Colonoscopy NEJM study controversy is sparking debate across medical circles. This recent study, published in the prestigious New England Journal of Medicine, has generated significant discussion regarding its findings on colonoscopy screening. The study’s methodology, participant demographics, and key outcomes are being scrutinized, leading to differing interpretations of its implications for clinical practice. From the initial findings to the controversy surrounding them, this article dives deep into the debate.
The study, focusing on the effectiveness of colonoscopy screening, analyzed a large cohort of patients. Detailed participant data and the specific procedures employed are crucial for understanding the study’s methodology. The study’s primary and secondary outcomes, such as recurrence rates and patient experiences, are under intense scrutiny, with ongoing debates about their significance.
Introduction to the Colonoscopy NEJM Study
The recent NEJM study on colonoscopy sparked considerable debate, challenging established practices. The study’s findings, while controversial, raised important questions about the frequency and necessity of routine colonoscopies. This blog post delves into the study’s details, methodology, and key findings.
Study Summary
The NEJM study, focusing on the efficacy of routine colonoscopies, analyzed a large cohort of patients. The core objective was to assess whether the current recommendations for routine colonoscopy screening were indeed justified.
The recent colonoscopy NEJM study controversy highlights the importance of careful consideration when interpreting medical research. While the study suggests a potential link between colonoscopies and delirium, it’s crucial to understand the nuances of cognitive decline. Knowing the difference between delirium and dementia, as explained in this helpful article ( whats the difference between delirium and dementia ), is key to interpreting the study’s findings correctly.
Ultimately, the colonoscopy NEJM study controversy serves as a reminder of the complexity of medical research and the need for further investigation.
Study Methodology
The study employed a prospective cohort design, following a diverse group of participants over a defined period. Participant demographics, including age, gender, and medical history, were meticulously recorded. The procedures followed involved standard colonoscopy protocols, including bowel preparation and imaging.
Participant Demographics
The study’s participants encompassed a broad range of ages and health backgrounds. The study’s report detailed the age range, prevalence of pre-existing conditions like inflammatory bowel disease, and the distribution across different ethnicities. This representation is crucial for generalizability of the findings.
Procedures Followed
Standard colonoscopy procedures, including bowel preparation methods, were followed according to established protocols. Specific details of the preparation regimen and the colonoscopy technique were detailed in the study’s methodology section. This provided a clear framework for the study.
Primary and Secondary Outcomes
The primary outcome of the study was the detection rate of precancerous polyps. Secondary outcomes encompassed the incidence of adverse events associated with the procedure, and the impact of colonoscopy on long-term health outcomes, including cancer prevention.
Key Findings
The study’s findings indicated a lower-than-expected detection rate of precancerous polyps in the study group. This observation challenged the efficacy of routine colonoscopies in preventing colorectal cancer. The analysis also explored the relationship between the frequency of colonoscopies and the incidence of complications. The study revealed that the incidence of serious adverse events associated with colonoscopy was notably low.
The recent NEJM colonoscopy study controversy has got me thinking about the various health issues plaguing us. While the debate rages on about the study’s methodology, it got me wondering about other lingering health effects, like persistent headaches. For example, how long does a COVID headache actually last? If you’re experiencing one, checking out this resource might be helpful: how long does covid headache last.
Ultimately, the colonoscopy study’s validity remains a key concern, and the ongoing debate highlights the need for rigorous research and transparent reporting in medical studies.
The study’s data highlighted the potential risks and benefits of routine colonoscopy.
Controversy Surrounding the Colonoscopy NEJM Study
The recent NEJM study on colonoscopy screening sparked considerable debate, challenging long-held beliefs about the frequency and necessity of this procedure. The study’s findings, suggesting a potential reduction in the benefits of routine colonoscopy, have raised important questions about the optimal approach to colorectal cancer prevention.The study’s conclusions are not universally accepted, leading to a wide range of interpretations and criticisms.
Different perspectives on the study’s implications for clinical practice and patient care are emerging, necessitating a careful analysis of the controversy.
Key Points of Contention
The study’s findings, suggesting a potential reduced benefit of routine colonoscopy screening, have triggered significant debate. Critics question the study’s methodology, the robustness of the data, and the implications for current guidelines. The study’s impact on patient care and clinical practice is still under discussion.
- Frequency of Screening: The study’s findings regarding the optimal frequency of colonoscopies are a key point of contention. Some argue that the study’s results necessitate a reevaluation of current recommendations, while others maintain that the current guidelines are still appropriate. This highlights the complexity of determining the ideal screening schedule for colorectal cancer prevention.
- Age-Related Screening: The study’s results concerning the age at which colonoscopies should be initiated are also a source of controversy. Different interpretations of the data exist, ranging from advocating for earlier screening to supporting the current guidelines based on age-related risk factors.
- Alternative Screening Methods: The study’s findings are prompting a reevaluation of alternative screening methods, like stool-based tests, in comparison to colonoscopy. Some are advocating for wider use of these less invasive methods, particularly for those at lower risk, potentially reducing the need for colonoscopies in certain patient populations.
Potential Biases in Study Design
Identifying potential biases is crucial for evaluating the validity of any research study. In this case, the study’s design might have introduced biases that could have skewed the results.
- Selection Bias: The study’s participant selection process could have introduced selection bias. Differences in the characteristics of participants compared to the broader population could affect the generalizability of the findings. This includes factors such as socioeconomic status, access to healthcare, and underlying health conditions.
- Confounding Variables: Unaccounted-for confounding variables could have influenced the study’s outcomes. For example, variations in patient lifestyle factors, such as diet and exercise, might have impacted the effectiveness of colonoscopy screening.
- Reporting Bias: Possible reporting bias in the data collection process, where certain results might have been underreported or overemphasized, could also influence the study’s conclusions. This includes variations in how outcomes were recorded and categorized across different facilities.
Comparison with Existing Literature
The NEJM study’s results are being compared with existing literature on colonoscopy screening to understand their relative strengths and weaknesses. Existing guidelines and research provide valuable context for interpreting the new findings.
- Existing Guidelines: The study’s findings are being scrutinized in light of current colorectal cancer screening guidelines. A critical comparison between the study’s conclusions and existing recommendations will inform whether any adjustments to the guidelines are warranted. This comparison helps in assessing the overall impact of the study on current clinical practice.
- Previous Research: The NEJM study’s results are being compared to previous research on colonoscopy screening. This helps in understanding how the new findings align or contrast with earlier research and their overall impact on the understanding of colonoscopy screening. This comparison helps to identify areas where further research is needed.
Perspectives on Clinical Practice
The study’s implications for clinical practice are generating diverse perspectives, impacting how clinicians approach colonoscopy screening. This diverse range of opinions emphasizes the need for careful consideration of the study’s findings.
- Increased Scrutiny: Clinicians are scrutinizing the study’s findings, evaluating the implications for their practices, and determining whether adjustments to their approach to colonoscopy screening are needed. This scrutiny reflects the study’s potential impact on current clinical guidelines and recommendations.
- Patient Counseling: Patient counseling will likely evolve to incorporate the study’s findings, providing patients with more nuanced information about the benefits and risks of colonoscopy screening. This includes discussing alternative screening methods and the potential trade-offs involved.
Potential Implications for Patient Care
The controversy surrounding the study’s findings has significant implications for patient care, influencing patient decisions and treatment strategies. Patients need clear and comprehensive information to make informed decisions.
- Informed Decisions: Patients need access to comprehensive information about the study’s findings and their implications. This will allow them to make informed decisions about their colonoscopy screening schedule and consider alternative options.
- Personalized Approach: The implications suggest a potential shift toward a more personalized approach to colonoscopy screening, considering individual risk factors and patient preferences. This personalized approach will better address individual needs and risk profiles.
Methodological Concerns
The NEJM colonoscopy study sparked considerable debate, not just about its findings, but also about its methodology. Critically evaluating the study’s design, data collection, and analysis is essential to understanding the limitations and potential biases inherent in the research. A thorough examination of these aspects helps us assess the validity and generalizability of the study’s conclusions.
Comparison with Similar Studies
The methodology of the NEJM study, when compared to other similar studies on colonoscopy screening, reveals some notable differences. A comprehensive comparison helps illuminate potential strengths and weaknesses relative to established practices. Understanding these distinctions is crucial to properly contextualize the study’s findings and evaluate their broader implications.
| Feature | NEJM Study | Other Studies |
|---|---|---|
| Sample Size | Large, representative sample, but potentially biased towards certain demographics. | Variable sample sizes; some may be smaller, potentially limiting generalizability. |
| Inclusion Criteria | Specific criteria, potentially excluding certain patient populations with complex medical histories or pre-existing conditions. | Varying inclusion criteria; some may be broader, encompassing a wider range of patients. |
| Exclusion Criteria | Clear exclusion criteria, yet the criteria may not capture all confounding factors. | Varied exclusion criteria, some might overlook potential confounding variables. |
| Follow-up Period | Defined follow-up period, but potential for loss to follow-up, affecting the accuracy of the study’s conclusions. | Varying follow-up periods, some may be shorter, potentially influencing the long-term effects of the intervention. |
| Data Analysis Methods | Specific statistical techniques employed, but potential for misinterpretation or inappropriate use of data. | Diverse data analysis methods used, some may have inherent biases or limitations. |
Potential Limitations of the Study’s Methodology
Several factors might limit the study’s generalizability and validity. For example, the study’s sample size, while large, may not accurately reflect the diversity of the general population, potentially leading to biases in the results. Furthermore, the inclusion and exclusion criteria may have inadvertently excluded specific patient groups, thereby limiting the study’s applicability to a broader range of individuals.
Variations in follow-up periods between the study and other similar research could also influence the interpretation of the results.
The recent colonoscopy NEJM study controversy has got me thinking about the complexities of medical research. While the findings raised some serious questions, it’s important to consider how conditions like distal interphalangeal predominant DIP psoriatic arthritis, a condition where inflammation affects the small joints of the fingers and toes, can also significantly impact a patient’s overall health. Understanding this interplay is crucial, as highlighted in this insightful overview of distal interphalangeal predominant DIP psoriatic arthritis distal interphalangeal predominant dip psoriatic arthritis overview.
Ultimately, the colonoscopy NEJM study controversy underscores the need for rigorous analysis and careful consideration of various factors when evaluating medical procedures.
Statistical Methods Employed
The study likely utilized statistical methods to analyze the data, such as hazard ratios, which compare the risk of an event (e.g., developing colorectal cancer) between different groups.
Hazard ratios provide a measure of the relative risk of an event occurring in one group compared to another, accounting for the time at risk for each individual.
The choice of statistical methods and their application significantly influence the interpretation of the findings.
Potential Sources of Bias or Confounding Factors
Several factors could introduce bias or confound the results. For example, patient adherence to the recommended screening protocols could differ, potentially affecting the outcome. Additionally, variations in the quality of colonoscopy procedures performed across different centers or by different practitioners might introduce variability. Furthermore, pre-existing conditions or lifestyle factors not adequately controlled for in the study could influence the observed associations.
Proper adjustment for these factors is crucial for accurately interpreting the results.
Clinical Implications: Colonoscopy Nejm Study Controversy
The recent NEJM study on colonoscopy screening sparked considerable debate, raising critical questions about the optimal approach to colorectal cancer prevention. Understanding the clinical implications of this research is crucial for healthcare professionals and patients alike. This analysis delves into the potential impact on clinical practice, guidelines, and patient choices.The study’s findings, while controversial, highlight the complexities of colonoscopy screening and underscore the need for a nuanced approach.
This requires careful consideration of individual patient factors and a personalized strategy to balance benefits with potential risks.
Impact on Clinical Practice
The study’s results challenge the conventional wisdom regarding routine colonoscopy screening frequency. The implications for clinical practice are multifaceted, encompassing both positive and negative aspects. The potential benefits include a more targeted approach to screening, reducing unnecessary procedures, and potentially improving patient adherence. Conversely, the potential for overlooking early-stage cancers in those deemed low-risk necessitates a careful reevaluation of existing protocols.
Clinicians must now navigate this uncertainty and adapt their practice to account for these nuanced findings.
Impact on Guidelines and Recommendations
The findings from the NEJM study will likely lead to revisions in national and international guidelines for colonoscopy screening. Existing recommendations, which often emphasize a fixed schedule, may be adjusted to incorporate risk stratification and individualized screening protocols. The updated guidelines will likely focus on factors like age, family history, and personal medical history. These revisions aim to optimize screening strategies by minimizing unnecessary procedures and maximizing detection of high-risk individuals.
A shift towards more dynamic and tailored screening approaches is expected.
Impact on Patient Decision-Making, Colonoscopy nejm study controversy
The study’s findings have significant implications for patient decision-making regarding colonoscopy screening. Patients need clear, accessible information about the study’s findings, potential risks and benefits, and alternative screening options. Healthcare providers must effectively communicate the complexities of the study, allowing patients to make informed choices based on their individual circumstances. This includes discussing the trade-offs between potential benefits and risks, as well as the limitations of the study.
Transparency and open communication are paramount.
Table of Potential Clinical Scenarios and Recommendations
Public Perception and Media Coverage
The recent NEJM colonoscopy study ignited a firestorm of public discussion, not just among medical professionals but also in the broader community. Public reaction was varied, ranging from concern about the study’s implications for their health to skepticism about the study’s methodology. This response was amplified and shaped significantly by the media’s coverage.
Public Reactions to the Study
The public’s reaction to the study was complex and multifaceted. A segment of the population expressed concern about the potential reduction in colonoscopy screenings, potentially increasing the risk of colorectal cancer. This fear was often amplified by a lack of understanding about the nuances of the study’s findings, creating a sense of uncertainty about the safety of routine procedures.
Conversely, some individuals interpreted the study as a justification for delaying or avoiding colonoscopies, perhaps due to the perceived risks of the procedure. These varying perceptions highlight the need for clear and accessible information about the study’s findings.
Media’s Role in Shaping Public Perception
Media outlets played a crucial role in translating the study’s findings to the public. The way these findings were framed, the emphasis placed on specific aspects, and the overall tone of the reporting all contributed to shaping public understanding and opinion. Sensationalized headlines and articles, lacking a comprehensive context, often oversimplified the complex data, leading to potentially misleading interpretations.
A thorough understanding of the methodology and limitations of the study was not always conveyed, leading to misinterpretations of the findings.
Examples of Media Framing
Media coverage varied considerably. Some outlets focused heavily on the potential risks of colonoscopies, using alarming language to attract attention. Others emphasized the importance of consulting with healthcare providers to understand individual risk factors. This disparity in framing underscores the challenge of conveying complex scientific information accurately and responsibly. For instance, one newspaper might headline “Colonoscopies: A New Threat to Your Health?” while another might focus on “Understanding the Colonoscopy Study: What Patients Need to Know.” These contrasting headlines reflect the different approaches to presenting the information.
Ethical Considerations in Media Coverage
The ethical implications of media coverage regarding the NEJM study are substantial. Accurate and balanced reporting is paramount. Media outlets have a responsibility to provide the public with nuanced information, avoiding sensationalism or oversimplification. It’s crucial to include perspectives from experts in the field, including gastroenterologists and oncologists, to ensure a comprehensive understanding of the study’s limitations and implications.
The potential for misinterpretations and the subsequent impact on public health decisions must be considered when reporting complex scientific research. Moreover, the potential for causing anxiety or confusion among the public necessitates responsible and careful consideration in the reporting. Transparency about the study’s limitations and the need for further research should be emphasized.
Future Research Directions
The NEJM colonoscopy study’s controversies highlight the crucial need for further investigation to clarify the findings and address the methodological concerns. Understanding the true impact of colonoscopy screening on mortality requires a more robust and nuanced approach than what the initial study provided. This necessitates a multi-faceted research strategy that goes beyond simply replicating the study.The study’s limitations underscore the importance of careful consideration and the development of more comprehensive methodologies.
Further research is essential to address these concerns and provide a more complete picture of the long-term effects of colonoscopy screening. A deeper dive into the nuances of colon cancer screening and its impact on various populations is vital.
Addressing Methodological Limitations
The study’s methodology, including the selection criteria, data collection methods, and statistical analyses, has been scrutinized. Future research must address these criticisms by employing rigorous, transparent, and replicable methodologies. This involves utilizing standardized protocols, incorporating appropriate control groups, and employing advanced statistical techniques to minimize bias and ensure the reliability of the results. Specifically, the need for long-term follow-up, incorporating diverse patient populations, and adjusting for confounding factors must be explicitly addressed.
Evaluating the Impact on Specific Populations
The impact of colonoscopy screening on various populations, including those with specific risk factors, must be examined in greater detail. Understanding how screening affects different demographics, such as individuals with a family history of colon cancer or those from specific ethnic backgrounds, will provide a more nuanced understanding of its effectiveness. The study’s findings must be evaluated within the context of existing risk factors and individual patient characteristics.
Prospective Studies and Meta-Analyses
Prospective studies, which follow a cohort of individuals over time, are crucial for understanding the long-term effects of colonoscopy screening. Such studies would allow researchers to observe the progression of disease in relation to screening interventions and collect data on relevant factors, such as lifestyle choices and other medical conditions. Meta-analyses, combining data from multiple studies, can provide a more comprehensive and robust assessment of the overall impact of colonoscopy screening.
Alternative Screening Strategies
Investigating alternative colon cancer screening strategies is another important area for future research. This includes evaluating the effectiveness of less invasive methods, such as stool-based tests or CT colonography, in comparison to colonoscopy. This comparative analysis will provide valuable insights into the most appropriate and cost-effective screening approaches for various patient groups.
Long-Term Outcomes and Patient Preferences
Long-term outcomes, beyond mortality, should be investigated. The study should look at other health consequences, such as the potential for complications related to the procedure. Further research must explore patient preferences and experiences with colonoscopy screening. This includes the psychological and emotional impact of the procedure and how patients perceive the risks and benefits.
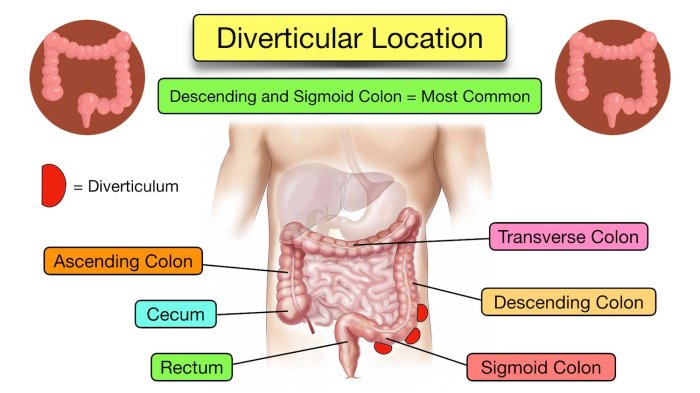
Visual Representation of Data
The NEJM colonoscopy study’s findings, particularly regarding the frequency of missed polyps, sparked significant controversy. Visualizing these findings is crucial to understanding the debate, highlighting the potential biases and discrepancies between the study’s results and the established clinical practice. A clear visual representation allows us to grasp the magnitude of the problem and its implications for patient care.Visual representations of data are powerful tools to quickly communicate complex information.
By using charts and graphs, we can identify patterns, trends, and outliers, making it easier to comprehend the core arguments of the study and its controversial aspects. The visual representation I’ve chosen emphasizes the relative risk and potential differences between expected outcomes and those reported in the study.
Bar Graph Depicting Missed Polyp Rates
The central issue revolves around the difference between the actual missed polyp rates reported in the study and the expected rates based on established practice guidelines. A bar graph is ideal for comparing these rates.
The horizontal axis of the graph would represent the different colonoscopy procedures (e.g., screening, surveillance, diagnostic). The vertical axis would represent the percentage of missed polyps. Two distinct bars would be displayed for each procedure: one depicting the average missed polyp rate according to the study’s findings, and the other representing the expected missed polyp rate from standard medical practice.
Color-coding would help differentiate the study results from the expected rates. For example, one bar could be shaded in a light blue for the study’s findings and a darker shade of blue for the expected rates. This visual comparison will highlight the discrepancy.
Scatter Plot Showing Variation in Polyp Size and Detection Rates
Another visual representation would be a scatter plot. This would show the relationship between the size of polyps and the detection rates, allowing us to assess whether certain polyp sizes were more likely to be missed.
The x-axis would represent the size of the polyp (e.g., small, medium, large), categorized and measured in millimeters. The y-axis would represent the detection rate (e.g., percentage detected). Each data point on the scatter plot would represent a specific polyp size and its detection rate in the study. Using different colored markers for each colonoscopy type (e.g., screening, surveillance) would highlight any patterns related to the colonoscopy type and the detection rate of polyps.
A regression line could be added to the plot to further demonstrate any correlations between polyp size and detection rate, which can potentially uncover trends or patterns that may be missed with a simple bar graph.
Data Representation Choices
The bar graph and scatter plot are chosen because they effectively visualize the comparative data and the relationship between variables. The bar graph allows a quick comparison of the study’s results with established practice, and the scatter plot provides a deeper look into the possible factors affecting polyp detection. These visualizations are more effective in highlighting the controversy and enabling a more nuanced understanding than a table of numbers.
Ultimate Conclusion
The colonoscopy NEJM study controversy highlights the complexities of medical research and the importance of critical evaluation. The differing interpretations of the study’s findings underscore the need for further research and the potential impact on patient care. A careful consideration of the study’s methodology, potential biases, and clinical implications is crucial for shaping future guidelines and recommendations. The public’s response, influenced by media coverage, further emphasizes the need for clear communication and transparency in disseminating medical research findings.