How to follow a gastroparesis diet is crucial for managing this digestive condition. Gastroparesis slows the emptying of food from your stomach, impacting everything from digestion to nutrient absorption. This detailed guide offers practical strategies for navigating a gastroparesis diet, from understanding the principles to crafting personalized meal plans.
The following sections will cover essential aspects, including macronutrient considerations, food selection guidelines, meal timing and portion control, hydration strategies, and managing symptoms and potential complications. We’ll explore different approaches, provide sample meal plans, and equip you with practical tips to make healthy eating easier and more enjoyable.
Introduction to Gastroparesis Diet
Gastroparesis is a chronic condition that affects the stomach’s ability to empty properly. This dysfunction can lead to a range of digestive issues, impacting nutrient absorption and overall well-being. The delayed emptying time of the stomach disrupts the normal digestive process, leading to discomfort and potentially serious complications.A specialized gastroparesis diet is crucial for managing symptoms and preventing further complications.
By carefully controlling the types and amounts of food consumed, individuals with gastroparesis can alleviate discomfort, improve nutrient absorption, and maintain a healthy lifestyle. It’s not a one-size-fits-all approach, as individual needs and responses vary.
Common Misconceptions about Gastroparesis Diets
Many people harbor misconceptions about the gastroparesis diet. One common misconception is that all high-fiber foods should be avoided. While some high-fiber foods might be problematic, many low-fiber, easily digestible foods can be included in a well-structured gastroparesis diet. Another misconception is that eating smaller meals more frequently will always help, when in reality, meal timing and portion sizes need to be carefully individualized.
Understanding these misconceptions is crucial to developing a tailored plan.
General Principles of a Gastroparesis Diet
The cornerstone of a successful gastroparesis diet is the principle of eating smaller, more frequent meals. This approach helps to prevent the stomach from becoming overly full, thus easing the strain on the digestive system. Additionally, the diet should focus on easily digestible foods. Foods high in fat, fiber, or acidity should be consumed with caution, or eliminated if they trigger symptoms.
Liquids should be taken separately from meals to minimize gastric distention and improve emptying. Meal timing and portion sizes are also key components to consider.
Comparing Different Approaches to Gastroparesis Diet Management
Different approaches exist for managing gastroparesis symptoms through diet. These strategies vary in their focus and emphasis, but all aim to optimize digestion and minimize discomfort.
| Approach | Focus | Examples | Potential Considerations |
|---|---|---|---|
| Low-Fiber Diet | Minimizes the intake of high-fiber foods that can cause stomach discomfort and delayed emptying. | White rice, cooked pasta, lean meats, low-fiber vegetables, and well-cooked fruits. | Can be restrictive and may limit essential nutrients if not carefully planned. Ensuring adequate nutrient intake is vital. |
| High-Protein, Low-Fat Diet | Prioritizes easily digestible proteins while limiting fats, which can slow gastric emptying. | Lean proteins like chicken breast, fish, eggs, and protein shakes. | May not be suitable for everyone and may need to be adjusted based on individual needs and preferences. |
| Bland Diet | Focuses on foods that are low in acidity, spice, and texture. | Plain yogurt, white bread, boiled vegetables, and clear broths. | Can be limiting in terms of flavor and variety, requiring creativity in meal planning. |
Macronutrient Considerations
A gastroparesis diet is more than just avoiding trigger foods; it’s about carefully managing the macronutrients you consume. This involves understanding how different types of carbohydrates, proteins, and fats affect gastric emptying and, consequently, your overall well-being. Finding the right balance is crucial for preventing complications and maintaining a healthy lifestyle.
Optimal Macronutrient Proportions
Gastroparesis patients often benefit from a diet with a moderate amount of carbohydrates, a higher proportion of protein, and healthy fats. This balanced approach helps regulate blood sugar levels, support muscle function, and promote overall satiety. The exact ratios can vary based on individual needs and tolerance, but generally, a focus on protein and healthy fats is key.
Carbohydrate Impact on Gastric Emptying
Different types of carbohydrates have varying effects on gastric emptying. Simple sugars, such as those found in candy, sugary drinks, and white bread, are rapidly digested and can cause significant fluctuations in blood sugar levels, leading to faster emptying, which can trigger symptoms. Complex carbohydrates, found in whole grains, fruits, and vegetables, are digested more slowly, leading to a more gradual release of glucose into the bloodstream.
This more gradual release can help stabilize blood sugar and potentially reduce the impact on gastric emptying.
Protein’s Role in Gastroparesis
Protein plays a vital role in maintaining muscle mass and overall health. It’s crucial for preventing complications associated with malnutrition and muscle loss, both of which can negatively impact quality of life. Adequate protein intake is essential for tissue repair, immune function, and overall recovery.
Healthy Protein Sources, How to follow a gastroparesis diet
Choosing the right protein sources is important for a gastroparesis diet. Lean meats, poultry without skin, fish, eggs, Greek yogurt, and beans are excellent sources of high-quality protein that are generally well-tolerated. It’s essential to prepare these foods in ways that don’t exacerbate symptoms. For example, finely chopped or ground meats may be better tolerated than large, whole pieces.
Recommended Daily Intake Guidelines
| Macronutrient | Recommended Daily Intake (Approximate) ||—|—|| Carbohydrates | 40-50% of total calories, prioritizing complex carbohydrates || Protein | 20-30% of total calories || Fats | 30-40% of total calories, focusing on healthy fats like avocados, nuts, and olive oil |
Food Selection Guidelines: How To Follow A Gastroparesis Diet
Navigating a gastroparesis diet can feel overwhelming, but with the right knowledge and strategies, you can find delicious and satisfying meals. This section will guide you through choosing foods that are gentle on your digestive system, helping you manage your symptoms effectively. Understanding which foods are well-tolerated and which should be avoided is crucial for maintaining overall health and well-being.
Well-Tolerated Foods
A gastroparesis diet prioritizes foods that are easy to digest and won’t exacerbate your symptoms. These include lean proteins, easily digestible carbohydrates, and plenty of fiber-rich vegetables. This approach helps to minimize digestive distress and promotes a balanced nutritional intake.
Foods to Avoid or Consume in Moderation
Certain foods can significantly hinder gastric emptying, leading to discomfort and complications. These include high-fat foods, greasy or fried foods, and very large meals. Consuming these foods in moderation or avoiding them altogether is often necessary to manage symptoms effectively.
Categorizing Foods Based on Impact on Gastric Emptying
Understanding how different foods affect your gastric emptying can help you make informed choices. This table provides a general guideline, but individual tolerances may vary.
| Category | Food Examples | Impact on Gastric Emptying |
|---|---|---|
| High | Plain baked chicken breast, cooked sweet potato, steamed broccoli, cooked quinoa, mashed banana | Generally well-tolerated and empty quickly |
| Moderate | Applesauce, cooked carrots, cooked oatmeal, cottage cheese, plain yogurt | May take some time to empty, but generally tolerable |
| Low | Fried foods, fatty meats, greasy sauces, high-fiber raw vegetables, whole fruits, chocolate, dairy products, beans, lentils, popcorn | Tend to slow down gastric emptying and cause discomfort. |
Healthy Meal Ideas and Snacks
A well-structured meal plan is key to managing gastroparesis. Here are a few examples of healthy and satisfying meal ideas, keeping in mind portion sizes and easy digestion.
- Breakfast: A small bowl of cooked oatmeal with a side of plain, low-fat yogurt and a few slices of steamed apple. This combination provides sustained energy and is easy on the stomach.
- Lunch: A small turkey breast sandwich on whole-wheat bread with a side of mashed sweet potato and a small portion of steamed green beans. This provides protein and complex carbohydrates for sustained energy.
- Dinner: A baked chicken breast with a side of steamed asparagus and a small portion of cooked brown rice. This balanced meal offers protein, vegetables, and complex carbohydrates.
- Snacks: Plain yogurt with a sprinkle of cinnamon, small portions of cooked quinoa, or a small apple sliced and topped with a tablespoon of peanut butter.
Easy-to-Digest Recipes
Many recipes can be adapted for easier digestion and quicker preparation.
Following a gastroparesis diet can feel overwhelming, but it’s totally manageable with a bit of planning. Key to navigating this is finding healthy, easily digestible meals. Learning to manage stress is crucial, too, as anxiety can often exacerbate symptoms. This is where understanding how to deal with anxiety comes in handy. how to deal with anxiety techniques, like mindfulness or deep breathing exercises, can be really helpful in reducing stress and improving overall well-being.
Once you’ve got a handle on your anxiety, you can focus more effectively on sticking to your gastroparesis diet.
- Creamy Tomato Soup: Use blended canned tomatoes and a small amount of low-fat milk or broth. Avoid any added cream or thickeners. The result is a light, flavorful, and easy-to-digest soup.
- Baked Chicken Breast with Roasted Vegetables: Baking chicken breast and vegetables like broccoli or carrots helps maintain moisture and nutrients, while keeping the preparation simple.
Meal Timing and Portion Control
Managing gastroparesis often involves careful attention to meal timing and portion sizes. Consistent eating patterns can significantly reduce symptoms like nausea, vomiting, and bloating. By understanding how your body reacts to food, you can tailor your eating habits to minimize discomfort and maximize nutrient intake.The key to managing gastroparesis through meal timing and portion control lies in providing your digestive system with manageable amounts of food at regular intervals.
This approach helps prevent the stomach from becoming overloaded, allowing for more efficient digestion and absorption.
Importance of Meal Timing
Consistent meal times help regulate your digestive system’s rhythm. Your body develops a pattern of releasing digestive enzymes and acids, which aids in breaking down food. By eating at roughly the same times each day, you support this natural process and improve overall digestive efficiency.
Importance of Portion Size
Smaller, more frequent meals are crucial for managing gastroparesis. Large meals can overwhelm the stomach, causing delayed emptying and triggering symptoms. Breaking down meals into smaller portions allows for better digestion and prevents the stomach from becoming overly full.
Sample Meal Plan
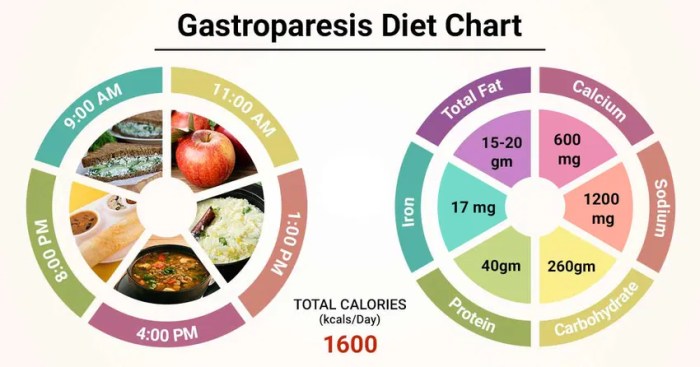
This sample meal plan demonstrates a strategy for smaller, more frequent meals, designed to accommodate the needs of someone with gastroparesis. Adjust portion sizes and meal times to your personal tolerance and needs.
- Breakfast (7:00 AM): 1/2 cup oatmeal with 1/4 cup berries and 1/4 cup plain yogurt. A small glass of milk.
- Mid-morning Snack (10:00 AM): 1/4 cup of nuts, or 1/2 apple slices with 1 tablespoon of peanut butter.
- Lunch (1:00 PM): 4 ounces grilled chicken breast with 1/2 cup of steamed vegetables and a small portion of brown rice (about 1/2 cup).
- Afternoon Snack (4:00 PM): 1/2 cup cottage cheese with a few slices of cucumber.
- Dinner (7:00 PM): 3 ounces lean fish (like cod or tilapia) with 1/2 cup of mixed greens and 1/4 cup of quinoa.
- Evening Snack (9:00 PM): 1/4 cup of low-sugar pudding or a small portion of protein shake.
Rationale for Smaller, More Frequent Meals
Breaking down meals into smaller, more frequent portions helps to:
- Prevent stomach overload.
- Reduce the risk of nausea and vomiting.
- Improve digestive efficiency.
- Maintain stable blood sugar levels.
Adjusting Meal Times
Adjusting meal times is a crucial part of personalizing your gastroparesis management plan. Pay close attention to how your body reacts to different meal schedules.
- Early Morning Sickness: If you experience early morning nausea, try shifting your first meal to a later time (e.g., 8:00 AM instead of 7:00 AM). You may need to adjust this to find a time that works for your body.
- Symptoms at Specific Times: If symptoms are triggered at certain times of the day, try shifting meals to earlier or later times to see if this helps manage your symptoms. Pay attention to how your body reacts and adjust as needed.
Meal Frequency Options
The following table Artikels various meal frequency options and their potential benefits. Note that these are examples and individual responses may vary.
Following a gastroparesis diet involves mindful choices about what you eat. Focus on smaller, more frequent meals, and avoid trigger foods like fatty or greasy options. Interestingly, studies on dietary habits often connect eating habits with overall health and longevity. For example, a recent article explored whether vegan diets might lead to longer lifespans and better aging, offering some compelling insights into the potential benefits of plant-based diets.
do vegans live longer and age better. Regardless of dietary choices, sticking to the right portions and avoiding foods that cause digestive distress remains key for managing gastroparesis symptoms.
| Meal Frequency | Potential Benefits |
|---|---|
| 6 small meals/day | Improved digestion, reduced stomach overload, potential for better blood sugar control. |
| 5 small meals/day | Balanced approach, allowing for flexibility, potentially reducing the burden of meal preparation. |
| 4 small meals/day | More time between meals, potentially better suited for individuals who struggle with frequent eating. |
Hydration Strategies

Staying hydrated is crucial for anyone with gastroparesis, but especially so for those experiencing delayed gastric emptying. Proper hydration helps to prevent dehydration, which can worsen symptoms and lead to further complications. Adequate hydration also supports digestion, nutrient absorption, and overall well-being.Maintaining a consistent fluid intake is key to managing symptoms and supporting the body’s functions. This includes careful consideration of the types of beverages consumed, and the timing of those beverages relative to meals.
Importance of Hydration
Proper hydration is essential for gastroparesis patients due to the impact of delayed gastric emptying on fluid absorption and overall bodily function. Dehydration can exacerbate nausea, vomiting, and abdominal pain. Furthermore, proper hydration helps to maintain blood volume and electrolyte balance, which is crucial for overall health and managing the symptoms associated with gastroparesis.
Appropriate Beverages for Consumption
Choosing the right beverages is a critical component of managing hydration in gastroparesis. Avoid sugary drinks, carbonated beverages, and very cold or very hot liquids, as these can exacerbate symptoms. Clear, colorless, and easily digestible fluids are preferable.
Preventing Dehydration and Managing Thirst
Consistent fluid intake throughout the day is vital. Carry a water bottle and sip on it regularly, even when not feeling thirsty. Thirst is often a late indicator of dehydration. Setting reminders on your phone or using a hydration tracker can help to maintain a consistent schedule. It’s important to note that consuming too much fluid too quickly can also be problematic.
Recommended Fluids and their Impact on Gastric Emptying
| Fluid | Impact on Gastric Emptying | Considerations |
|---|---|---|
| Water | Generally well-tolerated and does not significantly impact gastric emptying. | Best choice for most patients. |
| Clear broths (chicken, vegetable) | Can be well-tolerated, especially if low in sodium. | Good source of electrolytes if low sodium is considered. |
| Diluted fruit juices (apple, white grape) | May be tolerated in very small amounts, but can be problematic for some. | High sugar content can lead to digestive issues. |
| Herbal teas (ginger, chamomile) | Generally well-tolerated, though some may cause discomfort. | Consider the specific ingredients and how they affect individual patients. |
| Electrolyte solutions (pedialyte) | Can be beneficial for replacing lost electrolytes. | Follow package directions carefully. |
Hydrating Recipes and Combinations
A variety of hydrating recipes and combinations can be beneficial. For example, a simple mix of water, a small amount of lemon juice, and a pinch of salt can provide electrolytes and flavor without triggering digestive distress. Another option is a clear broth with a few slices of cucumber or a small piece of ginger. Important note: always adjust the recipe based on your personal tolerance.
Managing Symptoms and Potential Complications
Navigating gastroparesis requires understanding how to manage symptoms effectively and proactively address potential complications. This involves dietary adjustments, recognizing early warning signs, and developing strategies to prevent problems. By understanding the interplay between diet and gastroparesis, individuals can significantly improve their quality of life and overall well-being.
Managing Common Symptoms
Gastroparesis symptoms like nausea, vomiting, and bloating can be significantly impacted by dietary choices. Small, frequent meals are crucial, as large meals can overwhelm the digestive system. Avoiding trigger foods and incorporating strategies to improve digestion are key elements of symptom management. Liquids should be taken separately from meals, as combining them can worsen symptoms. Moreover, slow chewing and mindful eating can assist in smoother digestion.
Potential Complications of Poor Dietary Management
Poorly managed gastroparesis can lead to a cascade of complications. Dehydration, malnutrition, and electrolyte imbalances are significant concerns. Delayed gastric emptying can lead to nutrient deficiencies, impacting overall health. Repeated vomiting can cause electrolyte imbalances, requiring medical attention. Furthermore, prolonged malnutrition can weaken the immune system, making individuals more susceptible to infections.
Following a gastroparesis diet is all about mindful eating, focusing on easily digestible foods. While specific foods vary, the key is to avoid those that can trigger nausea or discomfort. For example, consider exploring the soothing effects of certain foods on IBS symptoms; check out this helpful guide on 6 foods to help soothe IBS symptoms naturally for some delicious options that might also benefit your gastroparesis.
Ultimately, experimenting with different foods and tracking how your body reacts is crucial for creating a personalized gastroparesis-friendly meal plan.
Identifying Early Signs of Complications
Recognizing early warning signs of complications is vital for timely intervention. Changes in bowel habits, such as constipation or diarrhea, are potential indicators. Persistent or worsening nausea and vomiting, along with a significant decrease in appetite, should be addressed promptly. Weight loss, fatigue, and dizziness are also red flags that warrant medical evaluation. Regular monitoring of symptoms and seeking medical attention when needed is paramount.
Strategies for Preventing and Managing Potential Complications
Implementing preventive measures and developing strategies for managing complications is essential. Maintaining a consistent meal schedule and avoiding trigger foods are key preventative strategies. Small, frequent meals and appropriate hydration strategies can prevent dehydration and electrolyte imbalances. Managing stress levels through relaxation techniques can also mitigate symptom flare-ups. If complications arise, immediate medical intervention is crucial, as well as adherence to prescribed treatments and dietary guidelines.
Example Strategies for Managing Symptoms and Complications
To illustrate, consider a scenario where nausea and vomiting are significant symptoms. Implementing a bland diet, consisting of easily digestible foods, can help. Smaller portions, taken frequently, can lessen the burden on the digestive system. Maintaining adequate hydration by sipping clear liquids throughout the day, rather than large quantities at once, is important. If symptoms worsen, immediate medical attention is required.
Table of Potential Gastroparesis Complications and Dietary Recommendations
| Potential Gastroparesis Complication | Dietary Recommendations |
|---|---|
| Dehydration | Frequent small sips of clear liquids, avoiding sugary drinks. |
| Malnutrition | Focus on nutrient-dense foods; consult a registered dietitian for personalized meal plans. |
| Electrolyte Imbalance | Include foods rich in electrolytes (potassium, sodium, magnesium) like bananas, potatoes, and leafy greens. Consult a doctor about electrolyte supplements. |
| Weight Loss | Increase calorie intake through nutrient-dense foods; avoid processed foods and sugary drinks. |
| Constipation | Increase fiber intake gradually, ensuring adequate hydration; consult a doctor if constipation persists. |
| Diarrhea | Consume easily digestible foods; avoid trigger foods. Maintain hydration with clear liquids. |
Practical Tips and Strategies
Navigating the gastroparesis diet can feel like a constant balancing act. It’s not just about what you eat, but also how you eat it. This section dives into practical strategies to make mealtimes easier and more manageable, focusing on preparation, managing challenges, and adapting to your unique needs.
Meal Preparation Strategies
Effective meal preparation is key to maintaining a gastroparesis diet. Pre-planning and prepping ingredients significantly reduces stress and ensures you have healthy, easily digestible meals on hand. Batch cooking meals for the week can save time and effort, especially when you are managing symptoms.
- Portion Control: Using smaller plates and bowls helps with portion control, reducing the volume of food consumed at each sitting. This minimizes the strain on your digestive system and can improve overall symptom management. A visual cue can be helpful in portioning out meals.
- Meal Timing and Spacing: Eating smaller meals and snacks throughout the day, rather than three large meals, can reduce the amount of food your stomach needs to process at one time. Regular meal timing and snack schedules create a consistent digestive pattern, which is particularly helpful in minimizing symptoms. This approach can significantly improve comfort and reduce the risk of experiencing discomfort from overeating.
- Food Texture Modification: Many gastroparesis sufferers find it easier to digest foods in a pureed or blended form. Pureeing soups, stews, and even fruits and vegetables can make them easier to eat and digest. Some people benefit from using food processors or blenders to create smooth textures.
Managing Mealtime Challenges
Gastroparesis can present unique challenges during mealtimes. Understanding these challenges and employing effective strategies can significantly improve the experience.
- Managing Nausea and Vomiting: Eating slowly and in small portions, avoiding greasy or fatty foods, and eating in a quiet, calm environment can help minimize nausea. Keeping ginger candies or ginger tea readily available can be beneficial. Certain foods, such as spicy or acidic ones, may worsen symptoms.
- Addressing Bloating and Discomfort: Limiting high-fiber foods and gas-producing foods, such as beans, broccoli, and cabbage, can help reduce bloating. Choosing low-fiber options, such as well-cooked or mashed vegetables, can minimize gas production and discomfort.
Adapting Recipes for a Gastroparesis Diet
The good news is that you can still enjoy delicious meals while following a gastroparesis diet. Creative adjustments can make your favorite dishes more manageable.
- Substituting Ingredients: Try replacing whole grains with finely ground grains or pureed options. Using pureed or blended vegetables in place of raw or whole vegetables can greatly improve digestive comfort. If a recipe calls for a specific type of fruit, try blending it or using pureed versions of that fruit.
- Modifying Cooking Methods: Many traditional cooking methods, such as frying, can be replaced with gentler alternatives. Baking, steaming, or poaching can often be just as flavorful and more gentle on the digestive system.
Managing Cravings and Emotional Eating
Emotional eating can be a significant challenge for anyone, but it can be particularly difficult for those with gastroparesis. Addressing the underlying emotional factors is key to managing cravings effectively.
- Identifying Triggers: Pay close attention to situations or emotions that trigger cravings. Journaling can be helpful in identifying patterns. This can provide insights into the root causes of your cravings, enabling more targeted strategies for managing them.
- Developing Healthy Coping Mechanisms: Engage in activities that bring you joy and help you manage stress, such as exercise, meditation, or spending time in nature. Exploring these alternative ways to cope with difficult emotions can help you manage cravings more effectively.
Common Cooking Methods Suitable for Gastroparesis Diets
| Cooking Method | Description | Suitability for Gastroparesis |
|---|---|---|
| Baking | Cooking in an oven | Excellent, allows for control over temperature and moisture |
| Steaming | Cooking over hot water | Excellent, preserves nutrients and avoids added fats |
| Poaching | Cooking in a liquid | Good, gentle cooking method for delicate ingredients |
| Pureeing/Blending | Turning food into a smooth consistency | Very Good, ideal for improving digestibility |
| Broiling | Cooking under a direct heat source | Moderate, potential for overcooking |
| Pan-frying | Cooking in a pan with oil | Moderate, limit oil and use gentle heat |
Dietary Adjustments for Specific Situations
Navigating a gastroparesis diet can feel like a balancing act, especially when faced with social events, travel, or unexpected situations. Flexibility and adaptability are key to managing symptoms and maintaining a healthy lifestyle. This section explores strategies for adjusting your dietary plan to accommodate various circumstances.
Holiday Meals
Holiday gatherings often present challenges due to tempting, rich foods and unfamiliar meal arrangements. Understanding the potential triggers and preparing in advance can minimize discomfort. For example, choosing smaller portions of dishes with higher fat or sugar content is crucial. Consider bringing a dish you know you can easily manage or a healthy alternative if you’re able.
Travel
Traveling can disrupt meal routines and access to familiar, gastroparesis-friendly foods. Pre-planning is essential. Pack familiar snacks and meals that you can easily reheat or consume. Research restaurants beforehand, noting their ability to offer suitable options. Have a backup plan for unexpected delays or changes in your travel schedule.
For instance, when traveling internationally, it’s important to be aware of potential food allergies or unfamiliar ingredients. Having an emergency kit with easily digestible snacks and electrolyte drinks can also be helpful.
Social Gatherings
Social events often involve shared meals, potentially making it difficult to maintain a gastroparesis-friendly diet. Communicate your dietary needs to hosts or companions in advance. Offer to bring a dish that aligns with your restrictions, or suggest alternatives to dishes you might otherwise avoid. Practice assertive communication, while remaining polite and understanding.
Unexpected or Difficult Situations
Life throws curveballs, and a gastroparesis diet requires adaptability. If you experience unexpected nausea or vomiting, prioritize clear fluids, and rest. If a meal proves particularly problematic, don’t be afraid to modify your plan for the remainder of the day. Focus on getting appropriate nutrients and fluids without causing further distress.
Flexibility and Personalization
A rigid diet rarely works. A gastroparesis diet should be flexible and personalized. Listen to your body’s cues. Modify your plan based on how specific foods or meals affect you. Experiment with different foods, portion sizes, and meal timings to identify what works best.
A personalized approach allows you to enjoy a healthy lifestyle while managing your symptoms effectively.
Table: Common Dietary Challenges and Potential Solutions
| Dietary Challenge | Potential Solution |
|---|---|
| Holiday meals with rich foods | Choose smaller portions, select lower-fat/sugar options, bring a safe dish, or request modifications. |
| Travel disrupting meal routines | Pack familiar, easy-to-manage snacks and meals. Research restaurants beforehand. Have a backup plan. |
| Social gatherings with shared meals | Communicate dietary needs to hosts/guests. Offer to bring a safe dish, suggest alternatives, and practice assertive communication. |
| Unexpected nausea or vomiting | Prioritize clear fluids, rest, and modify your plan for the day. |
| Unfamiliar or problematic foods | Modify portion sizes or eliminate those foods from the meal plan. |
Final Thoughts
In conclusion, following a gastroparesis diet is a personalized journey that requires understanding your body’s unique needs. By carefully considering macronutrients, food choices, meal timing, and hydration, you can effectively manage your symptoms and improve your overall well-being. This comprehensive guide offers a roadmap for success, empowering you to make informed choices and live a fulfilling life with gastroparesis.

