Chronic fatigue syndrome vs fibromyalgia: Understanding these conditions is crucial for those affected and those supporting them. This exploration delves into the complexities of diagnosing, treating, and living with these often-misunderstood illnesses. We’ll examine their shared and distinct symptoms, explore the challenges in diagnosis, and investigate the potential underlying mechanisms.
Both conditions significantly impact daily life, affecting work, social activities, and overall well-being. This blog post aims to provide a comprehensive overview, equipping readers with a better understanding of these challenging illnesses.
Understanding Chronic Fatigue Syndrome and Fibromyalgia
Chronic Fatigue Syndrome (CFS) and Fibromyalgia (FM) are debilitating conditions characterized by widespread pain and persistent fatigue. While often confused, they have distinct features and diagnostic criteria. This section will clarify the similarities and differences, highlighting common symptoms and the specific diagnostic approaches for each condition.These conditions significantly impact daily life, often leading to limitations in work, social activities, and overall well-being.
Understanding the nuances of each condition is crucial for effective diagnosis and management.
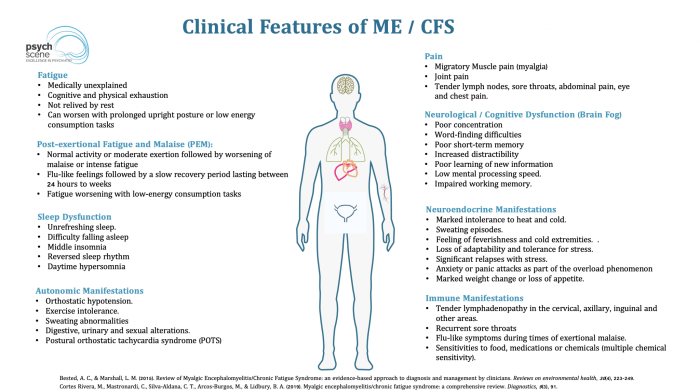
Overview of Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome, or CFS, is primarily defined by overwhelming fatigue that lasts for at least six months. This fatigue is often not relieved by rest and significantly impacts daily functioning. It’s a complex disorder with a multitude of potential contributing factors.
Overview of Fibromyalgia (FM)
Fibromyalgia (FM) is characterized by widespread musculoskeletal pain accompanied by fatigue, sleep disturbances, and cognitive difficulties. The pain is often described as aching, burning, or stabbing, and it typically affects multiple areas of the body. Unlike CFS, FM doesn’t focus solely on fatigue but incorporates a constellation of symptoms.
Similarities Between CFS and FM
Both CFS and FM share several overlapping symptoms, leading to frequent misdiagnosis. These shared symptoms include:
- Profound fatigue: This is a hallmark of both conditions, impacting energy levels and the ability to engage in daily activities.
- Sleep disturbances: Difficulty falling asleep, staying asleep, or experiencing restorative sleep is common to both CFS and FM.
- Cognitive difficulties: “Brain fog” or difficulties with concentration, memory, and other cognitive functions are often reported by individuals with either condition.
Differences Between CFS and FM
Despite the overlapping symptoms, CFS and FM differ in their primary focus and diagnostic criteria. A crucial distinction is the nature of the pain.
- CFS: Focuses primarily on extreme fatigue, which is often the most prominent symptom. The pain, when present, tends to be less widespread and less prominent than the fatigue.
- FM: Focuses on widespread pain as a primary symptom. While fatigue is also a common feature, the persistent pain is often the driving force behind the diagnosis.
Diagnostic Criteria for CFS
The diagnostic criteria for CFS often rely on a combination of symptoms and a lack of other explanations for the fatigue.
- Symptom duration: Fatigue must persist for at least six months.
- Symptom severity: The fatigue must significantly impair daily activities and not be attributable to other medical conditions.
- Exclusion of other causes: The fatigue should not be easily explained by other conditions, like depression or anxiety.
Diagnostic Criteria for Fibromyalgia
The diagnosis of Fibromyalgia (FM) usually requires a combination of widespread pain and other associated symptoms.
- Widespread pain: Pain must be present in at least multiple body areas, often described as aching, burning, or stabbing.
- Symptoms of FM: Additional symptoms such as fatigue, sleep disturbances, and cognitive difficulties are often present and contribute to the overall diagnosis.
- Exclusion of other causes: The symptoms should not be easily explained by other medical conditions.
Diagnostic Challenges: Chronic Fatigue Syndrome Vs Fibromyalgia
Navigating the world of chronic illnesses like Chronic Fatigue Syndrome (CFS) and Fibromyalgia (FM) often feels like walking through a dense fog. One of the most significant hurdles is the lack of definitive diagnostic tools. The very nature of these conditions, characterized by a complex interplay of symptoms, makes precise identification and differentiation a challenging endeavor.The absence of objective markers for both CFS and FM often leads to a diagnostic journey filled with uncertainty and potential misdiagnosis.
Clinicians must rely heavily on the patient’s self-reported symptoms, making the subjective experience of the individual central to the diagnostic process. This reliance on symptom-based criteria necessitates a thorough understanding of the complexities of the conditions and a careful evaluation of the patient’s individual experience.
Diagnostic Criteria Reliance
The diagnostic criteria for CFS and FM are primarily symptom-based. This means that doctors assess the presence and severity of specific symptoms to arrive at a diagnosis. This method, while necessary, presents challenges due to the highly subjective nature of many of the symptoms. Patients may experience varying degrees of the same symptom, and the interpretation of these experiences can differ greatly from one individual to another.
Difficulties in Distinguishing CFS and FM
The symptoms of CFS and FM can overlap considerably, making differentiation difficult. Both conditions are characterized by fatigue, pain, and cognitive dysfunction, which can make accurate diagnosis challenging for healthcare professionals. The shared symptoms can contribute to diagnostic confusion and delay in receiving the appropriate care.
Lack of Objective Diagnostic Tests
Currently, there are no objective diagnostic tests for either CFS or FM. This lack of definitive biomarkers for these conditions creates a significant hurdle for healthcare professionals. The absence of objective tests often necessitates a comprehensive evaluation of the patient’s history, physical examination, and symptom reporting to reach a diagnosis.
Subjective Nature of Symptoms
The subjective nature of symptoms in both CFS and FM is a critical factor in the diagnostic process. Factors such as individual variations in pain perception, cognitive function, and fatigue levels can significantly influence the experience and reporting of symptoms. This subjectivity can make comparing and contrasting symptoms between individuals challenging, further complicating the diagnostic process.
Comparison of Diagnostic Criteria
| Characteristic | Chronic Fatigue Syndrome (CFS) | Fibromyalgia (FM) |
|---|---|---|
| Primary Symptom | Extreme fatigue lasting at least six months, with significant impact on daily activities. | Widespread musculoskeletal pain, often accompanied by fatigue, sleep disturbances, and cognitive dysfunction. |
| Duration of Symptoms | Persistent fatigue for at least six months. | Persistent pain for at least three months. |
| Symptoms (Key) | Post-exertional malaise, sleep disturbances, cognitive dysfunction, and headache. | Widespread pain, tenderness to the touch at specific points, and sleep disturbances. |
| Other Considerations | Exclusion of other conditions with similar symptoms. | Exclusion of other conditions with similar symptoms. |
This table highlights some key differences in the diagnostic criteria for CFS and FM. The reliance on symptom reporting and the absence of objective tests necessitate a careful and thorough assessment process for both conditions.
Symptoms and Manifestations
Understanding the wide range of symptoms associated with Chronic Fatigue Syndrome (CFS) and Fibromyalgia (FM) is crucial for accurate diagnosis and effective management. These conditions are often characterized by overlapping symptoms, making differentiation challenging. This section delves into the diverse array of physical, cognitive, and emotional manifestations, highlighting the variability between individuals.The symptoms of CFS and FM can significantly impact daily life, affecting work, relationships, and overall well-being.
Figuring out chronic fatigue syndrome versus fibromyalgia can be tricky, right? Sometimes, seemingly unrelated symptoms like ear drainage can complicate the picture. Understanding the causes and treatment options for ear drainage is crucial, as it can sometimes be a symptom of an underlying health condition, potentially linked to the complex interplay of CFS and fibromyalgia. For a deeper dive into the potential causes and treatment of ear drainage, check out this helpful resource on ear drainage causes and treatment.
Ultimately, accurately diagnosing and managing these conditions requires careful consideration of all presenting symptoms.
Recognizing these symptoms is a first step toward seeking appropriate medical attention and support.
Physical Symptoms
Physical symptoms are often prominent in both CFS and FM. A wide array of physical discomfort can be experienced, significantly impacting daily activities. Muscle pain, fatigue, and sleep disturbances are key components of both conditions.
- Fatigue: This is a hallmark symptom of both CFS and FM, characterized by extreme tiredness and lack of energy. The fatigue in CFS is often described as debilitating, hindering even basic tasks. In FM, the fatigue is frequently accompanied by pain and stiffness.
- Pain: Widespread pain is a defining feature of FM, often described as aching, throbbing, or burning sensations. CFS may also present with muscle or joint pain, though this is not as consistently a prominent feature as in FM.
- Sleep Disturbances: Difficulty falling asleep, staying asleep, or experiencing restful sleep is common to both conditions. This can further exacerbate fatigue and other symptoms.
- Other Physical Symptoms: Other potential physical symptoms include headaches, dizziness, gastrointestinal issues, and musculoskeletal problems. These symptoms can vary significantly in intensity and frequency.
Cognitive Symptoms
Cognitive impairments, often referred to as “brain fog,” are significant challenges for individuals with CFS and FM. These impairments can affect concentration, memory, and processing speed.
Figuring out chronic fatigue syndrome (CFS) versus fibromyalgia can be tricky, as their symptoms overlap. One aspect often overlooked is how physical activity, like running a mile, affects calorie expenditure. Knowing how many calories you burn running a mile how many calories do you burn running a mile might help you better understand your body’s needs when dealing with these conditions.
Ultimately, a doctor’s diagnosis is crucial for proper management of either CFS or fibromyalgia.
- Concentration Problems: Difficulty concentrating, focusing on tasks, and maintaining attention are common cognitive symptoms.
- Memory Issues: Short-term memory problems and difficulty recalling information are frequent complaints.
- Processing Speed: Slower processing speed and difficulty with mental tasks can affect daily functioning.
Emotional Symptoms
The emotional impact of CFS and FM is often underestimated. These conditions can lead to significant emotional distress, impacting mental health and overall well-being.
- Mood Swings: Fluctuations in mood, including irritability, anxiety, and depression, are common.
- Anxiety and Depression: The chronic nature of these conditions can contribute to feelings of anxiety and depression, requiring specific mental health support.
- Emotional Exhaustion: The persistent physical and cognitive symptoms can lead to significant emotional exhaustion and feelings of overwhelm.
Symptom Severity Comparison
| Symptom Category | Chronic Fatigue Syndrome (CFS) | Fibromyalgia (FM) ||—|—|—|| Physical | Severe, debilitating fatigue, widespread pain, significant sleep disturbances | Widespread pain, fatigue, varying intensity, sleep disturbances || Cognitive | Significant brain fog, difficulty with concentration and memory | Cognitive impairments, including concentration and memory problems, varying intensity || Emotional | Increased risk of anxiety and depression, emotional exhaustion | Increased risk of anxiety and depression, emotional exhaustion, mood swings |
Underlying Mechanisms
Unraveling the intricate biological pathways behind chronic fatigue syndrome (CFS) and fibromyalgia (FM) remains a significant challenge for researchers. While definitive causes remain elusive, growing evidence points towards a complex interplay of factors involving inflammation, immune dysfunction, and potential genetic predispositions. This exploration delves into the current understanding of these underlying mechanisms, highlighting similarities and differences between the two conditions.The complex nature of these conditions suggests that a single, isolated cause is unlikely.
Instead, it is probable that a combination of genetic, environmental, and lifestyle factors contribute to the development and persistence of symptoms. Understanding these contributing factors is crucial for developing effective treatment strategies and improving the lives of those affected.
Potential Biological Mechanisms
Current research suggests that both CFS and FM are likely influenced by a combination of biological factors. Inflammation, immune dysfunction, and neuroendocrine imbalances are key areas of investigation. The interplay between these factors is likely different for each individual, adding further complexity to the conditions.
Role of Inflammation
Inflammation, a crucial part of the body’s defense mechanism, is often implicated in the development and persistence of both CFS and FM. Chronic low-grade inflammation can lead to various symptoms, including fatigue, pain, and sleep disturbances. Studies have shown elevated levels of inflammatory markers, such as cytokines, in individuals with both conditions. This chronic inflammation may contribute to the persistent pain and fatigue observed in these conditions.
Immune Dysfunction
Immune dysfunction is another potential contributor to both CFS and FM. The intricate balance of the immune system may be disrupted, potentially leading to an overreaction or underreaction to various stimuli. This disruption may contribute to the development of chronic fatigue and pain, and the exacerbation of symptoms by external factors. For example, infections or other stressors may trigger or worsen symptoms in individuals with compromised immune function.
Neuroendocrine Imbalances
Neuroendocrine imbalances, which affect the intricate interplay between the nervous and endocrine systems, are also suspected to play a role. Hormonal fluctuations and dysfunction in the hypothalamic-pituitary-adrenal (HPA) axis, responsible for stress response, have been linked to the development and exacerbation of symptoms. Disruptions in the neurotransmitter systems, which regulate mood and pain perception, may also be involved.
Genetic Predisposition
Genetic factors likely contribute to an individual’s susceptibility to developing CFS and FM. While no single gene has been identified as a definitive cause, studies suggest a complex interplay of genes, potentially influencing immune response, inflammation, and pain perception. Family history of these conditions may indicate a potential genetic predisposition.
Factors Contributing to Development
Several factors are thought to contribute to the development of both CFS and FM. These include infections, physical trauma, psychological stressors, and environmental exposures. The specific factors that trigger the conditions vary greatly between individuals. For example, one person might experience a viral infection, while another might experience a traumatic event as a catalyst.
Potential Interactions Diagram
Imagine a complex web of interacting factors. At the center, genetic predisposition influences an individual’s susceptibility. External factors like infections, trauma, or stress can trigger a cascade of events. These events, including neuroendocrine imbalances, and immune dysfunction, lead to chronic inflammation. The interplay of these factors leads to the persistent symptoms of fatigue, pain, and cognitive dysfunction.
This web is highly individualized and not precisely understood.
Treatment Approaches

Navigating the complex landscapes of Chronic Fatigue Syndrome (CFS) and Fibromyalgia (FM) often feels like trying to thread a needle in a hurricane. The lack of a single, definitive diagnostic test and the highly variable presentation of symptoms make treatment a personalized journey. Finding effective strategies that address the diverse needs of each individual is crucial. This often involves a multifaceted approach that considers both the physical and psychological aspects of the illness.Effective treatment for CFS and FM involves a multifaceted approach tailored to individual needs.
A personalized plan should address symptoms, manage pain, and improve overall quality of life. This necessitates a deep understanding of the patient’s unique experience and preferences. Crucially, treatment should be ongoing and adaptable to changing symptoms.
Different Treatment Strategies
Various strategies are employed in treating CFS and FM. These include lifestyle modifications, medications, and complementary therapies. The selection of specific treatments is heavily influenced by the individual patient’s symptoms, preferences, and medical history.
Figuring out chronic fatigue syndrome vs. fibromyalgia can be tricky, right? Understanding your health insurance options is just as important, especially when dealing with conditions like these. A gold plan health insurance, like gold plan health insurance what is it , can significantly impact your ability to manage the costs of treatment and ongoing care. Ultimately, knowing your options and how they relate to your specific needs is key to navigating these complex health issues.
Lifestyle Modifications
Implementing lifestyle adjustments can significantly impact the management of CFS and FM symptoms. Regular exercise, even in small increments, can improve energy levels and mood. Prioritizing adequate sleep is paramount, as sleep disturbances are frequently reported by patients. Maintaining a balanced diet, avoiding triggers (such as caffeine or stress), and practicing stress-reducing techniques, like mindfulness or meditation, can also contribute to symptom control.
Medications
Various medications are used to manage symptoms of CFS and FM. Pain relievers, such as NSAIDs or opioids, may help with pain management. Stimulants can sometimes increase energy levels. Antidepressants can be beneficial in addressing pain, sleep disturbances, and mood symptoms. However, medication responses vary widely, and finding the right medication or combination of medications often requires trial and error.
“Medication selection should be a collaborative decision between the patient and their healthcare provider.”
Complementary Therapies
Complementary therapies, including physical therapy, occupational therapy, and counseling, play an important role in the comprehensive management of CFS and FM. Physical therapy can help improve strength, flexibility, and endurance. Occupational therapy can help patients adapt their daily routines to accommodate their limitations. Counseling can address the psychological distress often associated with these conditions.
Patient-Centered Care
Patient-centered care is paramount in managing CFS and FM. This approach prioritizes the patient’s individual needs, preferences, and values. Open communication, active listening, and shared decision-making are essential elements of patient-centered care. Understanding the patient’s perspective is vital for developing an effective treatment plan.
Multidisciplinary Teams
Multidisciplinary teams, comprised of specialists like physicians, physical therapists, occupational therapists, psychologists, and social workers, can provide comprehensive care. The collaborative nature of these teams allows for a holistic approach to treatment, addressing the various physical, psychological, and social aspects of the conditions.
Comparison of Treatment Modalities
| Treatment Modality | CFS Effectiveness | FM Effectiveness | Potential Considerations |
|---|---|---|---|
| Lifestyle Modifications | Often beneficial, improves quality of life | Often beneficial, improves quality of life | Requires commitment and patient follow-through |
| Medications | Varied responses, requires careful selection | Varied responses, requires careful selection | Potential side effects, trial and error approach |
| Complementary Therapies | May improve symptoms and function | May improve symptoms and function | Individual responses vary, not a replacement for medical care |
| Multidisciplinary Teams | Provides comprehensive care, improves outcomes | Provides comprehensive care, improves outcomes | Requires access to specialized expertise |
Impact on Daily Life
Chronic Fatigue Syndrome (CFS) and Fibromyalgia (FM) profoundly impact daily life, often making simple tasks feel overwhelming. These conditions aren’t just about feeling tired; they significantly alter how individuals function and interact with the world around them. The impact extends far beyond physical symptoms, affecting emotional well-being, social connections, and professional life.Living with CFS and FM requires constant adaptation and resourcefulness.
The fluctuating energy levels, pain, and cognitive difficulties can disrupt routines, making it hard to maintain independence and participate in activities once enjoyed. The unpredictable nature of these conditions adds a layer of stress and anxiety to daily life, further hindering overall well-being.
Impact on Work
The fluctuating energy levels, cognitive difficulties, and pain associated with CFS and FM can severely impact employment. Many individuals experience reduced productivity, missed workdays, and difficulty concentrating on tasks. These conditions can also lead to job loss or career limitations due to the ongoing challenges of maintaining a consistent work schedule and fulfilling job requirements. For example, a person with CFS or FM might find it challenging to focus on complex tasks or maintain consistent energy levels throughout the workday, impacting their ability to meet deadlines or perform at a satisfactory level.
Impact on Social Activities
Social activities can become a significant challenge for individuals with CFS and FM. The fluctuating energy levels, pain, and cognitive difficulties can make it challenging to participate in social events, maintain relationships, and engage in hobbies. The unpredictable nature of these conditions can also lead to social isolation and feelings of loneliness, as individuals may find it difficult to keep up with social commitments or maintain consistent social interactions.
This can manifest in the form of cancelled plans, missed gatherings, and reduced social contact.
Impact on Relationships
The significant impact of CFS and FM on daily life can strain relationships. Changes in energy levels, mood swings, and difficulties with communication can create tension and misunderstandings within personal relationships. The constant need for rest and accommodation can place a burden on family members and partners, potentially leading to frustration and resentment. For instance, a partner might feel frustrated with the limitations imposed by the condition, while the individual with CFS or FM might feel misunderstood or unsupported.
Impact on Daily Tasks
Managing daily tasks can be incredibly difficult for individuals with CFS and FM. Simple activities, such as showering, cooking, or cleaning, can become significant hurdles due to pain, fatigue, and cognitive impairments. These conditions can significantly impact the ability to perform basic self-care activities, leading to a decrease in overall independence and quality of life. Individuals may require assistance with daily tasks or make significant adjustments to their routines to accommodate their symptoms.
For instance, a person with CFS or FM might need to break down large tasks into smaller, more manageable steps or enlist help from others to complete daily chores.
Impact on Quality of Life
The chronic nature of CFS and FM can significantly diminish the quality of life for those affected. The constant pain, fatigue, and cognitive difficulties can limit participation in activities, hobbies, and social events. This can lead to feelings of isolation, depression, and anxiety, further impacting overall well-being. The ability to enjoy life’s simple pleasures and engage in meaningful activities is often severely compromised.
Impact on Social Life
Social interactions become challenging due to the fluctuating energy levels, pain, and cognitive difficulties. Individuals may find it difficult to maintain friendships, attend social gatherings, or participate in activities that were once enjoyable. This can lead to social isolation and feelings of loneliness. Individuals with CFS and FM might need to limit their social engagements or adjust their social interactions to accommodate their symptoms.
For example, attending a party might be exhausting and painful, making it necessary to leave early or decline invitations altogether.
Challenges in the Workplace
The unpredictable nature of CFS and FM presents significant challenges in the workplace. Fluctuating energy levels, cognitive difficulties, and pain can lead to missed workdays, reduced productivity, and difficulty concentrating on tasks. This can result in difficulties with meeting deadlines, completing projects, and maintaining consistent job performance. Employers may not fully understand the challenges faced by employees with CFS and FM, potentially leading to misunderstandings or discrimination.
This can manifest in difficulties with scheduling, workload management, and accommodations.
Research and Future Directions
The quest to understand and effectively treat chronic fatigue syndrome (CFS) and fibromyalgia (FM) hinges on ongoing research. Current knowledge, while offering insights into these complex conditions, leaves significant gaps in our understanding of their underlying causes and effective treatments. This exploration into the future of research will highlight promising avenues for progress, emphasizing the crucial role of ongoing investigations in improving the lives of those affected.
Ongoing Research Efforts
Research into CFS and FM is multifaceted, encompassing various approaches to uncover the intricate mechanisms driving these conditions. Scientists are employing a variety of methodologies, from genetic studies to neuroimaging techniques, to delve into the biological underpinnings of these illnesses. This multifaceted approach is crucial given the complex interplay of factors likely contributing to these conditions.
Areas of Active Investigation
Numerous areas are currently under intense investigation. Genetic research is uncovering potential susceptibility genes and pathways linked to the development of CFS and FM. Neuroimaging studies are providing insights into brain function and structure, potentially revealing alterations in brain regions associated with pain processing, fatigue, and cognition. Furthermore, investigations into the role of the immune system and its interactions with the nervous system are being pursued.
These efforts aim to illuminate the intricate interplay of factors contributing to the symptoms experienced by patients.
Potential Breakthroughs in Treatment and Diagnosis, Chronic fatigue syndrome vs fibromyalgia
Advancements in diagnostic tools and therapeutic strategies are crucial for improving the lives of those living with CFS and FM. Researchers are exploring novel biomarkers that could aid in early detection and diagnosis, moving beyond the reliance on subjective symptom reports. Moreover, innovative treatments targeting specific biological pathways implicated in the conditions are being investigated. For example, therapies that modulate the immune system or address neuroinflammation show promise, though further research is necessary to validate these approaches.
Importance of Research to Improve Lives
Research efforts play a pivotal role in improving the lives of individuals affected by CFS and FM. By uncovering the underlying causes and mechanisms, scientists pave the way for more precise and effective treatments. Furthermore, improved diagnostic tools can lead to earlier intervention and potentially better management of symptoms. This has profound implications for reducing the debilitating impact of these conditions on daily life.
Current Research Findings
Recent research has highlighted potential avenues for treatment and diagnosis. Studies suggest a link between gut microbiota imbalances and CFS/FM symptoms. These findings underscore the potential role of restoring gut health in managing these conditions. Further, research indicates that interventions targeting neuroinflammation, such as certain anti-inflammatory medications, may show promise in alleviating symptoms. It is important to note that these are preliminary findings, and further research is necessary to confirm their validity and translate them into effective treatments.
Potential Implications of Future Research Directions
The future of research in CFS and FM holds significant potential. Continued investigations into genetic predispositions, immune system dysregulation, and neuroinflammation could lead to the development of personalized treatment strategies tailored to individual needs. These strategies could improve symptom management and overall well-being. For example, a better understanding of the role of specific immune cells in CFS/FM could lead to the development of targeted therapies that effectively modulate the immune response, thereby reducing the intensity of symptoms.
This could lead to better outcomes and quality of life for those living with these debilitating conditions.
Final Summary
In conclusion, chronic fatigue syndrome and fibromyalgia present unique diagnostic and treatment challenges. While sharing some overlapping symptoms, crucial differences exist in their presentation and underlying mechanisms. The subjective nature of symptoms underscores the importance of patient-centered care and multidisciplinary approaches to treatment. Further research is essential to enhance diagnostic accuracy and develop more effective treatments, ultimately improving the quality of life for those affected.

