How depression is treated sets the stage for this enthralling narrative, offering readers a glimpse into the multifaceted approaches to managing this challenging condition. From medication and therapy to lifestyle changes and support systems, this guide delves into the various strategies used to effectively treat depression. It’s a journey into understanding the diverse needs of individuals experiencing depression, emphasizing the importance of tailored treatment plans.
This exploration will cover a range of topics, from the different types of antidepressants and their mechanisms of action, to the various types of psychotherapy and their effectiveness. We’ll also discuss the crucial role of lifestyle modifications, complementary treatments, and the importance of combining different approaches for optimal results. The unique considerations for specific populations, such as adolescents and older adults, will also be addressed.
Finally, we’ll examine the critical role of monitoring and evaluating treatment effectiveness for a successful recovery.
Introduction to Depression Treatment
Depression is a serious mental health condition that affects millions worldwide. Effective treatment is crucial for improving quality of life and preventing long-term complications. Various approaches are employed, and successful outcomes often hinge on a personalized treatment plan tailored to the individual’s needs and preferences. Understanding the different types of depression, the various treatment modalities, and the importance of individualization is key to achieving positive outcomes.Different approaches are used to treat depression, recognizing the multifaceted nature of the condition.
These include medication, psychotherapy, lifestyle changes, and a combination of these approaches. The effectiveness of each method can vary significantly, and the optimal approach often depends on the specific type of depression and the individual’s response.
Types of Depression Commonly Treated
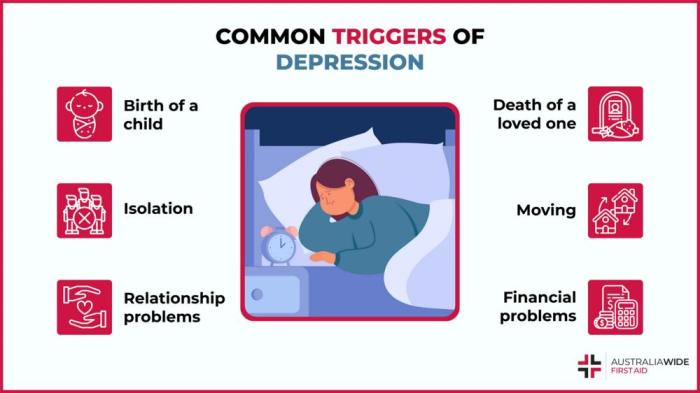
Depression manifests in diverse forms. Major Depressive Disorder (MDD) is the most common type, characterized by persistent sadness, loss of interest, and other symptoms. Persistent Depressive Disorder (Dysthymia) is a chronic form of depression, with symptoms lasting for at least two years. Other types, such as bipolar disorder, seasonal affective disorder (SAD), and postpartum depression, each have unique characteristics and require tailored treatment strategies.
Approaches to Depression Treatment
Treatment plans for depression are not one-size-fits-all. Individualized approaches consider the unique needs and preferences of each patient. Effective treatment often involves a combination of therapies, including medication, psychotherapy, and lifestyle changes. The selection of interventions is based on factors such as the severity of symptoms, the individual’s personal history, and preferences.
Importance of Individualized Treatment Plans
Treatment plans should be tailored to meet the specific needs of each individual. Factors like personal history, preferences, and cultural background should be taken into account. A collaborative approach, where the patient actively participates in decision-making, is crucial for achieving optimal outcomes. Open communication and trust between the patient and healthcare provider are essential for developing a successful treatment plan.
Common Factors Contributing to Effective Treatment
Several factors contribute to the effectiveness of depression treatment. These include a strong therapeutic alliance, adherence to the treatment plan, and a supportive environment. Early intervention, active participation from the patient, and regular follow-up appointments are vital for progress. The patient’s commitment to the treatment plan, alongside the support of loved ones and healthcare professionals, plays a significant role in successful recovery.
Comparison of Treatment Modalities
| Treatment Modality | Description | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Medication | Prescribed medications, such as antidepressants, to regulate brain chemistry. | Can rapidly alleviate symptoms in many cases, particularly for severe depression. | Potential side effects, including nausea, sleep disturbances, and sexual dysfunction. Not a quick fix, and may take several weeks to show effectiveness. |
| Psychotherapy | Various therapeutic approaches, such as cognitive behavioral therapy (CBT) and interpersonal therapy (IPT), to address thoughts, feelings, and behaviors. | Provides coping mechanisms and strategies to manage depression. Can help patients identify and address underlying issues. | May not be as effective as medication for severe depression, and can be time-consuming. |
| Lifestyle Changes | Modifications to daily routines, such as regular exercise, healthy diet, and sufficient sleep. | Can significantly improve mood and overall well-being. | Requires commitment and consistency. May not be sufficient for severe depression alone. |
Medication-Based Treatments
Medication plays a crucial role in managing depression, often used in conjunction with therapy and lifestyle changes. These medications, known as antidepressants, aim to restore the balance of neurochemicals in the brain, particularly serotonin, norepinephrine, and dopamine, which are linked to mood regulation. Finding the right medication and dosage is often a process of trial and error, and close monitoring by a healthcare professional is essential.Understanding the various types of antidepressants, their mechanisms of action, and potential side effects is key to making informed decisions about treatment.
This section delves into the specifics of medication-based approaches to depression, providing a comprehensive overview.
Types of Antidepressant Medications
Antidepressants are categorized into several classes, each with unique mechanisms of action. Understanding these classes is essential for navigating the treatment process. The selection of a specific antidepressant often depends on individual patient characteristics and the specific symptoms experienced.
- Selective Serotonin Reuptake Inhibitors (SSRIs): These medications, such as fluoxetine (Prozac) and sertraline (Zoloft), primarily affect serotonin levels by preventing its reabsorption into nerve cells. This allows more serotonin to remain in the synapse, potentially improving mood and reducing symptoms of depression.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Examples include venlafaxine (Effexor) and duloxetine (Cymbalta). SNRIs increase both serotonin and norepinephrine levels by blocking their reuptake. This dual action can potentially provide broader benefits for individuals experiencing more severe or complex symptoms.
- Tricyclic Antidepressants (TCAs): These older medications, such as amitriptyline and imipramine, affect serotonin and norepinephrine reuptake. While effective for some, their side effect profiles can be more extensive compared to newer classes, making them often less preferred for first-line treatment.
- Monoamine Oxidase Inhibitors (MAOIs): Phenelzine (Nardil) and tranylcypromine (Parnate) are examples. MAOIs work by inhibiting the enzyme monoamine oxidase, which breaks down neurotransmitters. This increases the availability of neurotransmitters like norepinephrine and serotonin, potentially improving mood. Due to their potential for serious interactions with certain foods and medications, MAOIs are typically reserved for cases where other antidepressants have been ineffective.
Mechanisms of Action
The specific mechanisms of action differ across antidepressant classes, but generally, these medications aim to increase the availability of neurotransmitters in the synaptic cleft. This enhanced availability can potentially lead to improved mood regulation and a reduction in depressive symptoms. For example, SSRIs block the reuptake of serotonin, leaving more serotonin available to bind to receptors on nerve cells.
Effectiveness and Side Effects, How depression is treated
The effectiveness of antidepressants varies from person to person. Some individuals may experience significant symptom reduction, while others may require adjustments in dosage or switching to a different class of medication. Factors such as the severity of depression, individual physiology, and co-occurring conditions can all influence treatment response.
- Side effects are a significant consideration. Common side effects can include nausea, insomnia, sexual dysfunction, and weight changes. It is essential to discuss these potential side effects with a healthcare provider and carefully monitor for any adverse reactions.
Importance of Adherence to Medication Regimens
Consistent adherence to the prescribed medication regimen is crucial for achieving optimal results. Skipping doses or discontinuing treatment prematurely can hinder the effectiveness of the medication and potentially lead to a relapse of depressive symptoms. It’s important to communicate openly with a healthcare provider about any challenges in maintaining adherence.
Potential Side Effects of Common Antidepressants
| Antidepressant Class | Common Side Effects |
|---|---|
| SSRIs | Nausea, insomnia, sexual dysfunction, headache, anxiety |
| SNRIs | Nausea, sweating, insomnia, sexual dysfunction, increased blood pressure |
| TCAs | Dry mouth, constipation, blurred vision, drowsiness, weight gain |
| MAOIs | Headache, dizziness, nausea, insomnia, potentially serious interactions with certain foods and medications |
Duration of Treatment
The duration of treatment varies significantly depending on the individual and the severity of the depression. Some individuals may experience improvement within a few weeks, while others may require months or even years of treatment. The decision about the duration of treatment should be made in consultation with a healthcare provider.
Treating depression often involves therapy, medication, and lifestyle changes. Learning how to support someone struggling with their mental health is crucial, and this extends to understanding proper physical support. Knowing how to lift a person safely here is just as important as knowing how to offer emotional support. Ultimately, a holistic approach that combines professional help with personal care is key to effectively managing depression.
| Antidepressant Class | Typical Treatment Duration |
|---|---|
| SSRIs/SNRIs | Typically 6-12 months or longer, depending on individual needs. |
| TCAs | Often longer than SSRIs or SNRIs, potentially for several months or years. |
| MAOIs | Usually considered for long-term management, depending on the individual’s response and health status. |
Psychotherapy Approaches
Psychotherapy plays a crucial role in treating depression, offering a supportive and structured environment for individuals to understand and manage their condition. It focuses on addressing the underlying emotional, behavioral, and cognitive factors contributing to depression, providing coping mechanisms and strategies for long-term well-being. Unlike medication, which primarily targets the biological aspects of depression, psychotherapy delves into the psychological realm, empowering individuals to actively participate in their recovery.Beyond medication, psychotherapy provides a valuable avenue for exploring the root causes of depression.
This exploration often involves identifying negative thought patterns, challenging unhelpful beliefs, and developing healthier coping mechanisms. By working with a therapist, individuals can gain insight into their emotions, improve interpersonal relationships, and build resilience to future stressors.
Common Types of Psychotherapy for Depression
Various types of psychotherapy are effective in treating depression, each with its own unique principles and techniques. These approaches address different aspects of the condition, tailoring strategies to individual needs. Understanding the strengths and limitations of each type can aid in selecting the most suitable approach for a particular individual.
- Cognitive Behavioral Therapy (CBT): CBT is a widely used and highly effective psychotherapy approach for depression. It emphasizes the connection between thoughts, feelings, and behaviors. CBT aims to identify and modify negative thought patterns that contribute to depressive symptoms. CBT techniques, such as cognitive restructuring and behavioral activation, equip individuals with tools to challenge negative thought patterns and engage in activities that promote well-being.
- Interpersonal Therapy (IPT): IPT focuses on improving interpersonal relationships and resolving conflicts that may contribute to or exacerbate depressive symptoms. This therapy helps individuals identify patterns in their relationships that may be problematic and develop effective communication and conflict resolution skills. IPT emphasizes the role of social support and healthy relationships in mental well-being.
- Psychodynamic Therapy: Psychodynamic therapy delves into unconscious patterns and past experiences to understand the origins of depression. It explores how past relationships and unresolved conflicts may be influencing current emotional states and behaviors. This therapy aims to enhance self-awareness and facilitate emotional processing to reduce the impact of past experiences on current difficulties.
- Acceptance and Commitment Therapy (ACT): ACT helps individuals accept their thoughts and feelings without judgment, while simultaneously committing to values-driven actions. This approach emphasizes mindfulness and self-compassion to foster psychological flexibility and reduce the impact of negative thoughts and emotions on behavior.
Specific Techniques in Different Therapies
Specific techniques vary across different psychotherapy approaches. Each technique aims to address different aspects of the individual’s experience with depression.
- Cognitive Restructuring (CBT): This involves identifying and challenging negative automatic thoughts, replacing them with more realistic and positive ones. A common example might be challenging the thought “I’m a complete failure” by identifying specific instances where the person has succeeded.
- Behavioral Activation (CBT): This technique involves increasing engagement in pleasurable activities and rewarding behaviors, regardless of mood. This can help break the cycle of inactivity and low motivation associated with depression.
- Interpersonal Problem-Solving (IPT): This technique focuses on teaching effective communication and problem-solving skills to improve relationships. It often involves role-playing and practicing new communication strategies.
- Mindfulness (ACT): This involves paying attention to the present moment without judgment. Mindfulness practices, such as meditation, can help individuals become more aware of their thoughts and feelings, fostering a sense of detachment and acceptance.
Effectiveness of Psychotherapy Approaches
The effectiveness of different psychotherapy approaches varies depending on the individual and the specific type of depression. For example, CBT is often highly effective for treating major depressive disorder characterized by negative thought patterns. IPT can be particularly beneficial for individuals experiencing depression related to interpersonal difficulties. Psychodynamic therapy may be suitable for individuals with complex or long-standing depressive symptoms, exploring deeper unconscious issues.
Therapist Specialties
| Therapist Type | Specialties |
|---|---|
| Cognitive Behavioral Therapist (CBT) | Depression, anxiety, stress management, relationship issues |
| Interpersonal Therapist (IPT) | Depression, relationship problems, grief, social anxiety |
| Psychodynamic Therapist | Personality disorders, trauma, long-standing emotional issues |
| Acceptance and Commitment Therapist (ACT) | Anxiety, depression, stress, chronic pain |
Lifestyle and Complementary Treatments: How Depression Is Treated
Beyond medication and therapy, lifestyle modifications play a crucial role in managing depression. Adopting healthy habits can significantly improve mood and overall well-being, often acting as powerful adjuncts to formal treatments. These lifestyle changes, when integrated into a comprehensive treatment plan, can lead to more sustainable improvements and a higher quality of life for individuals experiencing depression.Lifestyle interventions are not a replacement for professional care but rather a supportive component.
By focusing on diet, exercise, sleep, and stress management, individuals can create a foundation for resilience and mental well-being, making them better equipped to navigate the challenges of depression.
The Role of Exercise in Depression Management
Regular physical activity has demonstrably positive effects on mood and mental health. Exercise releases endorphins, which have mood-boosting properties, and it can also improve sleep quality and reduce stress. Finding activities you enjoy, whether it’s dancing, swimming, hiking, or team sports, is key to maintaining consistency. Even moderate-intensity exercise can be beneficial. Studies show that consistent exercise can lessen depressive symptoms and enhance overall emotional regulation.
The Importance of Nutrition in Depression
A balanced diet rich in fruits, vegetables, whole grains, and lean proteins is crucial for both physical and mental health. Nutrient deficiencies can contribute to mood changes. A healthy diet can improve energy levels, reduce inflammation, and provide essential nutrients that support brain function. Avoiding processed foods, sugary drinks, and excessive caffeine can help stabilize mood and energy levels.
Treating depression often involves a combination of therapies, like talk therapy and medication. Understanding the complexities of the human brain, particularly how things like the nucleus pulposus, a key component of the spine, might influence overall well-being, is crucial for effective treatment. Different approaches like cognitive behavioral therapy and medication can be employed to help manage the symptoms and promote recovery, but the specifics will vary from person to person.
Ultimately, the goal of treatment is to empower individuals to manage their mental health effectively and create a path toward well-being. Learning more about the role of the spine and its structures like the nucleus pulposus can provide a better understanding of the body’s intricate workings.
Proper nutrition can be an essential support in the fight against depression.
The Significance of Sleep Hygiene in Depression
Adequate sleep is essential for emotional regulation and overall well-being. Poor sleep can worsen depressive symptoms. Establishing a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a dark, quiet, and comfortable sleep environment are important steps in improving sleep quality. Addressing underlying sleep disorders like insomnia can also significantly contribute to mood stabilization.
Complementary and Alternative Medicine Approaches
Complementary and alternative medicine (CAM) approaches, such as yoga, meditation, and mindfulness, can be valuable adjuncts to conventional treatments. These practices can help manage stress, improve emotional regulation, and promote relaxation. It’s essential to consult with a healthcare professional before incorporating CAM into a treatment plan, particularly if you are taking other medications. Careful consideration and consultation with a healthcare professional are crucial for integrating CAM safely and effectively.
Treating depression often involves therapy, medication, and lifestyle changes. Finding healthy ways to manage late-night cravings can be really important for overall well-being, and healthy late night snacks can help you avoid unhealthy options and support a balanced diet. Ultimately, a holistic approach, including these lifestyle choices, plays a key role in effective depression treatment.
Specific Lifestyle Modifications for Depression Support
| Activity | Description |
|---|---|
| Mindfulness and Meditation | Practicing mindfulness involves focusing on the present moment without judgment. Meditation techniques can help reduce stress and promote emotional regulation. |
| Yoga | Yoga combines physical postures, breathing techniques, and meditation to improve flexibility, balance, and mental clarity. |
| Spending Time in Nature | Exposure to nature has been linked to reduced stress and improved mood. Taking walks in parks or spending time outdoors can be beneficial. |
| Social Connection | Maintaining strong social connections and engaging in meaningful relationships is crucial for mental well-being. Connecting with friends, family, or support groups can offer emotional support and a sense of belonging. |
| Creative Expression | Engaging in creative activities like painting, writing, or music can be a powerful way to express emotions and manage stress. |
Importance of Patient Self-Care in Depression Management
Self-care is vital in managing depression. It involves taking proactive steps to prioritize your physical and emotional well-being. This includes acknowledging and addressing your needs, setting boundaries, and practicing self-compassion. Prioritizing your well-being, even during challenging times, is an essential part of effective self-management of depression.
Combining Treatments
Treating depression effectively often requires a multifaceted approach. A personalized treatment plan that combines different strategies can significantly improve outcomes. This approach acknowledges the complexity of the condition and tailors interventions to address specific needs and symptoms.Combining treatments is not merely adding therapies together; it’s a carefully orchestrated strategy designed to maximize benefits and minimize risks. Understanding the rationale behind combining approaches, recognizing potential interactions, and tailoring the plan to individual needs are crucial for successful outcomes.
Rationale for Combining Treatments
Depression’s complexity often necessitates a combination of therapies. Symptoms can manifest in various ways, affecting different aspects of a person’s life. A single approach might not adequately address all facets of the condition. Combining treatments can target different aspects of the disorder, potentially leading to a more comprehensive and effective response.
Potential Benefits and Challenges of Combining Medication and Psychotherapy
Combining medication and psychotherapy offers significant potential benefits. Medication can help regulate neurochemicals, alleviating severe symptoms like persistent sadness and anhedonia, enabling individuals to engage more effectively in therapeutic interventions. Psychotherapy, in turn, provides coping mechanisms, addresses underlying issues, and fosters positive lifestyle changes.However, combining these approaches presents challenges. Potential drug interactions must be carefully considered and monitored.
For example, some antidepressants can affect sleep, which might impact the effectiveness of certain types of psychotherapy that involve evening sessions. Additionally, patients might experience side effects from medication that can impact their motivation to engage in therapy. Careful monitoring, open communication, and a collaborative approach between the healthcare team and the patient are essential to mitigate these potential difficulties.
Tailoring a Treatment Plan to Individual Needs
A successful treatment plan requires a thorough assessment of the individual’s specific needs and circumstances. Factors such as the severity of symptoms, personal history, and preferences should all be considered. For example, a patient with severe anxiety might benefit from a combination of medication to manage anxiety and cognitive behavioral therapy (CBT) to develop coping mechanisms. A patient with milder symptoms and a strong desire for lifestyle changes might focus on lifestyle modifications and support groups.
The ultimate goal is to create a plan that is not only effective but also sustainable and manageable for the individual.
Examples of Successful Combination Therapies
Numerous case studies and clinical trials demonstrate the efficacy of combined treatments. One example involves a patient with major depressive disorder who responded well to a combination of selective serotonin reuptake inhibitors (SSRIs) and cognitive behavioral therapy (CBT). CBT helped the patient identify and challenge negative thought patterns, while the medication managed their depressive symptoms, allowing for a more focused and positive therapeutic environment.
Another example might be the use of interpersonal therapy (IPT) alongside medication to address relationship difficulties that are contributing to the depressive symptoms.
Importance of Collaboration Between Healthcare Professionals
Effective combination therapy relies heavily on collaboration between various healthcare professionals. Psychiatrists, psychologists, therapists, and other relevant professionals need to communicate openly and share information to ensure a cohesive and coordinated approach. This includes regular communication about treatment progress, side effects, and any adjustments needed to the plan. Open communication is essential for creating a unified front to support the patient’s recovery.
Potential Interactions Between Treatment Modalities
| Treatment Modality 1 | Treatment Modality 2 | Potential Interactions | Example |
|---|---|---|---|
| Medication (e.g., SSRIs) | Psychotherapy (e.g., CBT) | Medication can influence therapy engagement and vice-versa; side effects may affect therapy adherence. | Medication-induced fatigue might reduce motivation for CBT sessions. |
| Lifestyle Changes (e.g., Exercise) | Psychotherapy (e.g., Mindfulness-Based Cognitive Therapy) | Lifestyle changes can enhance the effectiveness of therapy; therapy can provide motivation and structure for lifestyle changes. | Exercise can improve mood and energy, which in turn can make mindfulness practices more effective. |
| Medication (e.g., Mood Stabilizers) | Psychoeducation | Medication may stabilize mood, enabling clearer understanding of the condition and treatment. | Understanding the impact of mood swings on daily life is easier with medication-stabilized mood. |
Treatment Considerations for Specific Populations
Navigating the complexities of depression requires a nuanced approach, recognizing that individuals experience the condition differently based on factors like age, cultural background, and life circumstances. Effective treatment strategies must consider these unique needs to ensure optimal outcomes. This section delves into the specific considerations for various populations, highlighting the importance of tailoring interventions to address individual experiences and challenges.
Adolescent Depression
Adolescents face unique developmental and social pressures that can significantly impact their experience with depression. Treatment strategies must be adapted to address these developmental hurdles, fostering a supportive and understanding environment. Therapeutic approaches should incorporate family involvement and focus on building coping mechanisms and resilience. It’s crucial to consider the influence of peer relationships and social media on the adolescent’s emotional well-being.
Early intervention and preventative measures are paramount in this critical period of development. The adolescent brain is still developing, impacting how they respond to treatment.
Older Adult Depression
Older adults may experience depression differently than younger populations, potentially influenced by physical health conditions, social isolation, and loss. Treatment approaches should prioritize addressing co-occurring medical conditions and considering the impact of age-related cognitive changes. Cognitive-behavioral therapy (CBT) and interpersonal therapy (IPT) can be highly effective, but modifications might be necessary to accommodate any physical limitations. Medication management should carefully consider potential drug interactions with other medications.
Emphasis on social support and maintaining social connections is essential.
Cultural Considerations
Cultural background significantly influences treatment preferences and responses to depression. Different cultures may have varying beliefs about mental illness, impacting willingness to seek help and preferred treatment modalities. It’s crucial for clinicians to be culturally sensitive and aware of potential barriers to accessing care. The approach should be tailored to respect cultural values and beliefs. Treatment should include culturally appropriate support systems and resources.
Clinicians should actively seek training in cultural competency to effectively address the needs of diverse populations.
Depression During Pregnancy and Postpartum
Pregnancy and the postpartum period are particularly vulnerable times for developing or experiencing depression. Hormonal fluctuations, physical changes, and the transition to motherhood contribute to a heightened risk. Treatment plans must prioritize the safety of both the mother and the developing fetus. Psychotherapy, particularly supportive therapy, is often a cornerstone of treatment, while medication should be carefully considered.
Addressing the emotional needs of the infant or young child is also essential. Close monitoring of the mother’s mental health is critical throughout this period.
Role of Support Systems
Strong support systems play a crucial role in managing depression for individuals across all populations. Family, friends, and community resources can provide emotional support, practical assistance, and a sense of belonging. Encouraging individuals to connect with their support networks is vital. Building and utilizing these networks can significantly enhance treatment outcomes and promote recovery. Recognizing and utilizing available support groups, whether online or in-person, can also be valuable.
Resources for Diverse Populations
| Population | Potential Barriers | Resources |
|---|---|---|
| Adolescents | Stigma, lack of awareness, access to care | School counselors, community mental health centers, online support groups, crisis hotlines |
| Older Adults | Transportation limitations, financial constraints, social isolation | Senior centers, community health programs, home-based services, support groups |
| Individuals from diverse cultural backgrounds | Cultural stigma, language barriers, lack of culturally competent providers | Culturally specific organizations, community health workers, bilingual therapists, interpreter services |
| Pregnant and postpartum women | Fear of medication effects on fetus, lack of support, financial barriers | Maternal health clinics, perinatal mental health specialists, support groups, social work services |
Monitoring and Evaluation of Treatment

Ongoing monitoring is crucial for adapting depression treatment to individual needs and ensuring optimal outcomes. Regular assessment allows therapists and patients to track progress, identify roadblocks, and make necessary adjustments to the treatment plan. This dynamic process ensures the treatment remains effective and tailored to the evolving needs of the person experiencing depression.
Importance of Ongoing Monitoring
Effective treatment for depression requires continuous evaluation of its impact. Monitoring allows for timely interventions to address emerging challenges or adjust the treatment approach. This proactive approach ensures that the treatment plan remains relevant and effective throughout the therapeutic journey. A lack of monitoring can lead to treatment stagnation or even setbacks, highlighting the vital role of ongoing evaluation.
Methods for Tracking Progress
Several methods are used to track the effectiveness of depression treatment. These include regular check-ins with the therapist, self-reporting questionnaires, and standardized clinical assessments. By combining these approaches, a comprehensive picture of the patient’s progress emerges. A multi-faceted approach provides a more complete and reliable understanding of treatment efficacy.
Role of Patient Self-Reporting and Professional Assessments
Patient self-reporting, through questionnaires and diaries, provides valuable insights into mood changes, symptom severity, and overall well-being. This subjective data, combined with professional assessments, paints a more complete picture of treatment effectiveness. Professional assessments provide objective data that complements the patient’s subjective experience, ensuring a balanced evaluation.
Indicators of Treatment Success or Failure
Indicators of treatment success include a significant reduction in depressive symptoms, improved functional capacity, increased engagement in activities, and a higher overall quality of life. Conversely, indicators of treatment failure might include persistent or worsening symptoms, lack of response to treatment, and decreased engagement in life. These markers help determine the efficacy of the current treatment and guide adjustments.
Evaluating Treatment Outcomes
Evaluating treatment outcomes involves a systematic approach. Therapists and patients work collaboratively to assess the progress made in addressing the identified symptoms and overall well-being. This involves analyzing self-reported data, professional assessments, and tracking any changes in daily functioning. Through this systematic process, both parties can assess the effectiveness of the intervention.
Summary Table of Evaluation Tools
| Evaluation Tool | Application | Strengths | Limitations |
|---|---|---|---|
| Beck Depression Inventory (BDI-II) | Assessing the severity of depressive symptoms. | Well-established, reliable, and widely used. | May not capture all aspects of depression, and results can be influenced by social desirability bias. |
| Hamilton Rating Scale for Depression (HAM-D) | Assessing severity of depressive symptoms in a clinical setting. | Provides a comprehensive measure of various depressive symptoms. | Requires a clinician’s expertise for administration and interpretation. |
| Patient Health Questionnaire-9 (PHQ-9) | Screening and monitoring depressive symptoms in primary care settings. | Easy to administer and score, widely accessible. | May not be as comprehensive as other scales for specific symptom analysis. |
| Clinical Global Impression-Severity (CGI-S) | Assessing the overall severity of a patient’s condition. | Provides a general overview of the patient’s status. | Subjective rating; clinician bias can influence the score. |
Wrap-Up
In conclusion, treating depression requires a holistic and individualized approach. This guide has highlighted the various treatment modalities, from medication and psychotherapy to lifestyle adjustments and support systems. The key takeaway is that effective treatment often involves a combination of strategies tailored to the individual’s specific needs and preferences. Remember, seeking professional help is crucial, and open communication with healthcare providers is essential for navigating this journey toward recovery.

