Dystonia vs dyskinesia in parkinsons is a crucial distinction for understanding and managing this complex neurological condition. These movement disorders, often presenting with involuntary muscle contractions and abnormal movements, can significantly impact a Parkinson’s patient’s quality of life. This exploration delves into the specifics of each, their differences, and how they manifest in Parkinson’s disease. We’ll examine their underlying causes, diagnostic methods, and treatment approaches, ultimately offering a clearer understanding of these challenging symptoms.
This comprehensive guide aims to equip readers with a deeper understanding of the nuances between dystonia and dyskinesia in Parkinson’s. We will cover the various types of each, their prevalence, diagnostic criteria, and typical presentations. Moreover, we’ll delve into potential risk factors, treatment strategies, and long-term management, ultimately providing a well-rounded perspective on these often-overlooked aspects of Parkinson’s disease.
Defining Dystonia and Dyskinesia
Understanding the differences between dystonia and dyskinesia is crucial for accurate diagnosis and effective management in neurological conditions like Parkinson’s disease. Both conditions involve involuntary movements, but their underlying mechanisms and clinical presentations differ significantly. This section delves into the specifics of each, highlighting their characteristics, symptoms, and the mechanisms driving them.
Defining Dystonia
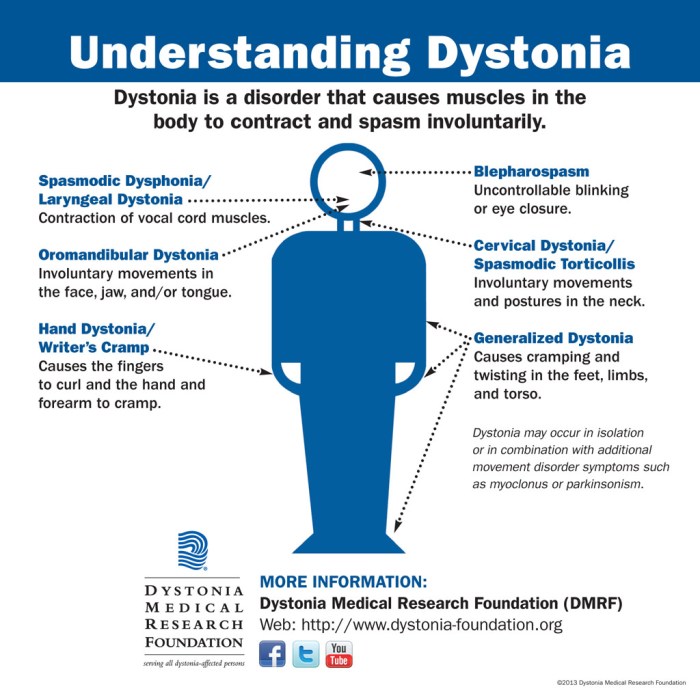
Dystonia is a neurological movement disorder characterized by sustained or intermittent muscle contractions. These contractions cause twisting, repetitive movements or abnormal postures. Symptoms can vary significantly in severity and location, affecting different parts of the body. For example, someone might experience twisting of the neck, abnormal postures of the hands or feet, or even widespread muscle contractions across multiple areas.
The spasms often cause pain and discomfort, and can significantly impact daily activities. The movements can be slow, sustained, or rapid, depending on the individual and the specific type of dystonia.
Defining Dyskinesia
Dyskinesia encompasses a group of neurological movement disorders characterized by involuntary, irregular, and often repetitive movements. These movements can range from subtle fidgeting to severe, uncontrollable jerking. The movements are typically non-rhythmic and can affect various parts of the body, including the face, arms, legs, and trunk. Dyskinesia is often associated with certain medical conditions, like Parkinson’s disease, and can be triggered or worsened by medications or other factors.
For instance, individuals with Parkinson’s disease may experience dyskinesia as a side effect of levodopa treatment.
Comparing Clinical Presentations
Dystonia and dyskinesia, while both involving involuntary movements, differ in their presentation. Dystonia often manifests as sustained, patterned movements that produce abnormal postures. Dyskinesia, on the other hand, typically presents as irregular, unpredictable movements, sometimes described as writhing or jerking. The timing and location of these movements in dyskinesia are often variable and can fluctuate over time.
The speed and pattern of dyskinetic movements can change rapidly. Distinguishing between the two conditions often relies on careful observation of the patient’s movements, noting their consistency and pattern.
Underlying Mechanisms, Dystonia vs dyskinesia in parkinsons
The precise mechanisms underlying dystonia and dyskinesia are still being investigated. However, current research suggests that dystonia may arise from abnormal neuronal activity in the basal ganglia, leading to sustained muscle contractions. This imbalance can be triggered by various factors, including genetic predisposition, environmental toxins, or brain injury. Dyskinesia, in contrast, may be linked to abnormal dopamine signaling in the brain, particularly in the basal ganglia.
Understanding the difference between dystonia and dyskinesia in Parkinson’s can be tricky, but it’s crucial for effective management. While exploring ways to manage these symptoms, it’s important to remember that sometimes lifestyle changes, like focusing on losing weight with IBS , can significantly impact overall well-being and potentially ease certain symptoms. This can, in turn, influence the progression and severity of dystonia and dyskinesia in Parkinson’s.
This can be a consequence of prolonged or excessive dopamine receptor stimulation, as seen with certain medications used to treat Parkinson’s disease.
Differences Summarized
| Feature | Dystonia | Dyskinesia |
|---|---|---|
| Movement Pattern | Sustained, twisting, repetitive, often producing abnormal postures | Irregular, unpredictable, often repetitive, jerking or writhing |
| Muscle Involvement | Localized or widespread muscle contractions | Variable, can affect various body parts |
| Symptoms | Sustained muscle contractions, abnormal postures, pain | Involuntary, irregular movements, varying in severity |
| Underlying Mechanism | Abnormal neuronal activity in the basal ganglia | Abnormal dopamine signaling in the basal ganglia |
Dystonia in Parkinson’s Disease
Dystonia, a movement disorder characterized by sustained muscle contractions, can significantly impact the quality of life for individuals with Parkinson’s disease (PD). While tremor and rigidity are more commonly associated with PD, dystonia can co-occur, often adding a complex layer to the clinical presentation and management. Understanding the nuances of dystonia in PD is crucial for accurate diagnosis and effective treatment strategies.Parkinson’s disease itself is a progressive neurodegenerative disorder, primarily affecting dopamine-producing neurons in the brain.
This dopamine deficiency leads to motor symptoms such as tremors, slowness of movement (bradykinesia), and rigidity. Dystonia, in this context, represents an additional motor complication, often manifesting as twisting or repetitive movements.
Types of Dystonia in Parkinson’s
Dystonia in Parkinson’s disease can manifest in various forms. Common types include focal dystonia, affecting a specific muscle group, and segmental dystonia, involving adjacent muscle groups. Generalized dystonia, which affects multiple muscle groups, and cranial dystonia, impacting the muscles of the head and neck, can also occur. The specific type of dystonia in a given patient can vary and may evolve over time.
Prevalence and Incidence of Dystonia in Parkinson’s
The prevalence of dystonia in Parkinson’s disease is estimated to range from 10% to 40% across different studies. The incidence, meaning the rate at which new cases occur, varies depending on the specific subtype and the patient population studied. Factors like disease duration and age of onset can influence the likelihood of developing dystonia. It is important to note that these figures represent estimates and can differ based on study methodology and inclusion criteria.
Diagnostic Criteria for Dystonia in Parkinson’s
Diagnosing dystonia in Parkinson’s involves a multi-faceted approach. Clinicians consider the patient’s medical history, physical examination findings, and potentially supporting diagnostic tests. The diagnostic criteria emphasize the presence of sustained muscle contractions, twisting movements, or postures, and their impact on daily functioning. Differentiating dystonia from other movement disorders in PD is crucial for appropriate management.
Typical Presentation of Dystonia in Parkinson’s Patients
The presentation of dystonia in Parkinson’s patients can vary. It often presents as twisting or repetitive movements, such as twisting of the neck, or abnormal postures, like a fixed position of the arm or leg. These symptoms can fluctuate in severity and may be exacerbated by factors like stress, fatigue, or changes in medication dosage. The symptoms may also be more prominent during specific times of the day.
Methods Used to Diagnose Dystonia in Parkinson’s
Various methods are used to diagnose dystonia in Parkinson’s disease, including a comprehensive neurological examination, which assesses muscle tone, reflexes, and range of motion. Electrodiagnostic studies, like electromyography (EMG), can help differentiate dystonia from other movement disorders by evaluating the electrical activity in muscles. Brain imaging techniques, such as MRI or CT scans, can assist in ruling out other potential causes of movement disorders.
Ever wondered about the difference between dystonia and dyskinesia in Parkinson’s? It’s a tricky one, but essentially, dystonia involves sustained muscle contractions, while dyskinesia is more about involuntary movements. Trying to figure out the best ways to manage these symptoms can be tough, and it’s important to talk to your doctor. This can often involve careful monitoring and adjustments to treatment plans, just like understanding how long you can safely stay in a sauna can involve knowing your body’s limits.
How long can you stay in a sauna depends on various factors, and similarly, managing Parkinson’s symptoms requires a personalized approach. Ultimately, the goal is to find what works best for you and your individual needs, and the key to this is thorough consultation with your healthcare professional.
Risk Factors for Dystonia in Parkinson’s
| Risk Factor | Description |
|---|---|
| Age of Onset | Earlier age of Parkinson’s onset may increase the risk of developing dystonia. |
| Disease Duration | Longer duration of Parkinson’s disease is often associated with a higher chance of developing dystonia. |
| Medication Dosage | Specific medications for Parkinson’s disease, especially levodopa, can potentially trigger or worsen dystonia in some individuals. |
| Genetic Predisposition | A family history of dystonia or other neurological disorders might increase the risk of developing dystonia in Parkinson’s patients. |
| Underlying Medical Conditions | Presence of other medical conditions can interact with Parkinson’s and potentially increase the likelihood of dystonia. |
Dyskinesia in Parkinson’s Disease
Parkinson’s disease, a progressive neurodegenerative disorder, often presents with motor symptoms like tremors and rigidity. However, a significant proportion of individuals with Parkinson’s also experience dyskinesias, involuntary movements that can significantly impact their quality of life. Understanding the different types, prevalence, and diagnostic criteria of dyskinesia is crucial for effective management and support.
Types of Dyskinesia in Parkinson’s
Dyskinesias in Parkinson’s can manifest in various forms, impacting different parts of the body and varying in severity. Common types include:
- Chorea: Characterized by rapid, jerky, and unpredictable movements, often involving multiple parts of the body simultaneously. These movements can be subtle or quite prominent.
- Athetosis: Involves slow, writhing, and involuntary movements, primarily affecting the extremities and face. The movements tend to be more continuous than chorea.
- Dystonia: Involves sustained muscle contractions, resulting in twisting or repetitive movements. These movements can lead to abnormal postures and impair function.
- Myoclonus: Brief, shock-like muscle contractions, often affecting the limbs. These movements are typically less severe than chorea or athetosis.
Prevalence and Incidence of Dyskinesia
The prevalence of dyskinesia in Parkinson’s disease is significant, impacting a substantial portion of patients over the long term. Studies indicate that the risk of developing dyskinesia increases with the duration of levodopa therapy, a common medication used to manage Parkinson’s symptoms. The precise incidence varies depending on factors such as age at diagnosis, the specific type of dyskinesia, and the individual’s response to treatment.
It’s important to note that not all Parkinson’s patients develop dyskinesia, and the severity can differ widely.
Diagnostic Criteria for Dyskinesia
A diagnosis of dyskinesia in Parkinson’s relies on a combination of clinical evaluation and observation. Clinicians assess the nature, frequency, and distribution of involuntary movements. A detailed medical history, including the duration and type of Parkinson’s symptoms and medication history, is crucial. No single test definitively diagnoses dyskinesia; instead, the diagnosis is based on a thorough evaluation of symptoms.
The observation of abnormal involuntary movements is central to diagnosis.
Typical Presentation of Dyskinesia in Parkinson’s
The presentation of dyskinesia in Parkinson’s patients varies greatly. Symptoms often emerge after long-term levodopa therapy, becoming more pronounced as the disease progresses. Patients may experience dyskinesia during periods of activity or rest. Some individuals experience dyskinesia that is intermittent, while others have continuous, fluctuating movements. Symptoms are typically assessed using standardized scales, which evaluate the severity and impact of the involuntary movements.
Methods Used to Diagnose Dyskinesia
Diagnosis involves a comprehensive clinical assessment. A neurological examination, focused on observing involuntary movements, is essential. Neuroimaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT), can sometimes help rule out other neurological conditions. Moreover, detailed documentation of the movements, including frequency, location, and intensity, is crucial. Specific scales are used to quantitatively assess the severity and impact of dyskinesia on daily activities.
Potential Risk Factors for Dyskinesia
Factors influencing the development of dyskinesia are complex and not fully understood. Here’s a table summarizing potential risk factors:
| Risk Factor | Description |
|---|---|
| Levodopa Dose and Duration | Higher doses and longer durations of levodopa therapy are strongly associated with a greater risk of dyskinesia. |
| Age at Parkinson’s Onset | Younger age at diagnosis might be a factor, although more research is needed to confirm this. |
| Disease Duration | The progression of the disease itself, measured in time, may play a role in the development of dyskinesia. |
| Genetic Predisposition | Some genetic variations may increase the susceptibility to dyskinesia. |
| Other Medications | Concurrent use of other medications, particularly those that interact with levodopa, can influence dyskinesia risk. |
Distinguishing Dystonia from Dyskinesia in Parkinson’s
Differentiating between dystonia and dyskinesia in Parkinson’s disease can be challenging, as both can manifest with involuntary movements. Accurate diagnosis is crucial for appropriate management and treatment. These conditions, though often co-occurring, have distinct characteristics that can be identified with careful neurological examination and, sometimes, imaging studies. Understanding these differences is vital for optimizing patient care.While both dystonia and dyskinesia involve involuntary movements, their underlying mechanisms and clinical presentation differ significantly.
Dystonia is characterized by sustained muscle contractions, often leading to twisting or repetitive movements, while dyskinesia involves involuntary, irregular movements. These differences are key in establishing a precise diagnosis.
Key Differences in Clinical Presentation
Dystonia and dyskinesia differ in the nature of the involuntary movements they produce. Dystonia typically involves sustained muscle contractions, resulting in postures or twisting movements that are often asymmetrical and can be painful. Dyskinesia, on the other hand, presents as irregular, unpredictable, and often more rapid movements. These movements can be choreiform (dance-like), athetoid (slow, writhing), or ballism (violent, jerky).
Recognizing these patterns helps distinguish between the two conditions.
Neurological Examination
A comprehensive neurological examination plays a crucial role in differentiating dystonia from dyskinesia. A thorough assessment involves observing the patient’s posture, range of motion, and involuntary movements. The examiner should carefully evaluate the distribution of the involuntary movements, their speed, and the presence of any associated features such as pain or discomfort. For example, a patient with dystonia may exhibit a characteristic posture, while a patient with dyskinesia may have more generalized, irregular movements.
Imaging Studies
Imaging studies, such as Magnetic Resonance Imaging (MRI), may provide additional insights. While MRI typically doesn’t offer definitive diagnoses, it can help rule out other neurological conditions that might mimic dystonia or dyskinesia. MRI may be helpful in cases where the clinical presentation is ambiguous, particularly to identify structural brain abnormalities that could contribute to the symptoms.
Treatment Strategies
Treatment approaches for dystonia and dyskinesia in Parkinson’s disease often differ. For dystonia, strategies might include medication adjustments, botulinum toxin injections, or surgical interventions like deep brain stimulation (DBS). Dyskinesia management often involves medication adjustments, such as lowering the dose of levodopa, or exploring other medication strategies. Individualized treatment plans are essential, as the effectiveness of various therapies can vary greatly among patients.
Figuring out dystonia versus dyskinesia in Parkinson’s can be tricky, but it’s important for proper treatment. While those are neurological issues, sometimes foot pain can be a red herring. For instance, Morton’s neuroma, a common cause of foot pain, mortons neuroma common cause of foot pain , can mimic the symptoms of movement disorders. Ultimately, accurate diagnosis of dystonia and dyskinesia is crucial for effective management of Parkinson’s symptoms.
Progression Over Time
The progression of dystonia and dyskinesia in Parkinson’s disease can vary considerably. Dystonia may initially manifest as intermittent spasms that gradually become more frequent and sustained. Dyskinesia, often associated with long-term levodopa therapy, typically appears later in the disease course, potentially increasing in severity over time. Monitoring the progression of these conditions is crucial for tailoring treatment strategies and managing potential complications.
Treatment Approaches
Managing dystonia and dyskinesia in Parkinson’s disease requires a multifaceted approach tailored to the individual patient. The effectiveness of interventions varies greatly, highlighting the need for personalized strategies. Treatment aims to alleviate symptoms, improve quality of life, and minimize the impact of these debilitating motor fluctuations.Addressing these motor complications often involves a combination of pharmacological and non-pharmacological strategies.
Finding the optimal balance and adjusting treatments over time is crucial for managing these conditions effectively.
Treatment Strategies for Dystonia in Parkinson’s Disease
Various treatment strategies are employed to manage dystonia in Parkinson’s disease. These approaches aim to reduce the severity and frequency of dystonic spasms.
- Pharmacological Interventions: Adjustments to Parkinson’s medications, such as increasing levodopa dosage or adding dopamine agonists, are frequently attempted. Sometimes, increasing the dose of medications that are known to help with dystonia can provide relief. However, these adjustments can also increase the risk of dyskinesia.
- Botulinum Toxin (Botox): Injections of botulinum toxin are a common treatment option. These injections can temporarily relax muscles affected by dystonia, reducing spasms and improving movement. However, the effects are temporary, requiring repeated injections. Side effects from Botox include pain at the injection site and bruising.
- Surgical Interventions: Deep brain stimulation (DBS) is a surgical option that may be considered in cases of severe, medication-resistant dystonia. DBS involves implanting electrodes in specific brain regions to deliver electrical impulses, modulating abnormal neuronal activity. The effectiveness of DBS in managing dystonia in Parkinson’s disease can vary considerably.
- Physical Therapy and Occupational Therapy: These non-pharmacological therapies can significantly improve functional ability and reduce the impact of dystonia. Strategies like stretching, range-of-motion exercises, and assistive devices can enhance daily activities and reduce discomfort. Occupational therapy can adapt daily routines to accommodate dystonic movements and improve independence.
Treatment Strategies for Dyskinesia in Parkinson’s Disease
Managing dyskinesia in Parkinson’s disease focuses on reducing the severity and frequency of involuntary movements.
- Pharmacological Adjustments: Reducing levodopa dosage or adjusting the timing of medication administration can sometimes reduce dyskinesia. Adding medications such as amantadine or adjusting the dose of other medications may also be considered. This approach aims to strike a balance between managing Parkinson’s symptoms and minimizing dyskinesia. However, reducing levodopa can worsen Parkinson’s symptoms.
- Lowering Levodopa Dose: Reducing the dosage of levodopa, the primary medication for Parkinson’s disease, is a common strategy to manage dyskinesia. This reduction aims to decrease the intensity of dopamine fluctuations, thereby reducing the frequency and severity of dyskinesia. However, this reduction often leads to worsening of Parkinson’s motor symptoms.
- Combination Therapy: Combining different medications, including those that affect dopamine receptors or other neurotransmitters, may provide better symptom control and minimize dyskinesia. This approach often involves careful monitoring and adjustments to dosage and timing.
- Surgical Interventions: Deep brain stimulation (DBS) can also be considered in cases of severe, medication-resistant dyskinesia. As with dystonia, the effectiveness of DBS in managing dyskinesia can vary significantly.
Comparison of Treatment Effectiveness
The effectiveness of treatments for dystonia and dyskinesia in Parkinson’s varies depending on individual factors and the specific characteristics of each condition.
| Treatment | Side Effects |
|---|---|
| Levodopa Dose Adjustments | Parkinson’s symptom worsening, dyskinesia fluctuations |
| Botulinum Toxin (Botox) | Pain at injection site, bruising |
| Deep Brain Stimulation (DBS) | Surgical risks, infection, device malfunction |
| Amantadine | Confusion, dizziness, hallucinations, nausea, sleep disturbances |
Examples of Medication
Examples of medications used to manage dystonia include botulinum toxin (Botox), and adjustments in the dosage of Parkinson’s medications.Examples of medications used to manage dyskinesia include amantadine, and adjustments in the dosage of Parkinson’s medications.
Illustrative Case Studies
Understanding dystonia and dyskinesia in Parkinson’s disease requires looking at real-life examples. These case studies, while hypothetical, illustrate the diverse ways these movement disorders can manifest and affect individuals. They highlight the challenges in diagnosis and the importance of personalized treatment approaches.The following case studies detail the symptoms, diagnosis, and treatment for patients with dystonia and dyskinesia, respectively, in the context of Parkinson’s disease.
They emphasize the physical and emotional toll these conditions can take on patients and their families.
Case Study 1: Dystonia in Parkinson’s Disease
This case involves a 62-year-old male patient, Mr. A, diagnosed with Parkinson’s disease five years prior. He initially presented with the typical Parkinsonian symptoms, including tremors, rigidity, and bradykinesia. However, over time, he started experiencing progressively worsening dystonic spasms in his left foot. These spasms were particularly pronounced during periods of stress or fatigue.
The spasms made walking difficult and painful, and his gait became unsteady.Mr. A’s symptoms were initially attributed to worsening Parkinson’s disease. However, a detailed neurological examination, including specific tests for dystonia, revealed the separate nature of the spasms. A diagnosis of dystonia co-occurring with Parkinson’s disease was made.Treatment involved a combination of strategies. Medication adjustments, including levodopa optimization, were attempted.
Physical therapy focused on improving flexibility and range of motion, along with exercises to address the specific muscle groups affected by dystonia. Botulinum toxin injections into the affected muscles provided temporary relief from the spasms. Support groups and counseling helped Mr. A cope with the emotional and psychological impact of the disease.Long-term outcomes for patients with Parkinson’s-related dystonia can vary significantly.
While some individuals experience periods of remission or significant improvement, others may experience persistent symptoms that impact their quality of life. Mr. A, in this example, continued to experience fluctuating dystonic episodes despite treatment.
Case Study 2: Dyskinesia in Parkinson’s Disease
A 58-year-old female patient, Ms. B, experienced dyskinesia as a complication of long-term levodopa therapy for her Parkinson’s disease. Her initial symptoms, including tremors and rigidity, were effectively managed with medication. However, after several years of stable control, Ms. B developed increasingly frequent and severe dyskinetic movements, particularly in her arms and legs.
These movements were involuntary, jerky, and unpredictable, making everyday tasks challenging.Ms. B’s symptoms were further assessed by a specialist to differentiate the dyskinesia from other movement disorders. A detailed medical history, including medication records and a neurological examination, confirmed the diagnosis of levodopa-induced dyskinesia.Treatment strategies focused on managing the dyskinesia while maintaining adequate Parkinson’s disease symptom control. This included adjusting the timing and dosage of levodopa, as well as exploring alternative medications that might minimize dyskinetic movements.
Deep brain stimulation (DBS) was also considered, but its application depended on the severity and responsiveness to other treatments. The emotional impact of the dyskinesia on Ms. B’s daily life was addressed through counseling and support groups.Long-term outcomes for patients with levodopa-induced dyskinesia are variable. While some patients may experience partial or complete remission with medication adjustments, others may continue to experience significant challenges with their dyskinetic movements.
Ms. B, in this example, saw some improvement in the frequency and severity of her dyskinesia with medication adjustments, but the symptoms persisted.
Prognosis and Long-Term Management: Dystonia Vs Dyskinesia In Parkinsons
Living with Parkinson’s disease (PD) can be challenging, and the presence of dystonia or dyskinesia adds another layer of complexity. Understanding the long-term outlook and developing effective management strategies is crucial for maintaining a good quality of life for individuals affected by these conditions. This section delves into the prognosis and management approaches for both dystonia and dyskinesia in the context of Parkinson’s.The long-term management of dystonia and dyskinesia in Parkinson’s involves a multifaceted approach encompassing medication adjustments, lifestyle modifications, and supportive therapies.
The goal is to mitigate symptoms, improve functional abilities, and enhance the overall well-being of the patient.
Long-Term Prognosis for Dystonia in Parkinson’s
Dystonia in Parkinson’s is often a progressive condition. While the progression varies greatly from person to person, it typically involves a gradual worsening of symptoms over time. The severity of the dystonia, its location, and the overall progression of Parkinson’s disease are all contributing factors. Some individuals may experience periods of stability, while others may see a more rapid decline.
The long-term prognosis is highly dependent on the individual’s specific response to treatment and the underlying progression of Parkinson’s disease.
Long-Term Prognosis for Dyskinesia in Parkinson’s
Dyskinesia, a common side effect of levodopa therapy in Parkinson’s, is often characterized by involuntary movements. The severity and type of dyskinesia can fluctuate significantly. Some individuals may experience mild, intermittent dyskinesia, while others may face more severe and debilitating movements. The long-term prognosis is influenced by the duration and dose of levodopa therapy, as well as the individual’s response to treatment adjustments.
The progression of Parkinson’s itself also plays a role in the evolution of dyskinesia.
Strategies for Long-Term Management of Dystonia and Dyskinesia
Effective long-term management of dystonia and dyskinesia requires a personalized approach tailored to the individual’s needs. Medication adjustments are often a cornerstone of treatment. This might involve altering the dosage, timing, or type of medication to minimize symptoms while maintaining adequate Parkinson’s control. Furthermore, non-pharmacological strategies are also important, including physical therapy, occupational therapy, and speech therapy.
These therapies can help improve motor skills, functional abilities, and communication, mitigating the impact of dystonia and dyskinesia. In addition, lifestyle modifications such as exercise, a balanced diet, and stress management techniques are important components of a comprehensive approach.
Importance of Patient Education and Support
Patient education plays a critical role in managing dystonia and dyskinesia. Educating patients about their condition, potential triggers, and treatment options empowers them to actively participate in their care. This knowledge empowers patients to make informed decisions and adapt their lifestyle to manage symptoms more effectively. Support groups and counseling services can provide valuable emotional and practical support, helping patients cope with the emotional toll of these conditions.
Understanding the emotional impact and providing support mechanisms can significantly improve the patient’s overall quality of life.
Potential Impact on Quality of Life
Dystonia and dyskinesia can significantly impact a patient’s quality of life. The involuntary movements, pain, and limitations in daily activities can lead to feelings of frustration, isolation, and reduced independence. The impact varies greatly from individual to individual, depending on the severity and type of symptoms. Strategies to address these impacts, including therapy, social support, and adjustments in daily routines, can enhance the quality of life.
Summary
In conclusion, differentiating dystonia from dyskinesia in Parkinson’s requires a nuanced understanding of their distinct characteristics and presentations. While both can significantly impact a patient’s life, their underlying mechanisms, symptoms, and treatment strategies differ. This in-depth look at dystonia vs dyskinesia in parkinsons aims to provide a clearer picture for patients, caregivers, and healthcare professionals. By understanding these complexities, we can better support those living with Parkinson’s disease.