledge needed to grasp the challenges faced by those affected.
Introduction to Macular Telangiectasia
Macular telangiectasia is a chronic eye condition affecting the macula, the central part of the retina responsible for sharp, detailed vision. This delicate area of the eye is highly susceptible to damage, and telangiectasia involves the abnormal widening and development of tiny blood vessels. The resulting changes in the macula can significantly impair vision, ranging from subtle blurring to profound loss of central vision.The core characteristic of macular telangiectasia is the development of these abnormal blood vessels in the macula.
This structural alteration leads to leakage of fluid and blood, potentially causing inflammation and scarring that compromise the macula’s function. The progression of the disease can vary, affecting each individual differently. Understanding the different types and symptoms is crucial for timely diagnosis and management.
Types of Macular Telangiectasia
Macular telangiectasia presents in two primary forms, each with its own set of characteristics: type 1 and type 2. Type 1, also known as “classic” macular telangiectasia, is characterized by the development of small, dilated blood vessels within the macula. Type 2, on the other hand, exhibits larger, tortuous blood vessels in the macula, frequently accompanied by macular edema.
Symptoms of Macular Telangiectasia
The symptoms associated with macular telangiectasia typically manifest gradually. Common symptoms include blurring or distortion of central vision, difficulty reading or recognizing faces, and a gradual loss of fine details. The perception of straight lines appearing wavy or distorted is also frequently reported. The initial symptoms are often subtle and may not be immediately recognized as a sign of an underlying disease.
Progression of Macular Telangiectasia
The progression of macular telangiectasia varies significantly depending on the type. Early stages might be marked by mild visual changes, while later stages can lead to considerable loss of central vision. The rate of progression can also differ between individuals. Factors such as age, genetics, and lifestyle choices might influence the speed at which the disease progresses.
Progression Stages by Type
| Type | Symptoms | Progression Stages |
|---|---|---|
| Type 1 | Initially, patients may experience mild blurring or distortion of central vision. Gradually, the symptoms worsen, with increasing difficulty in tasks requiring fine visual acuity. | Early: Subtle vision changes. Middle: Progressive loss of central vision, difficulty reading and recognizing faces. Late: Significant loss of central vision, potential for complete loss of vision in severe cases. |
| Type 2 | Patients typically experience more pronounced symptoms from the outset, with noticeable blurring and distortion of central vision. Fluid accumulation in the macula may contribute to a rapid decline in vision. | Early: Significant vision changes, with symptoms noticeable from the start. Middle: Rapid loss of central vision, pronounced distortion of straight lines. Late: Severe loss of central vision, potential for complete loss of vision in advanced stages. |
Causes and Risk Factors
Understanding the causes and risk factors of macular telangiectasia is crucial for early detection and management. While the precise mechanisms behind the development of this eye disease are still under investigation, several contributing factors have been identified. This knowledge helps in identifying individuals at higher risk and potentially influencing preventative strategies.The exact causes of macular telangiectasia remain largely unknown.
However, a combination of genetic predisposition and environmental factors appears to play a significant role in the development of the disease. Research continues to unravel the complex interplay between these elements, leading to a deeper understanding of the condition.
Genetic Predisposition, Macular telangiectasia eye disease
Genetic factors contribute significantly to the risk of developing macular telangiectasia. Certain genetic variations are associated with an increased likelihood of developing the disease. Individuals with a family history of the condition are more susceptible, suggesting a hereditary component. Studies are ongoing to identify specific genes involved, which could lead to more accurate risk assessment and potentially targeted therapies in the future.
Environmental Factors
Environmental factors also influence the development of macular telangiectasia. Smoking, for instance, is a known risk factor, potentially contributing to the development or progression of the disease. Prolonged sun exposure, particularly without adequate eye protection, may also play a role, although more research is needed to fully understand the relationship. Lifestyle choices, including diet and overall health, may also influence the risk, but further investigation is required to establish clear correlations.
Macular telangiectasia, a frustrating eye condition, can sometimes make you feel like your vision is playing tricks on you. While focusing on healthy eating is crucial for overall well-being, especially when dealing with eye health, it’s important to be mindful of what you eat if you’re experiencing digestive issues like diarrhea. For example, some foods can irritate your gut and worsen the problem, so check out this article on Foods to Avoid When You Have Diarrhea for helpful tips.
Ultimately, maintaining a balanced diet and focusing on nutritious foods is essential for managing both digestive health and eye health in the long run, particularly with macular telangiectasia.
Risk Factors Summary
Several factors have been identified as potentially increasing the risk of macular telangiectasia. It’s important to remember that these are not definitive causes, but rather factors associated with an elevated risk.
- Family history of macular telangiectasia
- Smoking
- Prolonged sun exposure without eye protection
- Age (the risk generally increases with age)
- Certain underlying health conditions, such as hypertension or diabetes
Comparison of Risk Factors for Different Types
While the exact causes remain unclear, some differences exist in risk factors between the different types of macular telangiectasia. A table below summarizes these observed variations. Note that the data is based on current research and more definitive comparisons may emerge as studies progress.
Macular telangiectasia, a condition affecting the eye’s macula, can cause vision problems. While seemingly unrelated, similar vascular issues can also lead to hematuria, or blood in the urine, as explored in this insightful article about Hematuria Blood in Urine Possible Causes in Men. Understanding these vascular connections is crucial for comprehensive health awareness, highlighting the importance of seeking expert advice for both conditions like macular telangiectasia.
| Risk Factor | Macular Telangiectasia Type 1 | Macular Telangiectasia Type 2 |
|---|---|---|
| Family history | High | Moderate |
| Smoking | Moderate to High | Moderate |
| Sun exposure | Moderate | Low |
| Age | High | High |
| Underlying health conditions | Moderate | Moderate |
Diagnosis and Evaluation
Diagnosing macular telangiectasia requires a careful evaluation by an ophthalmologist. The process involves a series of tests designed to identify the specific type of macular telangiectasia and assess its severity. Accurate diagnosis is crucial for determining the appropriate treatment plan and monitoring disease progression.
Diagnostic Procedures
Macular telangiectasia is diagnosed through a combination of clinical examinations and specialized imaging techniques. Ophthalmologists use a systematic approach to gather information and ensure a precise diagnosis.
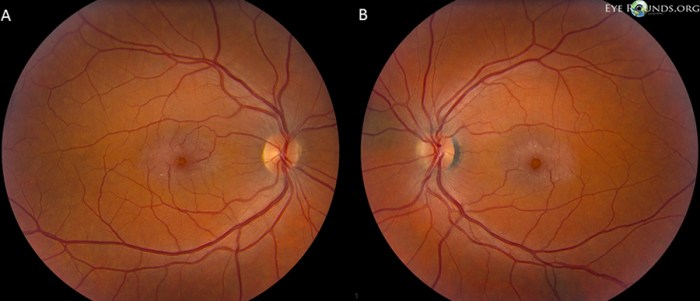
Ophthalmoscopy
A crucial initial step is ophthalmoscopy, which involves using an ophthalmoscope to examine the retina. This instrument allows the doctor to visualize the blood vessels in the macula. The presence of dilated, tortuous, and/or clustered blood vessels is a key indicator of macular telangiectasia. The ophthalmologist carefully assesses the extent and characteristics of the telangiectasia. Variations in the appearance of the telangiectasia, including their size and distribution, help in determining the specific type of the disease.
Specialized Imaging Techniques
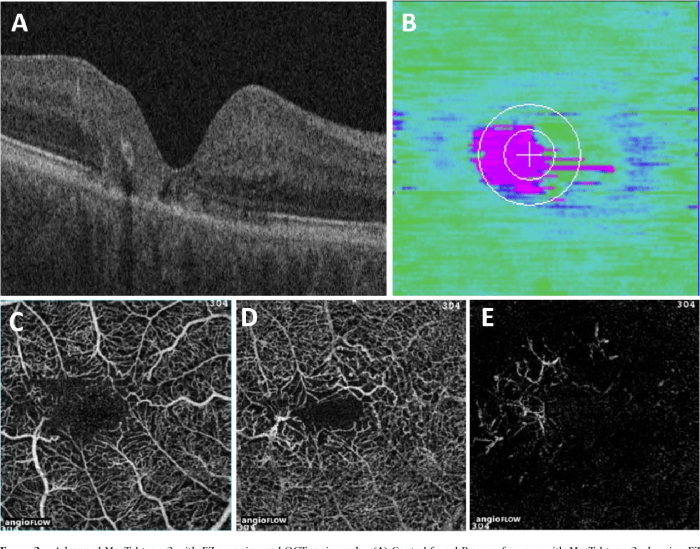
Advanced imaging techniques further refine the diagnostic process. Fundus photography provides detailed still images of the retina, allowing for comparison over time. Fluorescein angiography (FA) is a valuable tool. It involves injecting a fluorescent dye into the bloodstream. The dye highlights the blood vessels in the retina, revealing any abnormalities in their structure and function.
This method is especially helpful in identifying the leakage of fluid and blood. Optical coherence tomography (OCT) is another crucial technique. It produces high-resolution cross-sectional images of the retina, providing detailed views of the macula’s layers. OCT can help distinguish between macular telangiectasia and other macular conditions with similar appearances. These advanced imaging tools are crucial for comprehensive assessment.
Visual Field Tests
Visual field tests assess the patient’s peripheral vision. As macular telangiectasia progresses, it can lead to vision loss. These tests provide valuable information about the extent of the vision loss and its impact on daily activities. Various types of visual field testing are used, such as static perimetry and kinetic perimetry. These tests help determine the specific areas of vision loss.
The visual field tests are critical in evaluating the impact of the disease on the patient’s overall visual function.
Comprehensive Eye Exam Procedure
A comprehensive eye exam for macular telangiectasia typically involves these steps:
- Patient history: The ophthalmologist gathers information about the patient’s symptoms, medical history, and any family history of eye diseases.
- Visual acuity testing: This measures the sharpness of the patient’s vision using an eye chart.
- Ophthalmoscopy: The ophthalmologist examines the retina, looking for characteristic signs of macular telangiectasia, such as dilated and tortuous blood vessels.
- Specialized imaging techniques: Fluorescein angiography (FA) and optical coherence tomography (OCT) provide detailed images of the macula and surrounding tissues.
- Visual field testing: This assesses the extent of vision loss and identifies the specific areas affected.
Summary of Diagnostic Tests
| Diagnostic Test | Purpose |
|---|---|
| Ophthalmoscopy | Visual examination of the retina to detect characteristic blood vessel changes. |
| Fundus Photography | Provides detailed still images of the retina for comparison over time. |
| Fluorescein Angiography (FA) | Highlights blood vessels, revealing abnormalities in structure and function, especially leakage. |
| Optical Coherence Tomography (OCT) | Produces high-resolution images of the macula, aiding in identifying structural changes. |
| Visual Field Tests | Assesses the extent and location of visual loss. |
Management and Treatment Options: Macular Telangiectasia Eye Disease
Managing macular telangiectasia involves a multifaceted approach focusing on slowing disease progression and mitigating vision loss. Current strategies emphasize a combination of lifestyle modifications, monitoring, and, in some cases, specific treatments. Understanding the nuances of these approaches is crucial for patients and their healthcare providers.
Current Management Strategies
Current management strategies for macular telangiectasia are primarily centered on preventing further damage and preserving existing vision. These strategies include regular eye examinations to monitor disease progression and promptly address any changes. Early intervention can often slow the rate of vision loss and potentially improve outcomes.
Lifestyle Modifications
Lifestyle modifications play a significant role in managing macular telangiectasia. Adopting a healthy lifestyle can potentially reduce the risk factors associated with the disease and mitigate its progression. A diet rich in antioxidants and vitamins, such as vitamins C and E, may help protect the delicate tissues of the eye. Regular exercise and maintaining a healthy weight can also positively influence overall health and reduce cardiovascular risk, which may indirectly affect the progression of the disease.
Efficacy of Various Treatments
Various treatments are available for managing macular telangiectasia, although there’s no cure. The efficacy of each treatment varies depending on the specific subtype and stage of the disease. Laser photocoagulation is a common treatment that involves using a laser to seal off the abnormal blood vessels in the macula. This procedure aims to reduce leakage and prevent further damage.
While effective in some cases, it may not be suitable for all patients or stages of the disease.
Comparison of Treatment Options
Comparing the effectiveness of different treatment options requires careful consideration of individual patient factors. Factors such as the severity of the disease, the specific subtype, and the patient’s overall health must be taken into account when deciding on a course of treatment. While laser photocoagulation is a frequently used procedure, other options, such as anti-VEGF injections, may be considered for certain cases.
Summary Table of Treatment Options
| Treatment Option | Potential Benefits | Potential Drawbacks |
|---|---|---|
| Laser Photocoagulation | Can reduce leakage from abnormal vessels, potentially slowing vision loss. | May not be suitable for all stages or subtypes. May not completely halt progression. Potential for side effects, including scarring. |
| Anti-VEGF Injections | May reduce leakage from abnormal vessels, potentially slowing vision loss in some cases. | Requires frequent injections, potentially leading to discomfort or complications. Not effective for all patients. |
| Vitamin Supplements | May reduce risk factors, potentially slowing disease progression. | Limited clinical evidence of significant effect on disease progression. Should be taken under medical supervision. |
| Lifestyle Modifications | May reduce risk factors and support overall health, potentially slowing disease progression. | Does not directly treat the disease, but supports overall health. Requires sustained commitment. |
Impact on Vision and Daily Life
Living with macular telangiectasia can significantly impact vision quality and daily life. While the disease doesn’t typically cause complete blindness, it gradually affects central vision, making tasks that require sharp focus challenging. This progressive nature of the condition demands understanding and proactive strategies for maintaining independence and quality of life.The effects of macular telangiectasia on vision extend beyond simple blurring.
Individuals experience varying degrees of distortion, blurring, and loss of central vision. This impacts their ability to perform tasks requiring precise visual acuity. The consequences extend to numerous aspects of daily living, requiring adjustments and adaptations to maintain a fulfilling life.
Effects on Vision Quality
Macular telangiectasia primarily affects central vision, impacting the ability to see fine details, read, recognize faces, and drive. Individuals may notice blurring, distortion, and gradual loss of detail in the central part of their visual field. This can lead to difficulties in tasks that require clear vision, such as reading, writing, and recognizing faces. The gradual nature of the vision loss can make it challenging to adjust to the changing visual demands of daily life.
Impact on Daily Activities and Tasks
The impact on daily activities can range from minor inconveniences to significant challenges. Reading becomes more difficult, and navigating complex environments can be hazardous. Everyday tasks like cooking, driving, and using electronic devices can become frustrating or even impossible without assistance. Individuals may experience a decrease in their independence as they rely more on others for help with everyday activities.
Need for Assistive Technologies and Adaptations
Assistive technologies and adaptations are crucial for maintaining independence and quality of life. These tools can compensate for vision loss and help individuals continue participating in their desired activities. Examples include large-print materials, screen magnifiers, and voice-activated software. Properly selected assistive devices and techniques can help individuals maintain a sense of control and participation in their daily lives.
Macular telangiectasia, a frustrating eye condition, can sometimes be linked to underlying systemic issues. For instance, a deeper dive into the connection between eye health and hormonal imbalances like hypothyroidism and adrenal insufficiency is explored in detail in this insightful article: Hypothyroidism and Adrenal Insufficiency A Deep Dive. While the exact mechanisms aren’t fully understood, exploring these potential correlations can help in better understanding and managing macular telangiectasia.
Strategies for Maintaining Independence and Quality of Life
Maintaining independence and quality of life is paramount for individuals with macular telangiectasia. Regular eye care visits, open communication with healthcare professionals, and proactive management of the condition are essential. Learning about available assistive technologies, exploring support groups, and seeking professional guidance can provide essential tools and encouragement for adjusting to the changes in vision. Adapting daily routines and embracing assistive technologies are crucial for maintaining independence.
Potential Accommodations and Assistive Devices
- Large-print materials: Books, newspapers, and other printed materials in larger font sizes can significantly improve readability. Many libraries and bookstores offer large-print options.
- Screen magnifiers: These devices magnify computer screens, making it easier to read text and use electronic devices. Various types are available, ranging from handheld magnifiers to specialized software.
- Voice-activated software: Software that reads text aloud can assist with tasks like reading emails, documents, and websites. This can greatly improve access to information and communication.
- Assistive technology for daily living: Assistive devices for daily tasks, such as button-hookers or tools for reaching items, can help maintain independence. Adaptive devices for driving can assist with safely navigating roads and traffic.
- Visual aids: Enhancing visual aids like brightly colored objects or contrasting backgrounds can increase visibility and help with spatial awareness.
Patient Resources and Support
Navigating a macular telangiectasia diagnosis can be challenging. Having access to reliable resources and supportive communities is crucial for patients to understand their condition, manage their expectations, and live fulfilling lives. This section Artikels valuable resources and emphasizes the importance of patient education and self-management.
Reliable Resources for Patients
Understanding macular telangiectasia involves accessing accurate and trustworthy information. Numerous organizations offer comprehensive details on the disease, its progression, and available management options. Patient-centered resources are essential for empowering individuals with the knowledge they need to actively participate in their care.
- National Institutes of Health (NIH): The NIH provides extensive information on various health conditions, including macular telangiectasia. Their website offers detailed descriptions of the disease, research updates, and links to relevant studies. This is a cornerstone resource for patients seeking in-depth information and the latest advancements in research.
- American Academy of Ophthalmology (AAO): The AAO is a reputable professional organization dedicated to eye health. Their website features informative articles, educational materials, and details on different eye conditions, including macular telangiectasia. This is a valuable resource for those seeking expert perspectives and professional guidance.
- Mayo Clinic: The Mayo Clinic is a renowned medical institution known for its comprehensive medical information. Their website provides detailed explanations of various eye diseases and treatment options, making it a reliable resource for patients seeking expert insights.
Support Groups and Online Communities
Connecting with others facing similar challenges can be incredibly beneficial. Support groups and online communities offer a safe space for sharing experiences, exchanging advice, and receiving emotional support.
- Online Forums and Support Groups: Many online forums and support groups cater to individuals with specific health conditions, including macular telangiectasia. These platforms offer a chance to connect with peers who understand the unique challenges of the disease. Sharing experiences and strategies with others facing similar challenges can be highly valuable.
- Local Support Groups: Check with local eye care centers, hospitals, and community organizations to see if support groups exist for individuals with macular telangiectasia. These in-person groups can provide opportunities for direct interaction and personal connection with others who understand the specific concerns related to the condition.
Importance of Patient Education and Self-Management
Active participation in managing macular telangiectasia is essential for maintaining the best possible quality of life.
- Patient Education: Understanding the condition and its potential impact is crucial for proactive self-management. Educating oneself about treatment options, lifestyle adjustments, and potential complications empowers individuals to make informed decisions regarding their care.
- Self-Management Strategies: Implementing strategies for managing symptoms, including regular eye exams, medication adherence, and healthy lifestyle choices, can significantly impact the course of the disease and overall well-being.
Role of Ophthalmologists and Other Healthcare Professionals
Ophthalmologists play a vital role in the diagnosis and management of macular telangiectasia. Collaborating with other healthcare professionals is also important for comprehensive care.
- Ophthalmologists: Ophthalmologists are eye specialists who diagnose and manage macular telangiectasia. They are essential for monitoring the disease’s progression, recommending appropriate treatments, and providing guidance on managing vision loss.
- Other Healthcare Professionals: Collaboration with other healthcare professionals, such as optometrists, nutritionists, and therapists, can provide additional support and resources for managing the broader impacts of the condition on daily life.
Patient Resources and Support Organizations
This table provides links to organizations that offer resources and support for patients with macular telangiectasia.
| Organization | Website |
|---|---|
| American Academy of Ophthalmology | [Link to AAO website] |
| National Eye Institute (NEI) | [Link to NEI website] |
| Mayo Clinic | [Link to Mayo Clinic website] |
| [Add more organizations as appropriate] | [Add links] |
Final Conclusion

In conclusion, macular telangiectasia eye disease presents a multifaceted challenge impacting vision and daily life. Fortunately, proactive diagnosis, appropriate management strategies, and ongoing research offer hope for improving outcomes. This discussion highlights the importance of patient education and support, empowering individuals to navigate this condition effectively.