Gait training in physical therapy focuses on restoring and improving normal walking patterns. It’s crucial for daily life, impacting everything from mobility to overall health. Physical therapists address a wide range of gait abnormalities, tailoring interventions to specific needs. This comprehensive guide explores the entire process, from assessment and evaluation to interventions, patient selection, and measuring outcomes.
Understanding the historical evolution of gait training techniques and the diverse types of gait abnormalities is essential for therapists. The guide delves into the various methods of assessment, from standardized protocols to the use of advanced tools. It also explores the critical role of patient history and factors contributing to gait impairments. The importance of individualized programs and patient motivation is highlighted.
Introduction to Gait Training in Physical Therapy
Gait training in physical therapy is a specialized area focused on improving or restoring an individual’s ability to walk. It involves a comprehensive assessment, intervention, and rehabilitation process tailored to address specific gait impairments. This approach emphasizes restoring normal movement patterns and function, enhancing overall mobility, and improving the quality of life for patients.Gait is fundamental to daily activities, enabling us to perform tasks from simple movements like getting to the kitchen to more complex actions like climbing stairs or navigating challenging terrain.
A healthy gait is essential for maintaining independence, social participation, and overall well-being. Impairments in gait can significantly impact a person’s ability to perform these activities, potentially leading to isolation, reduced participation in social activities, and increased risk of falls.
Gait training in physical therapy is crucial for restoring mobility and balance, especially for those with underlying health conditions. Factors like high blood pressure can significantly impact walking patterns, and understanding its causes is key for effective treatment. High blood pressure causes can range from lifestyle choices to underlying health issues, all of which can influence the way a person walks.
Ultimately, effective gait training programs need to consider these factors and tailor exercises to each individual’s needs.
Significance of Gait in Daily Activities
Normal gait is crucial for numerous daily activities. Walking is vital for transportation, social interaction, and participation in recreational activities. It allows individuals to perform tasks ranging from shopping to engaging in hobbies. Without a functional gait, many daily activities become difficult or impossible.
Types of Gait Abnormalities
Physical therapists address a wide range of gait abnormalities, each with unique characteristics and underlying causes. These include, but are not limited to, steppage gait, where the foot slaps the ground, and foot drop, where the foot drags. Other gait deviations include compensatory patterns, such as a Trendelenburg gait, which occurs due to hip weakness. A stiff or rigid gait, on the other hand, is often associated with conditions affecting the joints or muscles.
Goals of Gait Training Programs
Gait training programs aim to restore normal gait patterns, minimize pain, improve balance, and increase functional mobility. The primary goals are to enable individuals to safely and independently perform essential daily activities, improve their quality of life, and reduce the risk of future falls. A successful program often involves a combination of therapeutic exercises, assistive devices, and patient education.
Historical Evolution of Gait Training Techniques
Early gait training methods focused primarily on passive exercises and assistive devices. Over time, a greater understanding of biomechanics and neuromuscular control has led to more sophisticated and targeted approaches. Modern techniques incorporate principles of functional movement, strength training, and balance exercises to achieve better and more durable results. The use of technology, such as gait analysis, has further refined the accuracy and effectiveness of gait training interventions.
Gait Abnormalities and Treatment Strategies
| Type of Gait Abnormality | Common Causes | Typical Treatment Strategies |
|---|---|---|
| Steppage Gait | Neuromuscular disorders like Charcot-Marie-Tooth disease, peripheral nerve damage, or muscular dystrophy. | Strengthening exercises for the lower extremities, proprioceptive training, and potentially orthotics. |
| Foot Drop | Peripheral nerve damage, stroke, cerebral palsy, or muscular weakness in the anterior tibialis muscle. | Strengthening exercises for the anterior tibialis muscle, use of ankle-foot orthoses (AFOs), and gait retraining exercises. |
| Trendelenburg Gait | Hip abductor weakness, often due to injury or conditions like arthritis. | Strengthening exercises for hip abductors, use of assistive devices like canes or walkers, and gait retraining. |
| Stiff or Rigid Gait | Conditions affecting the joints, such as arthritis, or neurological disorders that affect muscle control. | Range-of-motion exercises, stretching, strengthening exercises for affected muscles, and gait retraining. |
Assessment and Evaluation for Gait Training
Assessing gait is crucial for developing effective physical therapy interventions. A thorough understanding of a patient’s gait patterns, strengths, and weaknesses allows therapists to tailor treatment plans for optimal outcomes. This process involves a combination of subjective observations, objective measurements, and the use of advanced technologies. Accurate gait analysis informs treatment strategies and monitors progress throughout the rehabilitation journey.
Methods Used to Assess Gait
Gait assessment employs various methods, ranging from simple observations to sophisticated analyses. Direct observation of the patient’s walking pattern provides valuable initial insights into their gait characteristics, including stride length, cadence, and the presence of any observable compensations. These observations form the basis for more detailed assessments. Qualitative analysis involves careful scrutiny of the patient’s movement, identifying patterns and deviations from normal gait.
This method allows therapists to pinpoint potential areas for intervention.
Tools and Technologies in Gait Analysis
Advanced technologies enhance the accuracy and depth of gait analysis. Force plates measure ground reaction forces during gait, providing quantitative data on forces exerted at different phases of the gait cycle. Video recording, often combined with specialized software, allows for detailed analysis of motion, frame-by-frame, offering insights into joint angles, muscle activation, and movement coordination. 3D gait analysis systems, using multiple cameras, provide comprehensive three-dimensional data, revealing subtle deviations and asymmetries that might be missed with simpler techniques.
These systems enable a precise understanding of the biomechanics involved in gait.
Gait training in physical therapy helps patients regain their ability to walk normally after injury or illness. It’s crucial for improving mobility and independence. Understanding the intricate movements involved, like how the body coordinates and balances, is key to effective gait training. Often, this involves working with a physical therapist to practice different walking patterns. For example, learning to control the muscles involved in walking, like the ones that support the eye and regulate pupil function, is important for improved balance and stability.
To understand the anatomy of the eye, you might find this helpful: what is a pupil. Ultimately, the goal of gait training is to get patients back on their feet and moving freely again.
Factors Contributing to Gait Impairments
Numerous factors can contribute to gait impairments. Musculoskeletal conditions, such as osteoarthritis, rheumatoid arthritis, and spinal stenosis, frequently lead to pain and reduced mobility, impacting gait patterns. Neurological disorders, including stroke, multiple sclerosis, and cerebral palsy, can disrupt motor control and coordination, resulting in gait abnormalities. Other factors, such as peripheral neuropathy, can lead to sensory deficits that contribute to gait instability.
Gait training in physical therapy is crucial for restoring or improving walking ability. A key aspect of this process involves identifying and addressing any underlying issues, which often requires a skilled provider, like a physical therapist, to assess and create a personalized plan. Understanding what a provider is and their role in healthcare is vital for patients seeking this kind of therapy what is a provider.
Ultimately, gait training empowers individuals to regain their mobility and independence.
Understanding these contributing factors is essential for developing effective treatment strategies.
Importance of Patient History and Subjective Data
Patient history and subjective data play a vital role in the gait assessment process. Information about the patient’s medical history, current symptoms, pain levels, and previous treatments helps in formulating a comprehensive understanding of their condition. Patient reports regarding the onset, duration, and characteristics of gait difficulties are crucial for developing an appropriate treatment plan. Subjective feedback about comfort and perceived functional limitations is also essential.
This information, combined with objective assessments, creates a holistic picture of the patient’s needs.
Phases of Gait Analysis
Gait analysis typically follows a structured process, divided into distinct phases. The initial phase involves gathering patient history and performing a physical examination to identify any obvious musculoskeletal or neurological abnormalities. The next phase involves video recording or motion capture to document the gait pattern. Subsequent phases include data analysis using specialized software to identify specific gait deviations.
Finally, the data is interpreted to identify contributing factors and formulate treatment strategies.
Example of a Standardized Gait Assessment Protocol
A standardized gait assessment protocol might include the following steps:
- Gathering patient history and performing a physical examination, including assessment of muscle strength, range of motion, and sensation.
- Video recording of the patient walking at their self-selected pace over a specific distance, ensuring a clear view of the entire gait cycle.
- Using gait analysis software to measure parameters like stride length, cadence, step time, and velocity.
- Identifying any deviations from normal gait, such as asymmetry, excessive pronation, or antalgic gait.
- Analyzing the results to formulate a treatment plan tailored to the patient’s specific needs.
Assessment Tools for Gait Analysis
A variety of tools are employed in gait analysis. Their application depends on the specific assessment goals.
| Assessment Tool | Description | Application in Gait Analysis |
|---|---|---|
| Force Plates | Measure ground reaction forces during gait. | Quantifies forces at different gait phases, identifies asymmetries, and assesses stability. |
| Video Recording | Captures visual data of the gait cycle. | Allows for detailed analysis of joint motion, muscle activation, and compensatory mechanisms. |
| 3D Gait Analysis Systems | Utilizes multiple cameras to capture three-dimensional gait data. | Provides comprehensive analysis of spatial and temporal gait parameters, revealing subtle deviations and asymmetries. |
| Gait Analysis Software | Processes and analyzes data from various assessment tools. | Calculates gait parameters, generates reports, and facilitates comparison with normative data. |
Interventions and Techniques in Gait Training
Gait training interventions are crucial for restoring and improving functional mobility in individuals with gait abnormalities. These interventions are tailored to address the specific impairments and limitations affecting each patient’s gait cycle. A comprehensive approach often involves a combination of therapeutic exercises, assistive devices, and neuromuscular techniques. Successful outcomes depend on a thorough assessment, individualized treatment plans, and patient compliance.
Types of Interventions for Gait Abnormalities
Various interventions target different aspects of gait dysfunction. These interventions may include strengthening exercises, stretching, balance training, and gait retraining exercises. They are tailored to the specific cause and nature of the gait impairment, such as weakness, spasticity, or pain. The goal is to improve muscle strength, flexibility, and coordination to facilitate efficient and safe movement.
Techniques Used in Restoring Normal Gait Patterns
Restoring normal gait patterns involves a range of techniques. These include: addressing muscle imbalances through targeted strengthening, improving joint mobility through stretching, enhancing proprioception and balance through specific exercises, and correcting gait deviations through biofeedback and visual cues. These techniques work together to re-establish the natural rhythm and efficiency of walking.
Comparison of Therapeutic Exercise Techniques for Gait
Different therapeutic exercise techniques for gait restoration offer various approaches. For instance, resistance training can strengthen muscles involved in propulsion and support, while flexibility exercises improve joint range of motion and reduce stiffness. Balance training, utilizing unstable surfaces, enhances postural control and proprioception, which are crucial for smooth gait. Specific gait retraining exercises, such as practicing heel-toe walking, can improve the coordination and timing of movements in the gait cycle.
Role of Assistive Devices and Adaptive Equipment in Gait Training
Assistive devices and adaptive equipment play a vital role in gait training, particularly for individuals with significant mobility limitations. Walkers, canes, crutches, and prosthetics can provide support and stability, allowing patients to participate in gait training activities safely and effectively. Adaptive footwear can improve foot support and reduce pain, enhancing the overall gait experience. These tools enable patients to gradually progress towards independent mobility.
Description of Different Therapeutic Exercise Protocols
Therapeutic exercise protocols for gait training are developed based on the patient’s specific needs and goals. Protocols might involve progressive resistance training for strengthening, balance exercises on unstable surfaces, and functional gait training using various surfaces and terrains. These protocols can be adjusted based on the patient’s progress and tolerance. For example, a protocol for a patient with knee osteoarthritis might focus on strengthening quadriceps and hamstring muscles, improving joint mobility, and performing balance exercises.
Application of Neuromuscular Electrical Stimulation in Gait Training
Neuromuscular electrical stimulation (NMES) can be a valuable tool in gait training. NMES can facilitate muscle contractions, improve muscle strength and endurance, and potentially reduce pain and spasms. It can be particularly beneficial for patients with muscle weakness or neurological impairments. The specific application of NMES would be determined based on the patient’s specific needs and the assessment results.
For example, NMES might be used to stimulate the quadriceps muscles in a patient with knee weakness, leading to improved strength and gait.
Therapeutic Exercise Protocol Table
| Intervention Type | Description | Target Populations | Expected Outcomes |
|---|---|---|---|
| Resistance Training | Strengthening exercises using weights, resistance bands, or machines | Individuals with muscle weakness, impaired balance, or reduced gait speed | Improved muscle strength, increased power, and enhanced functional mobility |
| Flexibility Exercises | Stretching exercises to improve joint range of motion and reduce stiffness | Individuals with limited joint mobility, contractures, or muscle tightness | Increased flexibility, reduced pain, and improved range of motion |
| Balance Training | Exercises performed on unstable surfaces or with eyes closed to improve balance and proprioception | Individuals with impaired balance, poor coordination, or history of falls | Enhanced balance, improved coordination, and reduced risk of falls |
| Gait Retraining Exercises | Specific exercises focusing on improving gait patterns and biomechanics | Individuals with gait abnormalities, such as deviations or compensations | Improved gait efficiency, reduced gait deviations, and enhanced functional mobility |
| Assistive Device Use | Using canes, walkers, crutches, or prosthetics to support ambulation | Individuals with limited mobility or strength | Increased stability, improved balance, and enhanced mobility |
Patient Selection and Program Design
Gait training programs are highly individualized, requiring careful consideration of the patient’s specific needs and limitations. Proper patient selection and program design are crucial for achieving optimal outcomes and preventing setbacks. This section delves into the key factors involved in choosing suitable candidates for gait training and creating effective, tailored programs.Effective gait training hinges on understanding the patient’s unique condition and capabilities.
This understanding informs the creation of a personalized plan that maximizes progress while minimizing risks.
Factors to Consider When Selecting Patients
Patient selection for gait training involves a multifaceted assessment. The decision to include a patient in a gait training program hinges on several key factors. These factors include the patient’s medical history, the nature and severity of their gait impairments, their motivation and willingness to participate, and their overall physical capacity. A comprehensive evaluation is essential to determine the suitability of a patient for gait training.
- Medical History: Past diagnoses and treatments, particularly those impacting mobility or neurological function, are essential considerations. Conditions like stroke, spinal cord injury, or osteoarthritis require different approaches.
- Gait Impairments: The severity and nature of the gait dysfunction, such as weakness, pain, balance issues, or sensory deficits, directly influence the design and progression of the program. Assessing the specific areas where the patient is experiencing difficulties is crucial.
- Motivation and Willingness: Patient motivation and commitment to the program are critical for successful outcomes. Enthusiasm and a positive attitude contribute significantly to adherence and progress.
- Physical Capacity: The patient’s overall physical condition, including strength, endurance, and flexibility, plays a significant role in determining the appropriate level of intervention and intensity. Consideration should be given to the patient’s ability to tolerate the demands of the training.
Individualized Program Design, Gait training in physical therapy
Designing an effective gait training program requires a personalized approach. A customized program addresses the patient’s specific needs, capabilities, and goals. The program should be tailored to the individual, considering their strengths and weaknesses.
- Initial Assessment: The initial assessment provides a baseline understanding of the patient’s gait characteristics, functional limitations, and overall physical status. This comprehensive evaluation forms the foundation for developing the personalized program.
- Goal Setting: Collaboratively establishing realistic and measurable goals with the patient is crucial. These goals should be specific, measurable, achievable, relevant, and time-bound (SMART goals). This involves understanding the patient’s desired outcomes, such as improved walking distance or reduced pain.
- Program Components: The program should include a combination of exercises targeting strength, balance, proprioception, and cardiovascular endurance, tailored to the patient’s specific needs. This might include exercises like strengthening exercises for lower limbs, balance training using wobble boards or balance cushions, and proprioceptive neuromuscular facilitation (PNF) techniques. The exercises should be progressively challenging.
Program Progressions
Progressive overload is a key principle in gait training programs. This involves gradually increasing the intensity, duration, or complexity of the exercises to challenge the patient and promote adaptation.
- Gradual Progression: The program should progress gradually, building upon the patient’s abilities. This prevents frustration and potential injury.
- Examples: A typical progression might start with short, stationary exercises focusing on specific muscle groups. Later, the exercises could involve walking on flat surfaces, gradually increasing the distance and speed. Finally, the program could incorporate challenging terrain or inclines.
Patient Motivation and Adherence
Motivation plays a pivotal role in patient adherence to the gait training program. A positive attitude and understanding of the benefits contribute significantly to the success of the treatment.
- Encouragement: Providing positive reinforcement and encouragement throughout the training process is essential.
- Clear Communication: Open communication with the patient regarding their progress, setbacks, and future goals is crucial.
- Realistic Expectations: Setting realistic expectations helps maintain motivation and avoid frustration. Acknowledging the time commitment required and the gradual nature of improvement is vital.
Patient Education in Gait Training
Patient education is an integral component of gait training. Understanding the rationale behind the exercises and the importance of adherence enhances the effectiveness of the treatment.
- Instruction: Thorough explanation of the exercises, their purpose, and the rationale behind their use.
- Self-Management: Equipping the patient with the knowledge and skills to continue the exercises at home is vital.
- Addressing Concerns: Addressing any concerns or questions that the patient may have helps foster trust and confidence.
Program Examples
| Patient Characteristics | Program Components | Expected Progress | Considerations |
|---|---|---|---|
| Patient with stroke, moderate weakness in lower extremities, good motivation | Strengthening exercises for lower limbs, balance training on wobble board, gait training on flat surfaces, increasing distance gradually | Improved gait symmetry, increased walking speed and distance, improved balance | Close monitoring for muscle fatigue, encourage rest periods as needed |
| Patient with osteoarthritis, mild pain, moderate mobility | Range of motion exercises, strengthening exercises for core and lower limbs, low-impact aerobic exercise, pain management techniques, assistive devices as needed | Reduced pain, improved range of motion, increased mobility, improved gait efficiency | Regular pain assessment, modification of exercises based on pain levels, patient education on proper body mechanics |
Common Gait Disorders and Treatments
Gait disorders are a diverse range of conditions that affect how we walk. These disorders can significantly impact a person’s mobility, independence, and overall quality of life. Physical therapists play a crucial role in evaluating, diagnosing, and treating these conditions, working closely with patients to restore optimal gait function. Understanding the different types of gait disorders, their underlying causes, and effective treatment approaches is essential for effective physical therapy intervention.
Common Gait Disorders
Gait disorders encompass a broad spectrum of conditions, each with unique characteristics and contributing factors. Identifying these specific issues is paramount to creating targeted and effective treatment plans. Recognizing the patterns of abnormal movement is crucial for diagnosis and subsequent treatment.
- Cerebral Palsy: This group of disorders affects movement and muscle tone due to brain abnormalities during development. Common gait abnormalities include spasticity, ataxia, and weakness. These impairments can cause difficulty with balance, coordination, and walking. The severity varies greatly, impacting the intensity and nature of treatment approaches.
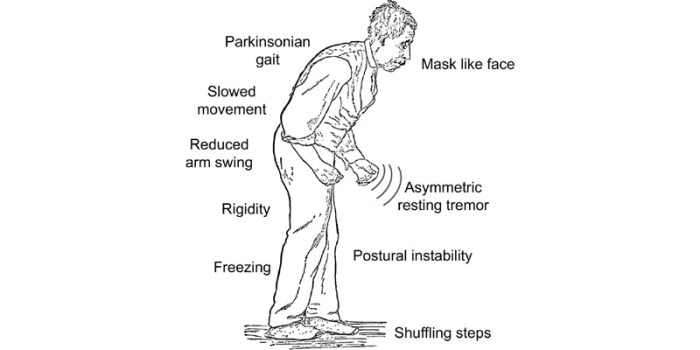
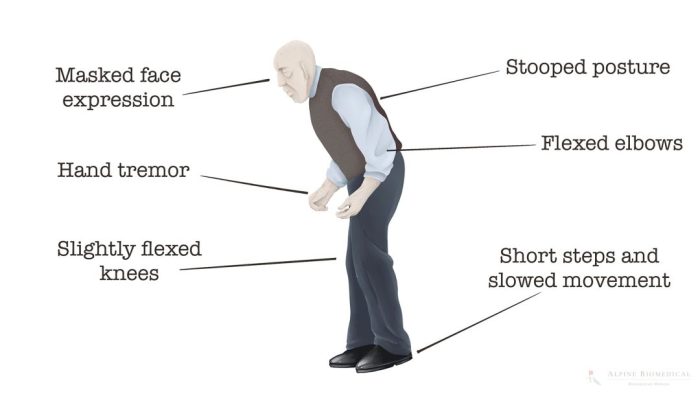
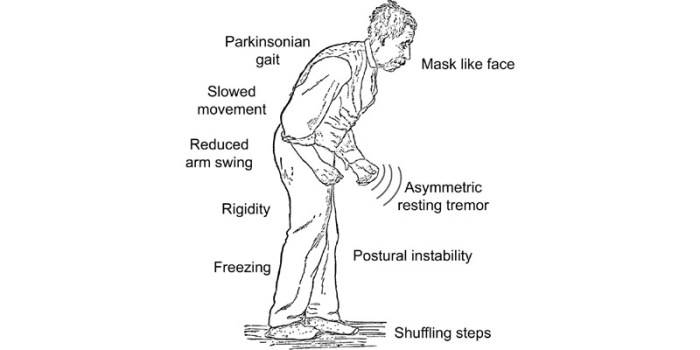
- Parkinson’s Disease: Characterized by progressive neurodegenerative changes, Parkinson’s disease often manifests as a shuffling gait with reduced arm swing, freezing episodes during gait, and postural instability. The progressive nature of the disease necessitates ongoing adjustments to treatment plans, ensuring interventions remain effective as symptoms evolve.
- Stroke: Following a stroke, patients often experience weakness, spasticity, or ataxia on one side of the body. These impairments can significantly affect gait, causing problems with balance, coordination, and step length. The specific gait deviations following a stroke depend heavily on the location and extent of the brain damage.
- Osteoarthritis: This degenerative joint disease affects the hips and knees, causing pain, stiffness, and reduced range of motion. Pain and stiffness can manifest in various ways during walking, impacting gait patterns and potentially causing limping or altered stride length. The degree of gait disturbance correlates with the severity of the arthritis.
- Multiple Sclerosis: This neurological disease involves damage to the myelin sheath surrounding nerve fibers. This damage leads to a wide array of symptoms, including gait abnormalities. These include issues with balance, coordination, and muscle weakness. The unpredictable nature of MS necessitates a dynamic and individualized approach to gait training.
Causes and Contributing Factors
The underlying causes of gait disorders are diverse and complex. Understanding these factors is essential to develop effective treatment strategies.
- Neurological Conditions: Neurological conditions like cerebral palsy, stroke, and multiple sclerosis can disrupt the signals between the brain and muscles, leading to abnormal gait patterns.
- Musculoskeletal Conditions: Osteoarthritis, hip dysplasia, and other musculoskeletal problems can cause pain, stiffness, and reduced range of motion, leading to altered gait patterns.
- Neuromuscular Diseases: Conditions such as muscular dystrophy and Charcot-Marie-Tooth disease affect muscle function and strength, directly impacting gait.
- Environmental Factors: Conditions like uneven surfaces or poor footwear can exacerbate existing gait problems.
Treatment Approaches
Treatment for gait disorders is multifaceted and often involves a combination of approaches.
- Physical Therapy: A core component of treatment, physical therapy focuses on improving strength, flexibility, balance, and coordination. Specific exercises and techniques are tailored to the individual’s needs and the specific gait disorder.
- Medications: Medications can play a supportive role in managing pain, spasticity, or other symptoms associated with specific disorders. The use of medications must be integrated within the overall treatment plan and carefully monitored by a medical professional.
- Assistive Devices: Canes, walkers, and braces can provide support and stability during gait, particularly for individuals with weakened muscles or balance issues.
- Surgery: In some cases, surgical interventions may be necessary to address underlying structural problems contributing to gait abnormalities.
Examples of Specific Exercises
Exercises tailored to the specific gait disorder are essential to enhance mobility and reduce pain.
- Cerebral Palsy: Stretching exercises, strengthening exercises, and balance exercises are crucial. Specific exercises target affected muscle groups, improving strength and flexibility. Activities like obstacle courses can help improve balance and coordination.
- Parkinson’s Disease: Exercises focusing on gait initiation, freezing episodes, and maintaining posture are crucial. Examples include heel-toe walking, stepping over objects, and practicing turning movements.
- Stroke: Exercises to improve strength, range of motion, and balance are critical. Examples include strengthening exercises for affected limbs and balance exercises like standing on one leg.
Role of Medications
Medications can be a crucial component of a comprehensive treatment plan.
- Pain Management: Analgesics or anti-inflammatory medications may be prescribed to manage pain associated with musculoskeletal conditions or neurologic disorders. These medications should be used in conjunction with physical therapy.
- Muscle Relaxants: These medications may be used to reduce spasticity in individuals with conditions like cerebral palsy or stroke.
- Other Medications: Medications for specific neurological conditions, such as those for Parkinson’s disease, are essential to manage the progression of the disease and reduce associated symptoms. These medications must be used under strict medical supervision.
Table of Common Gait Disorders
| Gait Disorder | Symptoms | Causes | Treatment Options |
|---|---|---|---|
| Cerebral Palsy | Spasticity, ataxia, weakness, difficulty with balance and coordination | Brain abnormalities during development | Physical therapy, medications, assistive devices, surgery |
| Parkinson’s Disease | Shuffling gait, reduced arm swing, freezing episodes, postural instability | Progressive neurodegenerative changes | Physical therapy, medications, assistive devices |
| Stroke | Weakness, spasticity, ataxia on one side of the body, balance and coordination problems | Cerebrovascular accident | Physical therapy, medications, assistive devices, potential surgery |
| Osteoarthritis | Pain, stiffness, reduced range of motion, limping, altered stride length | Degenerative joint disease | Physical therapy, medications, assistive devices, potential surgery |
| Multiple Sclerosis | Balance problems, coordination issues, muscle weakness, fatigue | Neurological disease | Physical therapy, medications, assistive devices, ongoing management |
Gait Training in Specific Populations
Gait training isn’t a one-size-fits-all approach. Understanding the unique needs and challenges of different patient populations is crucial for successful rehabilitation. Tailoring interventions to the specific characteristics of each group ensures optimal outcomes and fosters patient engagement. This section delves into gait training strategies for various populations, highlighting important considerations for each.
Gait Training for Pediatric Populations
Pediatric gait training focuses on developing appropriate movement patterns and promoting normal musculoskeletal development. Early intervention is key to address potential gait deviations and ensure proper motor skill acquisition. Therapists need to consider the child’s developmental stage, cognitive abilities, and emotional factors when designing the training program. Games, play-based activities, and adaptive equipment can enhance engagement and motivation.
- Emphasis on play-based activities and fun, engaging exercises to make the training more enjoyable and motivating for children.
- Careful consideration of the child’s developmental stage to adapt the exercises and intensity accordingly. Activities should be age-appropriate.
- Using assistive devices and adaptive equipment, such as walkers or braces, to support the child during gait training, when necessary.
- Incorporating family education and support to ensure a consistent and comprehensive approach to the child’s rehabilitation.
Gait Training for Geriatric Patients
Geriatric gait training addresses the specific needs of older adults, often facing challenges like decreased strength, balance issues, and decreased joint mobility. Interventions should prioritize safety, minimizing the risk of falls, and promoting independence. This approach often emphasizes functional mobility and adapting activities to the individual’s abilities.
- Prioritizing safety and fall prevention through exercises focusing on balance and proprioception.
- Utilizing assistive devices, such as walkers or canes, to enhance stability and support during gait training.
- Tailoring exercises to the patient’s specific physical limitations, adapting intensity and duration as needed.
- Incorporating functional tasks, such as navigating stairs or getting in and out of chairs, into the training program to improve real-world mobility.
Gait Training for Individuals with Neurological Conditions
Individuals with neurological conditions, such as stroke or cerebral palsy, often experience gait impairments due to motor control and coordination issues. Gait training programs should be tailored to address specific neurological deficits, promoting functional independence and improving mobility.
- Addressing specific impairments like spasticity, weakness, or sensory deficits.
- Utilizing techniques like constraint-induced movement therapy or task-oriented training to improve motor learning and functional gait.
- Using visual cues, proprioceptive feedback, and other sensory strategies to enhance gait control.
- Incorporating neuro-rehabilitation principles and therapies like constraint-induced movement therapy, which involves restricting use of the unaffected limb to promote use of the impaired limb.
Gait Training for Individuals with Musculoskeletal Impairments
Musculoskeletal impairments, such as osteoarthritis or amputations, can significantly impact gait. Gait training programs should focus on improving joint function, strength, and flexibility. Adaptive equipment, pain management strategies, and patient education are vital components of these programs.
- Addressing specific musculoskeletal impairments, such as joint pain, muscle weakness, or limited range of motion.
- Incorporating pain management techniques and strategies to address pain during movement and improve comfort.
- Using assistive devices, such as orthotics or prosthetics, to improve gait mechanics and reduce stress on affected joints.
- Focus on strengthening exercises for affected muscle groups to improve stability and support during ambulation.
Comparison of Gait Training Programs for Different Populations
| Population | Key Considerations | Training Focus | Example Interventions |
|---|---|---|---|
| Pediatric | Developmental stage, motivation, play-based activities | Normal gait development, motor skill acquisition | Play-based activities, adaptive equipment, family involvement |
| Geriatric | Balance, strength, fall prevention, functional mobility | Safe and independent mobility, functional tasks | Balance exercises, assistive devices, functional training |
| Neurological | Specific neurological deficits, motor control, coordination | Improving motor control, functional mobility, gait patterns | Constraint-induced movement therapy, sensory strategies, task-oriented training |
| Musculoskeletal | Joint pain, strength, flexibility, adaptive equipment | Improving joint function, mobility, pain management | Orthotics, prosthetics, strengthening exercises, pain management strategies |
Measuring Outcomes and Progress in Gait Training: Gait Training In Physical Therapy
Tracking progress in gait training is crucial for ensuring effectiveness and tailoring interventions. Accurate measurement allows therapists to assess the impact of treatment, adjust strategies as needed, and ultimately help patients achieve optimal functional outcomes. Monitoring patient responses and evaluating the effectiveness of interventions is key to successful rehabilitation.Precise measurement methods and standardized outcome measures provide a reliable and objective way to quantify changes in gait.
This allows for a clear understanding of the patient’s progress and facilitates communication between healthcare professionals. Furthermore, objective data supports the development of individualized treatment plans.
Methods for Measuring Gait Effectiveness
Various methods are employed to assess the effectiveness of gait training interventions. These include observational assessments, gait analysis using specialized equipment, and functional tests. Observational assessments, though subjective, provide a valuable initial evaluation. They involve the therapist observing the patient’s gait pattern, identifying areas for improvement, and tracking changes over time. Gait analysis, using sophisticated instruments like force plates and motion capture systems, provides detailed quantitative data on gait parameters.
This data allows for a more comprehensive understanding of the patient’s gait and the impact of interventions. Functional tests, such as timed up and go (TUG) or timed 25-foot walk tests, evaluate the patient’s functional mobility and ability to perform activities of daily living.
Metrics for Evaluating Gait Progress
Gait training progress is measured using a variety of metrics. These include measures of gait speed, cadence, stride length, step length, and symmetry. Changes in these metrics reflect the impact of the interventions. For instance, increased gait speed and reduced variability in gait patterns indicate improvement in the patient’s gait. Assessment of balance and postural control are also vital.
Improved balance and reduced sway are clear indicators of successful training.
Examples of Tracking and Documenting Gait Changes
Tracking changes in gait requires careful documentation. This involves recording initial gait parameters and subsequently documenting improvements over time. Using a standardized gait assessment form, clinicians can systematically note changes in gait speed, cadence, stride length, and symmetry. Progress notes should include detailed descriptions of observed changes and specific examples of improvements.
Outcome Measures in Physical Therapy
Numerous outcome measures are employed in physical therapy to assess progress. Examples include the Berg Balance Scale, the Timed Up and Go test, the Functional Gait Assessment, and the 6-minute walk test. Each measure targets specific aspects of functional mobility, balance, and gait. These standardized tools provide objective data, aiding in the assessment of progress and facilitating comparison across different patients and treatments.
Monitoring Patient Response to Interventions
Monitoring patient response involves a systematic evaluation of the patient’s progress. Regular assessments, including both objective measurements and subjective feedback from the patient, are crucial. Regular review of the patient’s progress allows for adjustments to the intervention plan, ensuring it remains tailored to the individual needs of the patient. Therapists should note any limitations or challenges faced by the patient during the intervention and make necessary modifications.
Importance of Standardized Outcome Measures
Standardized outcome measures are essential for reliable and valid assessments. They ensure consistency in measurement across different settings and therapists. This allows for comparison of results, facilitates research, and improves the overall quality of care. Standardized measures provide objective data, minimizing subjective bias and enhancing the accuracy of treatment evaluation.
Table of Outcome Measures
| Outcome Measure | Description | Application in Gait Training | Expected Improvements |
|---|---|---|---|
| Berg Balance Scale | Assesses balance and mobility | Evaluates balance before and after gait training | Improved balance, reduced falls, increased confidence in performing daily activities |
| Timed Up and Go (TUG) | Measures functional mobility | Assesses the patient’s ability to get up from a chair and walk a short distance | Decreased time to complete the task, improved gait speed, and enhanced functional mobility |
| Functional Gait Assessment (FGA) | Assesses gait quality and stability | Evaluates gait patterns, including initiation, terminal swing, and other aspects of gait | Improved gait efficiency, increased stride length, and better postural control |
| 6-Minute Walk Test | Measures the patient’s walking endurance | Assesses the patient’s ability to walk for a sustained period | Increased walking distance, improved endurance, and increased functional capacity |
Closing Notes
In conclusion, gait training in physical therapy is a multifaceted process demanding careful assessment, personalized interventions, and continuous monitoring of progress. This guide provides a detailed overview of the entire journey, empowering therapists with the knowledge to effectively address gait abnormalities and improve patients’ quality of life. The diverse techniques, from therapeutic exercises to assistive devices, highlight the multifaceted nature of this critical field.