Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious complication of diabetes, characterized by extremely high blood sugar levels without the presence of ketones. This often occurs in individuals with type 2 diabetes, particularly those who aren’t managing their blood sugar well. Understanding the underlying mechanisms, symptoms, and management strategies is crucial for anyone at risk. This blog post will explore the intricacies of HHNS, from its pathophysiology to potential complications and preventative measures.
HHNS typically develops gradually, unlike diabetic ketoacidosis (DKA), often stemming from a combination of factors like inadequate insulin, infections, or medications. The elevated blood sugar levels lead to a dangerous increase in the body’s osmotic pressure, causing dehydration and electrolyte imbalances. This complex condition requires immediate medical attention to prevent severe complications.
Introduction to Hyperglycemic Hyperosmolar Nonketotic Syndrome (HHNS)
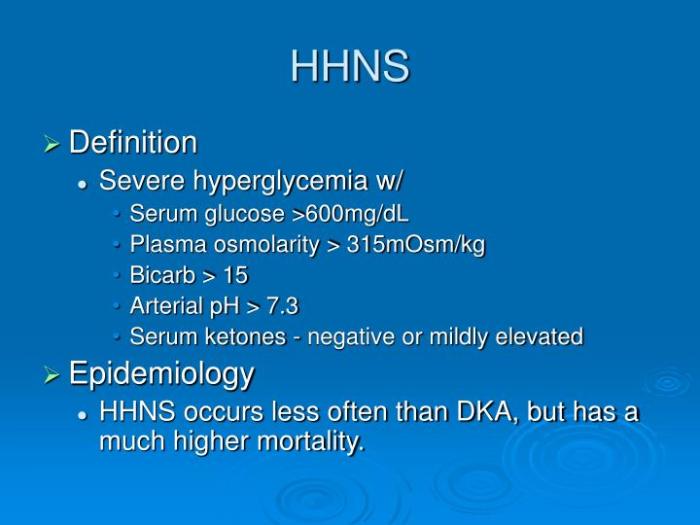
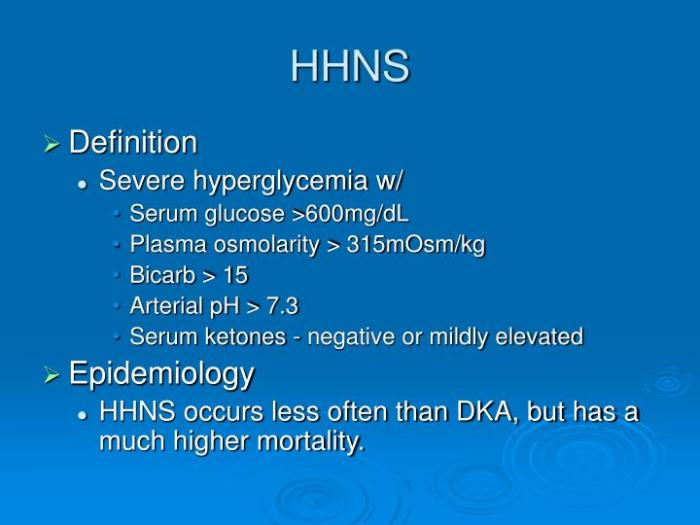
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious, life-threatening complication of diabetes mellitus, primarily in type 2 diabetes. It’s characterized by extremely high blood sugar levels without the presence of ketones in the urine or blood. This distinct feature differentiates HHNS from diabetic ketoacidosis (DKA), another serious complication. Understanding the pathophysiology, presentation, and risk factors of HHNS is crucial for early diagnosis and effective management.HHNS develops when the body’s ability to regulate blood sugar is overwhelmed, often due to a combination of factors.
The key mechanism involves a profound deficiency in insulin secretion and/or action, leading to uncontrolled hyperglycemia. This elevated blood glucose draws water out of cells, causing a dangerous shift in the body’s fluid balance and electrolyte levels. The resulting hyperosmolar state, characterized by high blood glucose levels and elevated serum osmolality, disrupts vital organ function.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) can be a serious complication of diabetes, requiring careful management. While focusing on blood sugar control is crucial, it’s also important to consider factors like the best time to take probiotics for overall gut health. Optimizing your probiotic intake, as detailed in this guide on best time to take probiotics , might indirectly support your body’s ability to manage blood sugar levels, contributing to better outcomes for HHNS.
Ultimately, consistent management of diabetes and a healthy lifestyle are key to preventing HHNS.
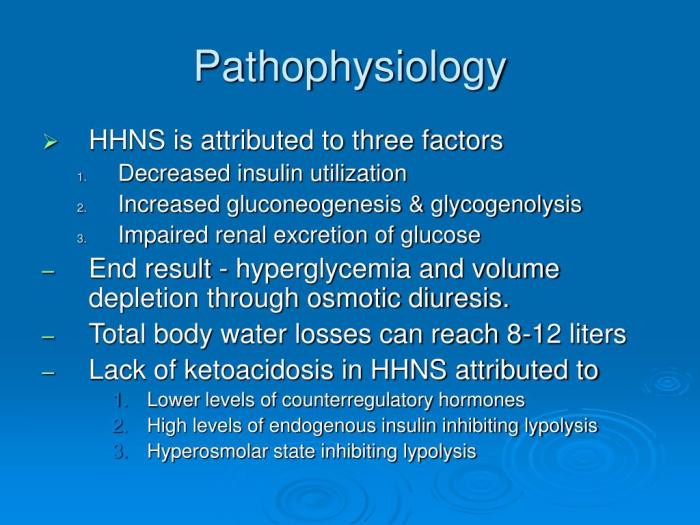
Pathophysiology of HHNS
The pathophysiology of HHNS centers around the interplay of impaired insulin secretion and/or action, and insufficient fluid intake. Insufficient insulin action allows for a significant rise in blood glucose levels. This hyperglycemia leads to osmotic diuresis, where excess glucose is excreted in the urine, pulling water with it. The loss of water leads to dehydration and an increase in serum osmolality.
The body attempts to compensate by producing more urine, further exacerbating the dehydration. This cycle perpetuates the hyperosmolar state, ultimately leading to impaired organ function.
Typical Presentation of HHNS
HHNS typically presents with a gradual onset of symptoms, often over several days to weeks. The symptoms are related to the severe dehydration and electrolyte imbalances. Patients may experience:
- Extreme thirst (polydipsia): The body’s attempt to compensate for dehydration.
- Increased urination (polyuria): Osmotic diuresis caused by high blood glucose levels.
- Dry mouth and skin: Direct effects of dehydration.
- Weakness, lethargy, and confusion: Due to the impact of hyperglycemia and dehydration on brain function.
- Headache: A common symptom that may indicate an increase in intracranial pressure.
- Vision problems: Possible consequence of the hyperosmolar state affecting the optic nerve.
Risk Factors for HHNS
Several factors can increase the risk of developing HHNS. These include:
- Poorly controlled diabetes: This is the most significant risk factor, as uncontrolled blood sugar levels increase the likelihood of severe hyperglycemia.
- Infections: Illnesses, such as pneumonia or urinary tract infections, can increase insulin needs, thereby disrupting blood glucose control.
- Certain medications: Some medications, such as diuretics, steroids, and some antipsychotics, can impair glucose regulation.
- Recent surgery or trauma: Stressful events can increase insulin requirements and impair blood glucose control.
- Insufficient fluid intake: Dehydration can worsen hyperglycemia and contribute to the development of HHNS.
- Advanced age: Older adults may have reduced ability to regulate blood glucose.
Symptoms, Severity, and Potential Causes of HHNS
| Symptom | Severity | Potential Causes |
|---|---|---|
| Extreme thirst | Mild to severe, depending on the degree of dehydration | Insufficient fluid intake, osmotic diuresis, hyperglycemia |
| Increased urination | Mild to severe, reflecting the osmotic diuresis | Hyperglycemia, dehydration |
| Weakness and lethargy | Can range from mild to profound, indicative of organ dysfunction | Dehydration, electrolyte imbalances, cerebral dysfunction |
| Confusion and altered mental status | Can progress to coma, indicating severe brain dysfunction | Hyperosmolarity, electrolyte abnormalities, cerebral edema |
| Dry mouth and skin | Severe, reflecting the dehydration | Osmotic diuresis, insufficient fluid intake |
Diagnosis and Evaluation of HHNS
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious medical emergency requiring prompt diagnosis and management. Early recognition and intervention are crucial for minimizing complications and improving patient outcomes. Accurately assessing the patient and interpreting laboratory results are vital steps in establishing a diagnosis and developing an effective treatment plan.
Diagnostic Criteria for HHNS
The diagnosis of HHNS relies on a combination of clinical presentation and laboratory findings. Key diagnostic criteria include severe hyperglycemia, typically exceeding 600 mg/dL, coupled with a serum osmolality significantly elevated above normal ranges. Absence of ketoacidosis, a hallmark of diabetic ketoacidosis (DKA), is also a defining characteristic. The clinical picture often includes profound dehydration, altered mental status, and neurological dysfunction.
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious complication of diabetes, often triggered by infections or poor blood sugar control. Managing blood sugar levels is key, and finding delicious, satisfying treats like those found in go to diabetic desserts can make a big difference in overall well-being. While enjoying these treats, it’s crucial to maintain a balanced diet and medication schedule to prevent HHNS from recurring.
These factors, alongside the laboratory data, confirm the diagnosis.
Laboratory Findings in HHNS
Several key laboratory parameters support the diagnosis of HHNS. Blood glucose levels are usually markedly elevated, frequently exceeding 600 mg/dL. Serum osmolality is also significantly elevated, reflecting the increased concentration of solutes in the blood. Electrolyte imbalances, particularly hyponatremia (low sodium), hypokalemia (low potassium), and hypochloremia (low chloride), are common. These imbalances result from the osmotic diuresis caused by the high blood glucose levels.
In addition, the serum bicarbonate levels are usually normal to slightly elevated. The presence of these findings, in combination with clinical symptoms, strongly suggests HHNS.
Evaluation Procedures for Suspected HHNS
Evaluating patients suspected of HHNS involves a comprehensive approach, including a thorough history and physical examination, alongside a series of laboratory tests. The history should focus on the patient’s medical history, including any underlying conditions, recent illness, medication use, and dietary habits. The physical examination should assess vital signs, including blood pressure, pulse, and respiratory rate. Assessing the patient’s mental status and neurological function is critical.
Blood samples are collected for comprehensive laboratory analysis, including complete blood count (CBC), serum electrolytes, glucose, blood urea nitrogen (BUN), creatinine, and serum osmolality. These analyses help confirm the diagnosis and evaluate the severity of the condition.
Dealing with hyperglycemic hyperosmolar nonketotic syndrome can be tough, especially when it comes to managing the emotional rollercoaster. It’s all too easy to feel overwhelmed, but finding healthy coping mechanisms, like those discussed in this insightful article on coping with emotions and eczema , can make a real difference. Ultimately, understanding how to navigate these feelings is key to managing the symptoms and overall well-being associated with hyperglycemic hyperosmolar nonketotic syndrome.
Significance of Key Laboratory Values
Blood glucose levels are crucial for diagnosing and monitoring HHNS. Elevated blood glucose levels, often exceeding 600 mg/dL, signify a severe hyperglycemic state. Serum osmolality reflects the concentration of solutes in the blood. Significant elevations indicate dehydration and the need for aggressive fluid resuscitation. Electrolyte imbalances, particularly hyponatremia, hypokalemia, and hypochloremia, are significant complications of HHNS.
These imbalances need prompt correction to prevent further complications.
Comparison of HHNS with Other Conditions
| Feature | HHNS | DKA ||—|—|—|| Blood Glucose | Extremely high (>600 mg/dL) | High, but can be variable || Ketones | Absent | Present || Serum Osmolality | Extremely high | Usually normal or slightly elevated || Electrolytes | Often low (hyponatremia, hypokalemia) | Can be low (hyponatremia) || Mental Status | Often altered | Can be altered || Dehydration | Often profound | Can be present, but often less severe than HHNS |The table highlights the key differences between HHNS and DKA.
While both conditions involve hyperglycemia, their underlying pathophysiology and laboratory findings differ significantly. This distinction is vital for accurate diagnosis and appropriate treatment.
Interpreting Blood Test Results Related to HHNS
Interpreting blood test results in the context of HHNS requires a thorough understanding of the patient’s clinical presentation and the specific laboratory findings. A combination of elevated blood glucose, significantly elevated serum osmolality, and electrolyte imbalances, particularly hyponatremia, provides strong evidence for HHNS. For example, a patient presenting with altered mental status, severe dehydration, and blood glucose exceeding 700 mg/dL, coupled with hyponatremia and elevated serum osmolality, strongly suggests HHNS.
Careful evaluation of the complete picture is essential for accurate interpretation and appropriate management.
Management and Treatment of HHNS
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) necessitates prompt and aggressive management to restore hydration and electrolyte balance while addressing the underlying hyperglycemia. Early intervention is crucial to prevent severe complications and improve patient outcomes. Effective management focuses on correcting the fluid and electrolyte imbalances, reducing hyperglycemia, and supporting the patient’s overall stability.The cornerstone of HHNS management lies in the meticulous administration of intravenous fluids, electrolyte replacement, and insulin therapy.
A coordinated approach, closely monitoring vital signs and laboratory values, is essential to prevent adverse reactions and ensure the patient’s safety throughout the treatment process.
Intravenous Fluid Therapy
Intravenous (IV) fluids are paramount in the initial management of HHNS. They rapidly rehydrate the patient, correct the hyperosmolar state, and improve tissue perfusion. The choice of fluid and the rate of administration are crucial for patient safety.
- Types of IV Fluids: The initial fluid choice is typically 0.9% normal saline (NS) due to its isotonic nature and ability to quickly restore intravascular volume. Later, as the serum sodium level decreases, 0.45% normal saline or even dextrose-containing solutions may be necessary to avoid hyponatremia.
- Administration Rates: The rate of fluid administration is carefully titrated based on the patient’s clinical status, including vital signs, urine output, and serum sodium levels. Initial rates might be 250-500 mL/hour, adjusted according to response. Monitoring for signs of fluid overload, such as pulmonary edema, is critical. Close monitoring of the patient’s condition is paramount throughout the process.
The goal is to rehydrate the patient without causing complications.
Electrolyte Correction
Electrolyte imbalances are common in HHNS and require careful attention. Correcting these imbalances is essential to prevent further complications and ensure the effectiveness of the overall treatment plan.
- Potassium: Hyperglycemia drives potassium into the cells, leading to hypokalemia. Frequent monitoring of potassium levels is crucial, and potassium replacement may be necessary, given the potential for cardiac arrhythmias if not addressed properly. Replacement is guided by the potassium level and clinical status. It is vital to avoid rapid potassium correction, as it can lead to potentially fatal complications.
- Sodium: HHNS is characterized by hypernatremia. Correcting hypernatremia should be done cautiously, avoiding rapid shifts in serum sodium levels, as this can lead to cerebral edema. A gradual decrease in serum sodium is usually recommended to mitigate this risk. Slow correction minimizes risk.
- Other Electrolytes: Other electrolytes like magnesium and phosphate may also be depleted, and their correction should be managed under close medical supervision.
Insulin Therapy
Insulin therapy is necessary to lower blood glucose levels and promote rehydration.
- Rationale: Insulin facilitates the uptake of glucose into cells, reducing hyperglycemia and decreasing osmotic diuresis. This in turn helps restore fluid balance.
- Approach: Low-dose insulin infusion is typically initiated. The goal is to gradually lower blood glucose levels to prevent hypoglycemia and to improve the overall patient response. A slow, steady reduction in blood glucose levels is preferred.
Step-by-Step Procedure for IV Fluid Administration in HHNS
- Assessment: Thorough patient assessment, including vital signs, blood glucose levels, and electrolyte levels, is critical. This initial assessment establishes a baseline for subsequent interventions.
- Initial Fluid Bolus: Administer a rapid IV fluid bolus (e.g., 500 mL of 0.9% normal saline) to quickly restore intravascular volume.
- Maintenance Fluid Infusion: Initiate a maintenance IV fluid infusion (e.g., 0.9% normal saline) at a rate appropriate for the patient’s needs, closely monitoring vital signs and urine output. The goal is to maintain adequate hydration and to address the underlying fluid deficit.
- Electrolyte Monitoring and Replacement: Frequent electrolyte monitoring (including potassium) is crucial. Replacement of electrolytes is administered according to laboratory results and clinical judgment.
- Insulin Therapy: Initiate low-dose insulin infusion according to protocol and patient response.
- Close Monitoring: Continuously monitor vital signs, blood glucose, electrolytes, and urine output to adjust therapy as needed.
Complications and Prognosis of HHNS
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious medical condition requiring prompt and effective management. While often treatable, the potential for complications and long-term effects on patient well-being must be carefully considered. Understanding the potential complications, influencing factors, and prognosis is crucial for both patient care and healthcare provider decision-making.
Potential Acute Complications
HHNS can lead to a cascade of acute complications, primarily stemming from the severe dehydration and electrolyte imbalances. These imbalances can disrupt various organ systems, potentially causing significant harm. Acute kidney injury is a particularly concerning complication, often resulting from the reduced blood flow to the kidneys due to dehydration and the resulting decreased glomerular filtration rate. Other potential complications include cardiovascular issues, such as heart failure or arrhythmias, and neurological complications, such as seizures or coma.
Long-Term Effects on Health and Well-being
While prompt treatment can often mitigate the acute effects of HHNS, long-term consequences can still impact patients’ health and well-being. Patients may experience persistent cognitive impairment or other neurological deficits if the brain is significantly affected by the severe hyperglycemia and dehydration. Moreover, individuals may develop an increased susceptibility to future episodes of HHNS. Sustained hyperglycemia, a hallmark of this condition, can also negatively impact vascular health, increasing the risk of cardiovascular complications over time.
Factors Influencing Prognosis
Several factors influence the prognosis of HHNS, ranging from the severity of the initial presentation to the promptness and efficacy of treatment. The patient’s underlying health status, including pre-existing conditions like cardiovascular disease or renal impairment, can significantly impact the outcome. Age, nutritional status, and the presence of concomitant infections or other illnesses also play a crucial role in determining the prognosis.
Additionally, timely access to appropriate medical care, including intensive monitoring and effective management strategies, is essential in improving the prognosis.
Mortality Rates
The mortality rate associated with HHNS is influenced by the severity of the condition and the timeliness of intervention. While the mortality rate is not as high as with diabetic ketoacidosis (DKA), it still presents a considerable risk. Studies have shown that patients with severe HHNS, particularly those with co-morbidities or delayed diagnosis, have higher mortality rates. It is important to note that the mortality rate is influenced by access to timely and appropriate medical care.
Correlation Between Severity and Complications
| Severity of HHNS | Potential Complications |
|---|---|
| Mild | Electrolyte imbalances, mild dehydration, possible confusion |
| Moderate | Moderate dehydration, electrolyte abnormalities, possible seizures, acute kidney injury |
| Severe | Severe dehydration, significant electrolyte disturbances, coma, acute kidney injury, cardiovascular complications, neurological deficits |
The table above provides a general overview. The specific complications and their severity can vary significantly depending on individual factors and the promptness of treatment. The most severe cases often require intensive care unit (ICU) management.
Prevention and Education of HHNS
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious but preventable complication of diabetes. Early detection and proactive management of risk factors are crucial in preventing HHNS. By understanding the triggers and implementing preventative measures, individuals with diabetes can significantly reduce their risk of developing this potentially life-threatening condition.
Strategies for Preventing HHNS in Susceptible Individuals
Effective prevention hinges on meticulous self-management and proactive engagement with healthcare providers. Individuals at high risk of HHNS development, such as those with poorly controlled diabetes, should prioritize consistent blood glucose monitoring, adherence to medication regimens, and prompt medical attention for any signs of illness. This proactive approach significantly minimizes the risk of hyperglycemia escalating into HHNS.
Importance of Patient Education
Patient education plays a pivotal role in empowering individuals with diabetes to actively participate in their care. Thorough education regarding blood glucose monitoring techniques, recognizing symptoms of rising blood sugar, and understanding the importance of lifestyle modifications is crucial. Comprehensive patient education programs can equip individuals with the knowledge and skills needed to effectively manage their condition and prevent complications like HHNS.
Role of Healthcare Providers in Educating Patients
Healthcare providers have a critical role in educating patients about HHNS prevention. This includes providing clear and concise information about the risks, triggers, and symptoms of HHNS. Regular follow-up appointments, personalized diabetes management plans, and ongoing support are essential components of patient education. Diabetes educators and registered dietitians can provide invaluable assistance in this process. Healthcare providers should tailor their educational approach to each patient’s individual needs and circumstances, ensuring clarity and understanding.
Tips for Managing Risk Factors
Several risk factors contribute to the development of HHNS. Managing these factors effectively can significantly reduce the likelihood of developing the syndrome. Strategies include meticulous adherence to medication regimens, consistent blood glucose monitoring, timely recognition and treatment of infections or illnesses, and proactive management of underlying medical conditions. Maintaining a healthy lifestyle, including regular exercise and a balanced diet, also plays a significant role in preventing HHNS.
Prevention Strategies Flowchart

This flowchart visualizes the key steps in preventing HHNS. It begins with routine blood glucose monitoring, progressing through identifying and managing risk factors, and culminates in early intervention when signs of illness or hyperglycemia appear.
Blood Glucose Monitoring Techniques, Hyperglycemic hyperosmolar nonketotic syndrome
Effective blood glucose monitoring is fundamental to preventing HHNS. Regular monitoring allows individuals to detect rising glucose levels early, enabling timely interventions to prevent severe hyperglycemia. Different methods, such as finger-prick testing and continuous glucose monitors (CGMs), are available, and selecting the most suitable method is crucial. Proper technique and interpretation of results are essential to effective glucose management.
Case Studies and Illustrations of HHNS: Hyperglycemic Hyperosmolar Nonketotic Syndrome
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a serious medical emergency requiring prompt diagnosis and management. Understanding real-world case studies allows healthcare professionals to better recognize the spectrum of presentations and develop effective treatment strategies. This section delves into illustrative cases, highlighting different patient presentations, management approaches, and outcomes.
Illustrative Case Studies of HHNS
Various patient presentations characterize HHNS, from subtle symptoms to severe complications. Case studies offer invaluable insights into recognizing HHNS in diverse patient populations.
- Case Study 1: A 75-year-old female with a history of type 2 diabetes and hypertension presented with progressively worsening polyuria, polydipsia, and altered mental status. Blood glucose levels were found to be extremely elevated (approximately 600 mg/dL). The patient exhibited a profound state of dehydration, with dry mucous membranes and decreased skin turgor. Management involved aggressive fluid resuscitation, insulin therapy, and electrolyte correction.
The patient’s mental status improved gradually, and she was discharged after several days of intensive care.
- Case Study 2: A 62-year-old male with type 2 diabetes, uncontrolled by medication, presented with profound weakness, lethargy, and confusion. Initial blood glucose was elevated to 550 mg/dL. The patient had a history of poor adherence to his diabetes management plan. Treatment involved correcting dehydration and administering insulin. The patient showed improvement in his mental status but required several days of monitoring due to a prolonged response to therapy.
- Case Study 3: A 30-year-old female with type 1 diabetes, poorly managed, presented to the emergency room with a Glasgow Coma Scale of 10. Her blood glucose was 700 mg/dL. This case highlighted the need for rapid diagnosis and intervention. Prompt treatment, including aggressive fluid and electrolyte replacement, and insulin therapy, led to gradual improvement in the patient’s neurological status.
The patient required prolonged hospitalization and close monitoring.
Outcomes for Patients with HHNS
Patient outcomes in HHNS vary depending on the severity of the presentation, promptness of diagnosis and treatment, and underlying comorbidities.
- Favorable Outcomes: Patients with timely and appropriate treatment, generally respond well, demonstrating improvement in their mental status and overall condition. Complete recovery and discharge from the hospital are common in cases where the disease process is contained, and the underlying condition is adequately managed.
- Moderate Outcomes: Some patients experience a prolonged recovery period with residual neurological symptoms. These cases may necessitate ongoing rehabilitation or therapy to address the lingering effects of the syndrome.
- Unfavorable Outcomes: Severe cases of HHNS, especially those with delayed diagnosis or inadequate treatment, can result in severe complications such as seizures, coma, and even death. The outcomes depend on the patient’s overall health status, severity of the syndrome, and the speed and effectiveness of treatment.
Physiological Changes During HHNS
HHNS involves a complex cascade of physiological changes, primarily centered around severe hyperglycemia and dehydration.
- Hyperglycemia: A profound increase in blood glucose levels leads to osmotic diuresis, resulting in significant fluid loss from the body. This diuresis exacerbates dehydration and further contributes to hyperosmolarity.
- Dehydration: The significant fluid loss due to osmotic diuresis causes electrolyte imbalances and impaired cellular function. This dehydration is a major contributor to the patient’s clinical presentation.
- Electrolyte Imbalances: Dehydration leads to changes in sodium, potassium, and other electrolytes. These imbalances further compromise cellular function and can contribute to neurological dysfunction.
- Neurological Dysfunction: The combination of hyperglycemia, hyperosmolarity, and electrolyte imbalances can lead to a spectrum of neurological symptoms, ranging from confusion and lethargy to seizures and coma.
Diagnosis of HHNS in a Case Study
Accurate diagnosis of HHNS involves a combination of clinical assessment and laboratory findings.
- Clinical Evaluation: The clinical picture, including symptoms such as polyuria, polydipsia, and altered mental status, is crucial in raising suspicion for HHNS.
- Laboratory Findings: Key laboratory tests include serum glucose, serum osmolality, serum electrolytes, and blood urea nitrogen (BUN)/creatinine levels to evaluate the degree of dehydration.
Final Wrap-Up
In conclusion, hyperglycemic hyperosmolar nonketotic syndrome (HHNS) is a potentially life-threatening condition requiring prompt diagnosis and aggressive management. Understanding the risk factors, symptoms, and treatment protocols is vital for both patients and healthcare providers. Prevention through proper blood glucose control and lifestyle modifications plays a key role in mitigating the risk of developing HHNS. This discussion highlights the importance of proactive diabetes management to prevent this severe complication.