Low testosterone in women sets the stage for this enthralling narrative, offering readers a glimpse into a complex hormonal landscape. We’ll explore the intricacies of low testosterone levels in women, delving into its various definitions, measurement methods, and the diverse factors that influence them. From understanding the typical ranges to identifying potential symptoms and underlying causes, this discussion will equip you with a comprehensive knowledge base.
This comprehensive guide explores the often-overlooked issue of low testosterone in women, shedding light on its effects on physical, emotional, and cognitive well-being. We’ll examine the symptoms, potential underlying causes, and the diagnostic process. Additionally, we’ll delve into treatment options, lifestyle management, and the overall impact on women’s health, providing a thorough and informative resource for anyone interested in learning more.
Defining Low Testosterone in Women
Low testosterone in women, often referred to as low T, is a condition where the body produces insufficient amounts of this crucial hormone. While testosterone is often associated with male characteristics, it plays a vital role in women’s health, impacting various physiological functions, including bone density, muscle mass, and energy levels. Understanding this condition is important for women’s well-being and effective diagnosis and treatment.This condition is not simply a case of women having “low testosterone” like men.
The production and function of testosterone in women are distinct from those in men, leading to different clinical presentations and diagnostic approaches. Understanding the nuances of low T in women is essential for accurate assessment and appropriate management.
Defining Low Testosterone in Women
Low testosterone in women is characterized by a persistent and clinically significant deficiency in circulating testosterone levels. This deficiency, when not attributed to other medical conditions, can manifest in various ways and often requires a thorough assessment.
Measuring Testosterone Levels in Women
Several methods exist for measuring testosterone levels in women. These methods include blood tests, which are the most common and reliable approach. The specific testosterone assays used can vary, and some tests may be more sensitive than others. Furthermore, factors like the time of day the blood draw is performed, the woman’s recent activity, and even stress levels can influence the results.
These factors must be considered when interpreting the results. It is essential to discuss these factors with the healthcare provider to understand how they might impact the test results.
Factors Affecting Testosterone Measurements
Various factors can influence testosterone levels in women, making accurate measurement challenging. These include:
- Time of day: Testosterone levels naturally fluctuate throughout the day, peaking in the morning and declining as the day progresses.
- Stress levels: Stress can affect hormone production, including testosterone. Chronic stress can lead to fluctuations in testosterone levels.
- Menstrual cycle: Testosterone levels can vary during different phases of the menstrual cycle. Fluctuations are more pronounced in some women compared to others.
- Medications: Certain medications, including some contraceptives and hormone therapies, can impact testosterone levels.
- Health conditions: Underlying health conditions, such as thyroid disorders or adrenal problems, can influence testosterone production.
Typical Testosterone Ranges in Women
The normal range for testosterone levels in women is typically lower than in men, and there is considerable variation between individuals. It is not possible to provide a single, universal range as it can be influenced by various factors mentioned above. Therefore, healthcare professionals use clinical judgment and consider individual circumstances when assessing a woman’s testosterone levels.
Comparison of Symptoms in Women and Men
| Symptom | Women | Men |
|---|---|---|
| Fatigue | Reduced energy levels, decreased motivation, general tiredness | Reduced energy levels, decreased motivation, general tiredness |
| Low Libido | Reduced sexual desire and interest | Reduced sexual desire and interest |
| Mood Swings | Irritability, anxiety, depression | Irritability, anxiety, depression |
| Bone Density | Decreased bone density, increased risk of osteoporosis | Decreased bone density, increased risk of osteoporosis |
| Muscle Mass | Reduced muscle mass and strength | Reduced muscle mass and strength |
| Cognitive Function | Difficulty with concentration, memory problems | Difficulty with concentration, memory problems |
Symptoms and Manifestations: Low Testosterone In Women
Low testosterone in women, while less frequently discussed than in men, can manifest in a variety of ways, impacting physical, emotional, and cognitive well-being. Recognizing these symptoms is crucial for early diagnosis and appropriate intervention. Symptoms can vary greatly depending on the underlying cause, making accurate identification and treatment challenging. Understanding the nuances of these symptoms is essential for both healthcare providers and individuals experiencing them.The spectrum of symptoms associated with low testosterone in women is broad and can often overlap with other health conditions.
This overlap can make diagnosis difficult, emphasizing the importance of a comprehensive evaluation by a healthcare professional. Symptoms might not always be directly attributable to low testosterone but can be part of a complex interplay of factors. For example, a woman experiencing fatigue and mood swings might be experiencing these symptoms due to low testosterone, but also other factors like stress or thyroid issues.
Common Symptoms, Low testosterone in women
Low testosterone in women can present with a range of physical, emotional, and cognitive symptoms. It is important to note that these symptoms are not exclusive to low testosterone and can be caused by other factors.
- Physical symptoms include decreased libido, vaginal dryness, fatigue, muscle weakness, and decreased bone density. These physical changes can affect a woman’s daily life and overall quality of life.
- Emotional symptoms might include mood swings, irritability, anxiety, and depression. These emotional changes can be significant and impact relationships and work performance.
- Cognitive symptoms may include difficulty concentrating, memory problems, and decreased mental clarity. These cognitive symptoms can affect daily tasks and decision-making.
Overlap with Other Conditions
The symptoms of low testosterone can overlap significantly with other conditions common in women. This overlap can complicate diagnosis and necessitates a careful evaluation by a healthcare professional.
Low testosterone in women can sometimes cause a range of symptoms, like fatigue and low libido. If you’re concerned about your health, it’s important to talk to a doctor. To ensure your overall well-being, you should also know how to access free HIV testing, and an expert can guide you through this process. For example, you can find helpful information on ask an expert when and how can i get free hiv testing , which might offer insights into where to go and how to get tested conveniently.
Ultimately, understanding your health needs, including testosterone levels and safe practices like HIV testing, is key to feeling your best.
- Symptoms like fatigue, mood swings, and cognitive difficulties can be seen in various conditions, including thyroid disorders, depression, and stress. Therefore, a thorough medical history and physical examination are essential to rule out other potential causes.
- For instance, a woman experiencing both low libido and vaginal dryness might be experiencing these symptoms due to low testosterone, but also factors like menopause or certain medications. It is vital to consider these possibilities when evaluating a patient.
Variability in Symptoms
The presentation of symptoms can vary depending on the underlying cause of low testosterone. For example, a woman experiencing low testosterone due to a specific medical condition, such as adrenal insufficiency, might present with different symptoms compared to someone experiencing low testosterone due to aging.
- The severity and type of symptoms can differ based on the specific hormonal imbalance or medical condition. A thorough understanding of the patient’s medical history and other contributing factors is crucial.
- For example, a woman with PCOS might experience symptoms like irregular periods, acne, and hair growth alongside low testosterone symptoms. The symptoms are not always clearly delineated and can be interconnected.
Symptom Summary Table
The table below summarizes potential physical, emotional, and cognitive symptoms associated with low testosterone in women. Remember, this is not an exhaustive list, and individual experiences may vary.
| Category | Symptom |
|---|---|
| Physical | Decreased libido, vaginal dryness, fatigue, muscle weakness, decreased bone density |
| Emotional | Mood swings, irritability, anxiety, depression |
| Cognitive | Difficulty concentrating, memory problems, decreased mental clarity |
Underlying Causes
Low testosterone levels in women can stem from a complex interplay of factors, ranging from medical conditions to lifestyle choices and even age-related changes. Understanding these contributing elements is crucial for proper diagnosis and effective treatment strategies. This exploration delves into the multifaceted causes of low testosterone in women, highlighting the hormonal imbalances and medical conditions often associated with it.Hormonal imbalances are a significant contributor to low testosterone levels in women.
These imbalances often involve other hormones in the body, disrupting the delicate equilibrium necessary for optimal testosterone production. For example, conditions like PCOS (Polycystic Ovary Syndrome) can lead to elevated levels of androgens, such as androstenedione, which can indirectly affect testosterone production. Further, thyroid dysfunction can impact the entire endocrine system, potentially impacting testosterone levels. The interconnected nature of the endocrine system underscores the importance of a comprehensive evaluation to identify the root cause of low testosterone.
Medical Conditions Associated with Low Testosterone
Various medical conditions can negatively impact testosterone levels in women. These conditions can directly affect the ovaries or adrenal glands, or they can indirectly impact the hormonal balance.
- Polycystic Ovary Syndrome (PCOS): Characterized by hormonal imbalances, PCOS can lead to elevated androgens, which may in turn suppress testosterone production.
- Adrenal insufficiency: Conditions affecting the adrenal glands, responsible for producing steroid hormones, including cortisol and testosterone, can result in lower testosterone levels.
- Hypothyroidism: An underactive thyroid gland can disrupt the delicate hormonal balance, affecting testosterone production, and potentially other hormones. For example, a patient with hypothyroidism may experience a range of symptoms, including fatigue and decreased libido, often linked to low testosterone.
- Cushing’s syndrome: This condition involves the overproduction of cortisol, which can disrupt the hormonal balance, leading to reduced testosterone levels. For instance, a patient with Cushing’s syndrome may experience weight gain and muscle loss, often indicative of underlying hormonal imbalances.
- Diabetes: Long-term high blood sugar levels associated with diabetes can contribute to inflammation and oxidative stress, impacting various hormones, including testosterone.
Lifestyle Factors and Low Testosterone
Lifestyle choices can significantly influence testosterone levels in women. Stress, for example, can disrupt the body’s hormonal balance. Chronic stress can lead to elevated cortisol levels, which can negatively impact testosterone production. Poor diet, lack of sleep, and a sedentary lifestyle can also contribute to low testosterone.
- Stress: Chronic stress is a significant factor in hormonal imbalances. Elevated cortisol levels, a hallmark of stress, can suppress the production of other hormones, including testosterone.
- Diet and Nutrition: A diet deficient in essential nutrients or high in processed foods can negatively impact hormonal health. For example, inadequate intake of protein and healthy fats can hinder the body’s ability to produce testosterone.
- Sleep Deprivation: Insufficient sleep disrupts the body’s natural hormone cycles, potentially impacting testosterone production. The disruption in hormonal regulation associated with sleep deprivation can have a cascading effect on various bodily functions.
- Lack of Physical Activity: Regular exercise plays a crucial role in maintaining hormonal balance. A sedentary lifestyle can contribute to hormonal imbalances, including low testosterone.
Age-Related Changes and Testosterone
Age-related changes can also affect testosterone levels in women. As women transition through different life stages, including menopause, hormonal fluctuations can occur, potentially leading to a decline in testosterone production. For instance, a significant drop in estrogen and progesterone levels during menopause can trigger changes in the body’s hormonal landscape, potentially affecting testosterone.
- Menopause: The cessation of menstruation in women marks a period of significant hormonal changes, often leading to decreased testosterone production.
Diagnosis and Treatment
Low testosterone in women, while less common than in men, can significantly impact health and well-being. Accurate diagnosis and appropriate treatment are crucial for managing symptoms and improving quality of life. This section details the diagnostic process and available treatment options.
Low testosterone in women can be a tricky issue, affecting everything from energy levels to mood. One often overlooked aspect of hormonal balance is diet, specifically the types of fats we consume. Choosing the right fats, like those found in beef tallow, can potentially impact hormone production in a positive way, contrasting with the potential drawbacks of seed oils.
For a deeper dive into the pros and cons of different fats, check out this helpful comparison of beef tallow vs seed oil. Ultimately, understanding these dietary choices is key to optimizing your overall health and well-being, and therefore, addressing low testosterone.
Diagnostic Process
Diagnosing low testosterone in women requires a multifaceted approach. A thorough medical history and physical examination are essential initial steps. This involves discussing symptoms, medical conditions, medications, and family history. Physical examination may reveal signs associated with low testosterone, although these may be subtle.
Blood Tests
Blood tests are fundamental to diagnosing low testosterone. These tests measure the levels of testosterone and other related hormones. Crucially, these tests must be performed at specific times of the day and under controlled conditions to ensure accurate results. For example, testosterone levels fluctuate throughout the day, so testing at different times can yield varying results. Multiple tests may be necessary to confirm the diagnosis.
Key blood tests include:
- Total testosterone: Measures the overall amount of testosterone in the blood.
- Free testosterone: Measures the biologically active form of testosterone.
- Sex hormone-binding globulin (SHBG): A protein that binds to testosterone, influencing its availability. Understanding SHBG levels is vital as it can affect the interpretation of total and free testosterone levels.
- Other hormones: Depending on the suspected underlying cause, other hormone levels like luteinizing hormone (LH), follicle-stimulating hormone (FSH), and estradiol might be assessed.
Other Assessments
Beyond blood tests, additional assessments might be necessary to identify potential underlying causes of low testosterone. These could include:
- Imaging studies: Such as ultrasounds or MRI scans, to evaluate the ovaries and adrenal glands for potential abnormalities.
- Genetic testing: In certain cases, genetic testing might be considered to rule out specific genetic conditions that could contribute to low testosterone.
- Metabolic panel: This panel assesses various blood components, including glucose, cholesterol, and electrolytes, to evaluate overall health and rule out potential contributing factors.
Treatment Options
Effective management of low testosterone in women often involves a combination of approaches. The most appropriate treatment plan is tailored to the individual’s specific needs and underlying cause.
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) involves supplementing low testosterone levels with exogenous hormones. This can include testosterone replacement therapy, which comes in various forms like creams, gels, patches, or injections. However, HRT should be carefully considered and discussed with a healthcare provider, considering potential risks and benefits. It is essential to acknowledge that long-term effects of HRT can vary significantly based on individual circumstances and the type of HRT administered.
Lifestyle Modifications
Lifestyle modifications can complement HRT or be used as an independent approach to managing symptoms of low testosterone. These include:
- Dietary changes: A balanced diet rich in fruits, vegetables, and lean proteins can support overall health.
- Regular exercise: Engaging in regular physical activity can positively influence hormone levels and overall well-being.
- Stress management techniques: Stress reduction through meditation, yoga, or other relaxation techniques can impact hormone balance.
- Sufficient sleep: Adequate sleep is crucial for hormone regulation and overall health.
Comparison of Approaches
The choice between HRT and lifestyle modifications depends on various factors, including the severity of symptoms, the underlying cause, and individual preferences. Lifestyle modifications are often a safe and effective first-line approach, but in some cases, HRT may be necessary for significant symptom relief.
Diagnostic and Treatment Table
| Diagnostic Test | Potential Treatment Options |
|---|---|
| Total and free testosterone | Hormone replacement therapy (HRT) |
| SHBG | Lifestyle modifications |
| Imaging studies (e.g., ultrasound) | HRT or lifestyle modifications |
| Genetic testing | HRT or lifestyle modifications, depending on results |
| Metabolic panel | Dietary changes, exercise, stress management |
Impact on Women’s Health
Low testosterone, while often associated with men’s health, can significantly impact women’s well-being in various ways. Recognizing these effects is crucial for timely diagnosis and effective management strategies. Understanding how low testosterone manifests in women can help healthcare providers and individuals alike to address the underlying causes and implement appropriate treatments.Low testosterone levels in women can lead to a range of physical, mental, and reproductive health issues.
The impact of these reduced levels varies depending on the severity of the deficiency and individual factors, but the consequences can be considerable. Early intervention and appropriate treatment can often mitigate these effects, improving overall quality of life.
Physical Health Impact
The decrease in testosterone levels can affect various aspects of women’s physical health. These effects are often subtle but can accumulate over time, leading to significant consequences if left unaddressed.
- Bone Health: Low testosterone is linked to reduced bone density, increasing the risk of osteoporosis and fractures. This risk is particularly significant as women age, as bone loss accelerates naturally during menopause. Consequently, women with low testosterone may experience accelerated bone loss compared to their peers with normal testosterone levels.
- Muscle Mass and Strength: Testosterone plays a role in maintaining muscle mass and strength. Reduced levels can lead to decreased muscle mass and strength, impacting mobility and daily activities. This can lead to a decreased ability to perform tasks that require physical exertion, impacting overall physical functionality.
- Energy Levels: A decrease in testosterone can contribute to fatigue and low energy levels. This can impact daily activities, work performance, and overall quality of life. Women experiencing these symptoms might find themselves needing more rest or experiencing significant lethargy.
Mental Health Impact
Low testosterone levels can have a significant impact on women’s mental health. The subtle shifts in hormone levels can significantly affect mood and cognitive function.
- Mood Changes: Fluctuations in testosterone can contribute to mood swings, irritability, and feelings of anxiety or depression. Women experiencing these symptoms might find themselves more susceptible to mood fluctuations.
- Cognitive Function: Some studies suggest a link between low testosterone and cognitive function, potentially impacting memory and concentration. However, more research is needed to fully understand this relationship.
Reproductive Health Impact
Low testosterone can also affect reproductive health in women. The hormone plays a complex role in various aspects of the reproductive system.
- Sexual Function: Reduced testosterone levels can affect libido and sexual function. This can lead to decreased sexual desire and difficulty experiencing pleasure. However, other factors such as stress, relationship issues, or medical conditions can also contribute to decreased sexual desire.
Long-Term Health Consequences
Untreated low testosterone in women can lead to a range of long-term health consequences. These consequences can be substantial and impact various aspects of a woman’s life.
| Category | Impact |
|---|---|
| Physical Health | Increased risk of osteoporosis, reduced muscle mass, decreased energy levels, potential for chronic fatigue syndrome, increased risk of cardiovascular disease |
| Mental Health | Mood swings, irritability, anxiety, depression, decreased cognitive function |
| Reproductive Health | Decreased libido, difficulty with sexual function, potential impact on fertility (though less pronounced than in men) |
Lifestyle Factors and Management

Taking control of your lifestyle is a powerful tool in managing and potentially boosting your testosterone levels. It’s not just about medications; a holistic approach involving diet, exercise, and stress management can significantly impact your overall well-being and hormone balance. Understanding how these elements interact is crucial for optimizing your health.Healthy lifestyle choices play a vital role in maintaining optimal testosterone levels.
A balanced approach to diet, exercise, and stress management can influence hormone production and overall health. By making conscious decisions about these aspects of your life, you can positively impact your testosterone levels and overall well-being.
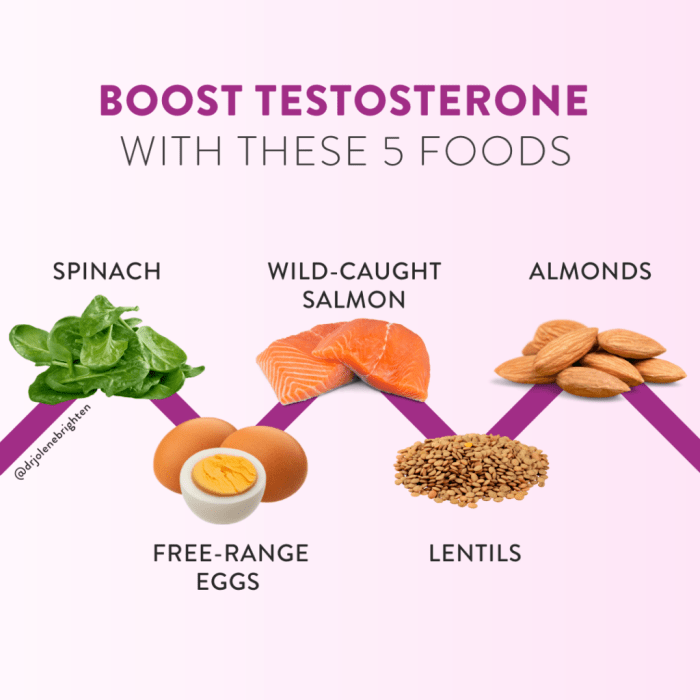
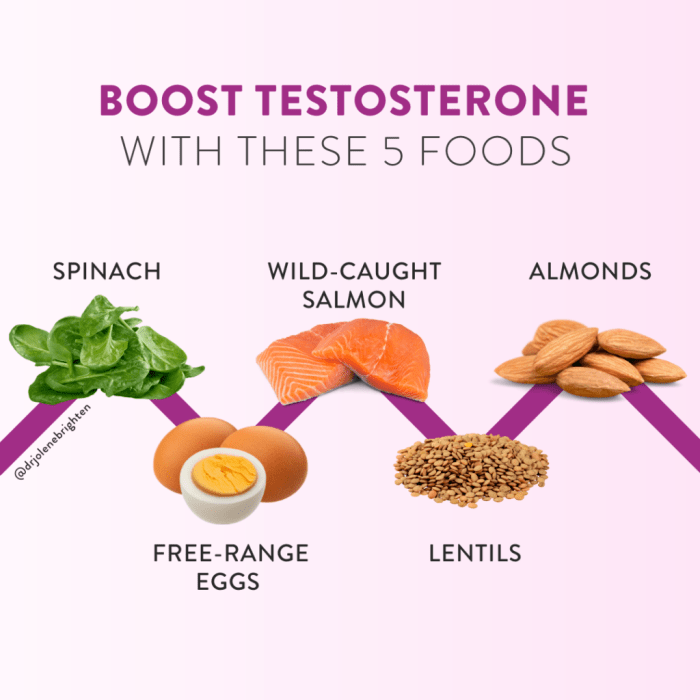
Diet Recommendations for Healthy Testosterone
A balanced diet is essential for supporting healthy testosterone levels. Focus on nutrient-rich foods that provide the building blocks for hormone production and overall health. Foods rich in zinc, magnesium, and vitamin D are particularly important.
Low testosterone in women can be a real head-scratcher, impacting everything from energy levels to libido. It’s often interconnected with other hormonal imbalances, like thyroid issues. For example, if you’re struggling with thyroid problems and skipping your medication, it can wreak havoc on your entire system, including your testosterone levels. This can lead to a cascade of unwanted symptoms, as outlined in this helpful resource on what happens when you dont take your thyroid meds.
Ultimately, keeping your thyroid health in check is crucial for overall hormonal balance, and thus, for healthy testosterone levels in women.
- Protein-rich foods: Lean meats, poultry, fish, beans, lentils, and tofu are excellent sources of protein, crucial for building and repairing tissues, which indirectly supports hormone production.
- Fruits and vegetables: A wide variety of colorful fruits and vegetables provide essential vitamins, minerals, and antioxidants, supporting overall health and hormone balance.
- Healthy fats: Include sources like avocados, nuts, seeds, and olive oil, which provide essential fatty acids and support hormone production.
- Complex carbohydrates: Choose whole grains, brown rice, and quinoa for sustained energy and overall health.
- Adequate hydration: Drink plenty of water throughout the day to support all bodily functions, including hormone production.
Exercise for Testosterone Support
Regular exercise is beneficial for overall health and can potentially influence testosterone levels. A combination of strength training and cardiovascular exercise is often recommended.
- Strength training: Focus on compound exercises that work multiple muscle groups, such as squats, deadlifts, bench presses, and rows. These exercises stimulate muscle growth, which may indirectly influence testosterone levels.
- Cardiovascular exercise: Incorporate activities like running, swimming, cycling, or brisk walking. These exercises improve cardiovascular health and contribute to overall well-being.
- Consistency: Regular exercise, rather than sporadic intense workouts, is more beneficial for sustained improvements in hormone balance and overall health.
Stress Management Techniques
Chronic stress can negatively impact hormone production, including testosterone. Implementing stress management techniques can be beneficial for maintaining healthy testosterone levels.
- Mindfulness and meditation: These practices can help manage stress and promote relaxation, which can have a positive effect on hormone balance.
- Yoga and stretching: These practices promote relaxation, reduce muscle tension, and improve overall well-being.
- Sufficient sleep: Aim for 7-9 hours of quality sleep each night, as sleep deprivation can negatively affect hormone production.
Sample Weekly Exercise Plan
This sample plan combines strength training and cardio for overall health and potential testosterone support. Adjust the intensity and duration based on your individual fitness level and preferences.
| Day | Activity | Duration/Sets |
|---|---|---|
| Monday | Strength Training (Legs) | 60-90 minutes (3 sets of 8-12 reps for each exercise) |
| Tuesday | Cardio (Running/Cycling) | 30-45 minutes |
| Wednesday | Strength Training (Upper Body) | 60-90 minutes (3 sets of 8-12 reps for each exercise) |
| Thursday | Yoga/Stretching | 30-60 minutes |
| Friday | Cardio (Swimming/Elliptical) | 30-45 minutes |
| Saturday | Rest or Active Recovery (Light walk/stretching) | 30-60 minutes |
| Sunday | Rest | Full rest |
Illustrative Cases and Examples
Understanding low testosterone in women requires exploring real-world scenarios. These case studies illustrate the diverse presentations of the condition, highlighting the importance of personalized diagnostic and treatment approaches. Each example details the specific circumstances leading to low testosterone, the diagnostic process, and the rationale behind the chosen treatment plan.
Case Study 1: Athletes with Low Testosterone
This case involves a 28-year-old female athlete experiencing persistent fatigue, decreased muscle mass, and diminished libido. Her rigorous training regime, coupled with nutritional deficiencies, likely contributed to her low testosterone levels. Initial blood tests revealed low serum testosterone and other hormonal imbalances. The diagnostic process included further blood tests to assess adrenal and thyroid function, and a comprehensive evaluation of her training and dietary habits.
Treatment focused on optimizing her diet with adequate protein intake, reducing training intensity, and supplementing with specific micronutrients to support hormone production.
Case Study 2: Women with PCOS and Low Testosterone
A 32-year-old woman presented with hirsutism, irregular menstrual cycles, and acne, indicative of polycystic ovary syndrome (PCOS). Further investigation revealed low testosterone levels, a common association with PCOS. The diagnostic process included a detailed medical history, physical examination, and hormonal analysis. Treatment included lifestyle modifications, such as a balanced diet and regular exercise, to manage PCOS symptoms and potentially restore hormonal balance.
Medication, such as oral contraceptives or anti-androgens, might be considered to regulate menstrual cycles and reduce androgenic symptoms.
Case Study 3: Women with Adrenal Insufficiency and Low Testosterone
A 45-year-old woman experiencing chronic fatigue, weakness, and decreased libido, accompanied by low blood pressure and weight loss, raised concerns about adrenal insufficiency. The diagnostic process involved measuring cortisol levels and other relevant hormones. The low testosterone levels in this case likely resulted from the underlying adrenal insufficiency. Treatment focused on replacing the deficient hormones, such as cortisol, under medical supervision.
Careful monitoring of hormone levels was crucial to ensure proper dosage and prevent potential side effects.
Treatment Outcomes Summary
| Case Study | Symptoms | Diagnosis | Treatment Approach | Outcome |
|---|---|---|---|---|
| Athlete | Fatigue, decreased muscle mass, diminished libido | Low serum testosterone, hormonal imbalances | Dietary optimization, reduced training intensity, micronutrient supplementation | Improved energy levels, increased muscle mass, improved libido |
| PCOS | Hirsutism, irregular periods, acne | Low testosterone, PCOS | Lifestyle modifications (diet & exercise), medication (oral contraceptives/anti-androgens) | Reduced androgenic symptoms, regulated menstrual cycles |
| Adrenal Insufficiency | Chronic fatigue, weakness, decreased libido, low blood pressure, weight loss | Adrenal insufficiency, low testosterone | Hormone replacement therapy (cortisol), close monitoring | Improved energy levels, normalized hormone levels, reduced symptoms |
Conclusive Thoughts
In conclusion, low testosterone in women isn’t just a medical condition; it’s a multifaceted issue impacting various aspects of a woman’s life. Understanding its symptoms, causes, and potential treatment options empowers women to take control of their health. This exploration underscores the importance of personalized care and a holistic approach to managing this condition, recognizing that every woman’s experience is unique.
We encourage further research and discussion to improve awareness and understanding.