Causes of lower leg pain can range from simple overuse injuries to more complex conditions. This guide delves into the various potential culprits behind lower leg discomfort, providing a detailed overview of the anatomy, common causes, traumatic injuries, overuse syndromes, nerve-related issues, vascular problems, inflammatory conditions, and other possibilities. We’ll explore the symptoms, diagnostic considerations, and treatment approaches for each type of pain, empowering you with a better understanding of your lower leg’s health.
From the intricate interplay of bones, muscles, and tendons to the crucial role of blood flow, we’ll examine the complex factors that contribute to lower leg pain. We’ll also highlight the importance of seeking professional medical advice for accurate diagnosis and effective management of your condition.
Anatomy of the Lower Leg
The lower leg, a vital component of the human musculoskeletal system, is a complex structure responsible for mobility and stability. Understanding its intricate anatomy is crucial for comprehending the causes of pain and injuries. This section delves into the bones, muscles, tendons, and ligaments that make up the lower leg, their individual functions, and how they work together.The lower leg’s intricate design allows for a wide range of movements, from walking and running to jumping and hopping.
Understanding the precise interplay of these structures helps to diagnose and treat various lower leg ailments effectively.
Bones of the Lower Leg
The lower leg’s skeletal framework is primarily composed of the tibia and fibula. These long bones, positioned side-by-side, provide structural support and act as attachment points for muscles and tendons. The tibia, being the larger and more medial bone, bears the brunt of the body’s weight. The fibula, situated laterally, plays a supporting role and is involved in ankle stability.
Their precise alignment and connection to the ankle bones are critical for proper function.
Muscles of the Lower Leg
The lower leg is packed with powerful muscles that enable a wide range of movements. These muscles are crucial for activities such as dorsiflexion, plantar flexion, inversion, and eversion of the foot. They work in concert to propel the body forward and maintain balance. The arrangement and function of these muscles are key to understanding potential injuries.
Tendons and Ligaments of the Lower Leg
Tendons connect muscles to bones, facilitating the transmission of force generated by muscular contractions. Ligaments, on the other hand, connect bones to other bones, providing stability and preventing excessive movement. The lower leg’s complex network of tendons and ligaments is crucial for coordinated movement and protection against injuries. Damage to these structures can lead to significant pain and impairment.
Table: Lower Leg Structures
| Structure | Function | Potential Injury Sites |
|---|---|---|
| Tibia | Primary weight-bearing bone of the lower leg | Fractures, stress fractures, tibial plateau fractures |
| Fibula | Provides lateral support and attachment for muscles | Fractures, stress fractures, peroneal tendon injuries |
| Gastrocnemius | Plantar flexion of the foot (pointing toes downwards) | Muscle strains, tendinopathy (Achilles tendon) |
| Soleus | Assists in plantar flexion | Muscle strains, tendinopathy (Achilles tendon) |
| Anterior Tibialis | Dorsiflexion of the foot (lifting toes upwards) | Tendinitis, strains |
| Peroneal Muscles | Eversion and plantar flexion of the foot | Tendinitis, tears, sprains |
| Medial and Lateral Malleoli | Provide stability and attachment points for ligaments | Fractures, sprains (lateral ankle sprains) |
| Anterior Cruciate Ligament (ACL) | Provides stability to the knee joint, indirectly affecting lower leg | Tears, sprains |
| Posterior Cruciate Ligament (PCL) | Provides stability to the knee joint, indirectly affecting lower leg | Tears, sprains |
Blood Supply to the Lower Leg
The lower leg receives its blood supply from the popliteal artery, which branches into several smaller arteries. These arteries deliver oxygen and nutrients to the muscles, tendons, ligaments, and bones, ensuring proper function. Disruptions to this blood supply can lead to pain, ischemia (lack of blood flow), and potential tissue damage. Peripheral arterial disease (PAD) is an example of a condition affecting the blood vessels in the lower leg, which can cause significant pain and discomfort.
Common Causes of Lower Leg Pain
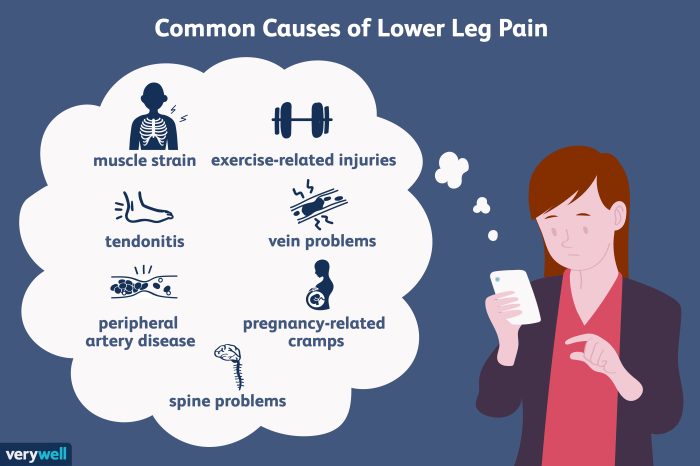
Lower leg pain can stem from a variety of issues, ranging from minor strains to more serious conditions. Understanding the potential causes is crucial for proper diagnosis and effective treatment. Pinpointing the source of the discomfort allows for targeted interventions and a faster return to normal activity.
Musculoskeletal Issues
Musculoskeletal problems are a frequent cause of lower leg pain. These issues often involve the muscles, tendons, ligaments, and bones of the lower leg. Various activities, from intense exercise to everyday movements, can strain these structures, leading to pain and discomfort.
- Muscle Strains and Sprains: These injuries are common, especially in athletes and individuals involved in physical activities. A muscle strain occurs when a muscle is stretched or torn, while a sprain involves damage to the ligaments surrounding a joint. Symptoms often include localized pain, tenderness, swelling, and limited range of motion. Examples include hamstring strains in runners or ankle sprains from sudden twists.
Proper rest, ice, compression, and elevation (RICE) are typically recommended for initial treatment.
- Tendinitis: Inflammation of a tendon, often due to overuse or repetitive stress. Pain is typically localized to the affected tendon, and it can worsen with activity. Achilles tendinitis, affecting the Achilles tendon, is a common example, often experienced by runners and those participating in jumping sports. Rest, physical therapy, and anti-inflammatory medications may be necessary.
- Fractures: A break in a bone, fractures can occur due to trauma or stress. Symptoms include sharp pain, swelling, bruising, and deformity. A stress fracture, a tiny crack in a bone, is often seen in athletes who engage in repetitive high-impact activities. A fracture resulting from a fall or accident will manifest with more severe pain and potentially an obvious change in the leg’s shape.
- Shin Splints: Pain along the shinbone, often caused by repetitive stress on the muscles and tissues around the tibia. The pain is usually mild at first, but it can intensify with activity. Shin splints are commonly seen in runners and dancers.
Vascular Issues
Vascular problems in the lower leg can lead to pain, often associated with reduced blood flow.
- Deep Vein Thrombosis (DVT): A blood clot in a deep vein, typically in the leg. Symptoms include pain, swelling, warmth, and redness in the affected area. DVT can be a serious condition requiring immediate medical attention.
- Peripheral Artery Disease (PAD): A narrowing of the arteries that supply blood to the legs. Symptoms include pain, cramping, numbness, and coldness in the legs, particularly during exercise. The pain often subsides with rest.
Neurological Issues
Conditions affecting the nerves in the lower leg can cause pain.
- Nerve Compression: Pressure on a nerve, often due to a herniated disc or other structural abnormalities. Symptoms may include pain, numbness, tingling, and weakness in the affected area. Symptoms are often dependent on the specific nerve involved.
Infections
Infections can sometimes cause lower leg pain.
- Cellulitis: A bacterial infection of the skin and underlying tissues. Symptoms include redness, swelling, warmth, pain, and fever. Prompt medical attention is necessary to prevent complications.
Summary Table
| Cause | Typical Symptoms | Potential Diagnostic Tests |
|---|---|---|
| Muscle Strains/Sprains | Localized pain, tenderness, swelling, limited range of motion | Physical examination, imaging (X-ray, MRI) |
| Tendinitis | Localized pain, tenderness, pain worsening with activity | Physical examination, imaging (ultrasound) |
| Fractures | Sharp pain, swelling, bruising, deformity | Physical examination, imaging (X-ray, MRI) |
| Shin Splints | Pain along the shinbone, worsening with activity | Physical examination, imaging (X-ray, MRI) |
| DVT | Pain, swelling, warmth, redness in affected area | Physical examination, Doppler ultrasound |
| PAD | Pain, cramping, numbness, coldness in legs, particularly during exercise | Physical examination, ankle-brachial index (ABI) |
| Nerve Compression | Pain, numbness, tingling, weakness in affected area | Physical examination, nerve conduction studies |
| Cellulitis | Redness, swelling, warmth, pain, fever | Physical examination, blood tests, imaging (ultrasound) |
Traumatic Injuries
Lower leg pain can stem from various traumatic events, ranging from minor sprains to severe fractures. Understanding the mechanisms of these injuries is crucial for accurate diagnosis and effective treatment. Prompt medical attention is essential to minimize complications and ensure a proper recovery.Trauma to the lower leg can result in a spectrum of injuries, impacting everything from soft tissues to the hard bone structure.
The severity of the injury is often determined by the force and direction of the impact, as well as the specific anatomical structures involved. Recognizing the patterns of injury can help healthcare professionals pinpoint the affected area and develop a suitable treatment plan.
Common Types of Traumatic Injuries
Several common traumatic injuries affect the lower leg, each with distinct characteristics and treatment approaches. These injuries can be broadly categorized into fractures, sprains, and strains, each with its own mechanism of injury and resulting symptoms.
Fractures
Fractures involve a break in the bone. These breaks can range from hairline cracks to complete breaks, depending on the force of the impact. Common causes include falls, direct blows, and high-impact sports activities. A fall from a significant height or a direct blow to the lower leg, such as a football tackle, can result in a fracture.
The mechanism of injury often determines the location and type of fracture. For instance, a fall directly onto the tibia might result in a tibial shaft fracture. Diagnosis often involves X-rays and other imaging techniques to confirm the break’s location and severity.
Sprains
Sprains are injuries to ligaments, the tough bands of tissue that connect bones to each other. They typically occur from twisting or wrenching movements. An ankle sprain, for example, is often caused by a sudden inversion or eversion of the foot. The severity of the sprain is graded based on the extent of ligament damage, from a mild stretching to a complete tear.
The mechanism of injury, such as a sudden twisting motion, is essential for determining the severity and appropriate treatment.
Strains
Strains involve overstretching or tearing of muscles or tendons. These injuries are frequently seen in sports activities or sudden movements. For instance, a hamstring strain might occur during a quick change of direction or a forceful kicking motion. The mechanism of injury, characterized by a sudden, forceful contraction or stretch of the muscle, is key to diagnosis.
Treatment typically involves rest, ice, compression, and elevation (RICE).
Table of Traumatic Lower Leg Injuries, Causes of lower leg pain
| Injury Type | Symptoms | Recommended Treatments |
|---|---|---|
| Fracture (e.g., tibia, fibula) | Severe pain, swelling, bruising, inability to bear weight, deformity, crepitus (a grating sound or feeling). | Immobilization (cast or splint), pain management, physical therapy, possible surgery. |
| Sprain (e.g., ankle sprain) | Pain, swelling, bruising, instability, limited range of motion. | RICE (Rest, Ice, Compression, Elevation), pain relievers, physical therapy, bracing. |
| Strain (e.g., hamstring strain) | Pain, tenderness, swelling, muscle weakness, limited range of motion, possible palpable defect. | RICE, pain relievers, physical therapy, strengthening exercises. |
Overuse Injuries: Causes Of Lower Leg Pain
Lower leg pain can stem from various causes, and overuse injuries are a significant contributor. These injuries result from repetitive stress and strain on the muscles, tendons, and bones in the lower leg, often without adequate time for recovery. Understanding these injuries is crucial for prevention and effective treatment.Repetitive movements, whether from exercise, work, or daily activities, can gradually damage the tissues in the lower leg.
This damage accumulates over time, leading to inflammation, pain, and ultimately, potential injury. Factors such as improper form, inadequate rest, and lack of appropriate conditioning can exacerbate the risk of overuse injuries.
Common Overuse Injuries
Overuse injuries are a common cause of lower leg pain, often arising from repetitive stress and strain on the muscles, tendons, and bones. This repetitive stress can lead to inflammation, pain, and ultimately, injury.
Shin Splints
Shin splints are a painful condition affecting the shin bone, typically caused by repetitive stress on the muscles and tissues around the tibia. Overuse during activities like running or jumping can contribute to this. Pain along the inner or outer edge of the shin, often worse after exercise, is a key symptom. In severe cases, swelling and tenderness may be present.
Stress Fractures
Stress fractures are tiny cracks in the bone, typically resulting from repeated stress and micro-trauma. These are more likely to occur in individuals with weakened bones, or those who rapidly increase the intensity or duration of their activity. Symptoms include pain that worsens with activity, localized tenderness, and sometimes swelling. The pain is often sharp and persistent, distinguishing it from other types of lower leg pain.
Lower leg pain can stem from various issues, like muscle strains or poor posture. But did you know that certain herbal remedies, like eucommia, might play a role in alleviating some of these aches? Learning more about eucommia and its potential benefits could be insightful for understanding the holistic approach to treating lower leg pain. For instance, what you need to know about eucommia can shed light on its potential medicinal properties.
Ultimately, pinpointing the exact cause of your lower leg pain requires a consultation with a healthcare professional.
Tendinopathy (Tendinitis and Tendinosis)
Tendinopathy encompasses a range of conditions involving the tendons, which connect muscles to bones. Repetitive movements, poor biomechanics, or muscle imbalances can lead to inflammation (tendinitis) or degenerative changes (tendinosis) in the tendons of the lower leg. Pain, tenderness, and sometimes swelling around the affected tendon are common symptoms. Tendinopathy often develops gradually, with pain increasing with activity.
Table: Overuse Injuries, Causes, and Prevention
| Injury | Causes | Preventative Measures |
|---|---|---|
| Shin Splints | Repetitive stress on muscles and tissues around the tibia, improper running form, inadequate warm-up, lack of flexibility, poor footwear, and increasing activity too quickly. | Gradual increase in activity, proper running form, stretching, supportive footwear, adequate rest, and warm-up before exercise. |
| Stress Fractures | Repeated stress and micro-trauma to the bone, insufficient bone density, rapid increase in activity intensity, poor bone health, and improper nutrition. | Gradual increase in activity, adequate rest, maintaining good bone health through nutrition and weight-bearing exercise, and ensuring proper footwear for the activity. |
| Tendinopathy | Repetitive stress on tendons, muscle imbalances, poor biomechanics, improper warm-up, and lack of flexibility. | Gradual increase in activity, appropriate warm-up and cool-down, stretching, maintaining good flexibility and strength, proper footwear, and addressing any muscle imbalances. |
Nerve-Related Conditions
Lower leg pain can stem from various nerve-related issues. These conditions often involve compression or irritation of nerves, leading to pain, numbness, tingling, and weakness. Understanding these conditions is crucial for proper diagnosis and treatment. Identifying the specific nerve affected and the underlying cause is essential for effective management.
Nerve Entrapment Syndromes
Nerve entrapment syndromes occur when nerves are compressed or constricted by surrounding tissues, leading to pain, numbness, and tingling. These syndromes can affect different nerves in the lower leg, resulting in diverse symptoms. Proper diagnosis is often aided by a thorough neurological examination, which evaluates sensation, reflexes, and muscle strength.
- Common nerve entrapment syndromes include tarsal tunnel syndrome, which involves the posterior tibial nerve, and common peroneal nerve entrapment. Tarsal tunnel syndrome frequently affects individuals who engage in activities that place repeated stress on the foot and ankle, like runners or dancers. Peroneal nerve entrapment can arise from direct trauma, or from chronic conditions like varicose veins.
- Symptoms of nerve entrapment syndromes can vary, depending on the specific nerve affected. Common symptoms include pain, numbness, and tingling, often worsened by activity or prolonged standing. The pain may radiate along the nerve distribution, for example, pain in the foot or ankle with peroneal nerve entrapment.
Mechanisms of Nerve-Related Pain
The mechanisms behind nerve-related pain are complex. Nerve compression can lead to inflammation, causing the release of chemicals that stimulate pain receptors. This process can cause a cascade of events, resulting in ongoing pain and potentially nerve damage. In some cases, repetitive stress or overuse can lead to nerve irritation, further contributing to the pain. Additionally, conditions like diabetes or vitamin deficiencies can increase the risk of nerve damage.
Role of Nerve Conduction Studies
Nerve conduction studies (NCS) are diagnostic tools that measure the speed and strength of electrical signals traveling along nerves. These studies can help identify nerve damage or entrapment. By comparing the results with normal values, clinicians can determine if a nerve is functioning correctly. These tests are often performed to differentiate nerve-related pain from other causes of lower leg pain.
Table of Nerve-Related Issues
| Condition | Symptoms | Potential Treatments |
|---|---|---|
| Tarsal Tunnel Syndrome | Pain, numbness, and tingling in the sole of the foot and ankle, often worsened by activity. Potential foot drop and difficulty with walking. | Rest, ice, compression, elevation, physical therapy, and in severe cases, surgery. |
| Common Peroneal Nerve Entrapment | Pain, numbness, and weakness in the lateral aspect of the foot and lower leg. Potential foot drop and difficulty with dorsiflexion (lifting the foot). | Conservative measures like splinting, physical therapy, and medications. In some cases, surgical decompression might be necessary. |
| Sciatica | Pain radiating down the leg, often associated with numbness and tingling. The pain may be triggered by movement, prolonged sitting, or coughing. | Conservative treatments like physical therapy, medication (pain relievers, anti-inflammatories), and in severe cases, surgery. |
| Diabetic Neuropathy | Numbness, tingling, and pain in the feet and legs, often progressing over time. May affect sensation and reflexes, leading to potential complications. | Management of blood sugar levels, pain medications, physical therapy, and foot care to prevent ulcers. |
Vascular Issues
Lower leg pain can stem from various vascular conditions, impacting blood flow and potentially leading to serious complications. Understanding these vascular issues is crucial for accurate diagnosis and effective treatment. The health of blood vessels in the lower leg directly affects the delivery of oxygen and nutrients to the tissues, impacting pain, swelling, and potential tissue damage. Recognizing the symptoms and potential complications associated with vascular issues is vital for prompt medical intervention.
Lower leg pain can stem from various issues, like muscle strains or poor circulation. But did you know that insulin resistance can also play a role? Addressing this often involves lifestyle changes, such as diet and exercise, and potentially exploring ways to reverse insulin resistance, like those outlined in this helpful guide on how to reverse insulin resistance.
Ultimately, understanding the root cause of your pain is key to effective treatment and finding relief.
Vascular Conditions Causing Lower Leg Pain
Blood vessel inflammation and narrowed arteries can restrict blood flow, causing pain and other symptoms in the lower leg. Various conditions can lead to these problems, ranging from relatively minor issues to more serious conditions requiring immediate medical attention. Recognizing the specific symptoms and understanding the potential complications are crucial for appropriate medical intervention.
Impact of Blood Flow on Lower Leg Pain
Adequate blood flow is essential for healthy tissue function in the lower leg. Reduced blood flow can result in oxygen deprivation and nutrient deficiency, triggering pain, numbness, and other symptoms. This deprivation can also lead to the breakdown of tissues and, in severe cases, tissue death (necrosis). The severity of the pain often correlates with the extent of the blood flow reduction.
Role of Blood Vessel Inflammation and its Symptoms
Inflammation of blood vessels, known as vasculitis, can cause lower leg pain, along with other symptoms like redness, swelling, and tenderness. These symptoms can vary depending on the severity and location of the inflammation. In some cases, the inflammation may be localized, while in others, it can affect the entire vascular system. Identifying the specific symptoms and their intensity can help in diagnosis and treatment planning.
Comparison of Vascular Issues
| Vascular Issue | Symptoms | Potential Complications |
|---|---|---|
| Peripheral Artery Disease (PAD) | Claudication (pain with walking), numbness, coolness, discoloration of skin, sores that heal slowly, hair loss, weak or absent pulses in the affected leg | Critical limb ischemia (severe reduced blood flow), amputation, heart attack, stroke |
| Deep Vein Thrombosis (DVT) | Swelling, pain, redness, warmth, tenderness in the affected leg, sometimes accompanied by fever and general malaise | Pulmonary embolism (blood clot traveling to the lungs), chronic venous insufficiency, leg ulcers |
| Raynaud’s Phenomenon | Episodes of color changes (white, blue, red) in the fingers and toes, numbness, tingling, and pain, often triggered by cold or stress | Tissue damage, skin ulcers, digital gangrene |
| Buerger’s Disease (Thromboangiitis Obliterans) | Pain, swelling, and inflammation of the blood vessels, particularly in the hands and feet. This is often associated with smoking and can lead to tissue damage, ulcers, and gangrene | Amputation, severe vascular complications |
Peripheral Artery Disease (PAD) and its Effect on Blood Flow
Peripheral artery disease (PAD) is a condition characterized by the narrowing of arteries in the extremities, particularly in the legs. This narrowing restricts blood flow, causing reduced oxygen and nutrient delivery to the lower leg tissues. Symptoms can range from mild discomfort to severe pain, particularly during exercise. PAD can affect individuals of all ages but is more prevalent in those with risk factors such as high blood pressure, high cholesterol, diabetes, and smoking.
Reduced blood flow in PAD can lead to pain during exercise (claudication) and potentially more serious complications. A significant portion of PAD cases go undiagnosed, leading to potential delays in treatment and progression of the disease.
Inflammatory Conditions

Lower leg pain can stem from various inflammatory processes within the tissues. Understanding these inflammatory conditions is crucial for accurate diagnosis and effective treatment. Inflammation, a natural response to injury or infection, involves the body’s immune system sending cells and chemicals to the affected area. This response, while vital for healing, can also cause pain and swelling if prolonged or excessive.
Types of Inflammatory Conditions
Inflammation in the lower leg can manifest in several ways, ranging from acute reactions to chronic diseases. These conditions can impact the muscles, tendons, joints, and surrounding tissues. Several conditions can lead to chronic inflammation and persistent lower leg pain.
Mechanisms of Inflammation and Pain
The body’s inflammatory response involves a complex interplay of cellular and chemical processes. Injured tissues release chemical signals, attracting immune cells to the area. These cells release further chemicals, causing increased blood flow, swelling, and heat. The release of inflammatory mediators, such as prostaglandins and cytokines, contributes significantly to pain perception. This inflammatory cascade can become problematic if it persists, leading to chronic pain and potential damage to tissues.
Examples of Inflammatory Diseases in the Lower Leg
Several inflammatory diseases can affect the lower leg, including, but not limited to, bursitis, tendonitis, and various forms of arthritis. Bursitis, for instance, is characterized by inflammation of the bursae, small fluid-filled sacs that cushion joints. Tendinitis, on the other hand, involves inflammation of tendons, the fibrous tissues connecting muscles to bones.
Lower leg pain can stem from various things, like muscle strains or poor circulation. Sometimes, dealing with chronic pain can lead to difficult decisions about care options, like considering comfort care vs hospice. comfort care vs hospice provides important information on the differences in these approaches. Ultimately, understanding the root causes of your lower leg pain is key to finding the best treatment plan.
Arthritis and Lower Leg Pain
Arthritis encompasses a group of conditions characterized by inflammation of the joints. Osteoarthritis, a common form, involves the breakdown of cartilage within the joints, leading to pain, stiffness, and reduced mobility. Rheumatoid arthritis is an autoimmune disease in which the body’s immune system attacks its own tissues, including the joints. These inflammatory processes can significantly impact the lower leg, causing pain, swelling, and decreased function in the ankles, knees, and other joints.
This can result in chronic pain and decreased mobility.
Table of Inflammatory Conditions, Symptoms, and Treatments
| Condition | Symptoms | Common Treatments |
|---|---|---|
| Bursitis | Pain, swelling, tenderness over the affected bursa; typically localized pain; may be aggravated by movement. | Rest, ice, compression, elevation; anti-inflammatory medications (NSAIDs); corticosteroid injections; physical therapy. |
| Tendinitis | Pain, tenderness, and sometimes swelling along the affected tendon; often worse with activity; localized pain. | Rest, ice, compression, elevation; anti-inflammatory medications (NSAIDs); physical therapy; stretching and strengthening exercises; orthotics. |
| Osteoarthritis | Pain, stiffness, and swelling in the affected joints; pain often worsens with activity; creaking or grating sensation in the joints. | Pain relievers (acetaminophen, NSAIDs); physical therapy; joint replacement surgery in severe cases; weight loss to reduce stress on joints. |
| Rheumatoid Arthritis | Pain, swelling, stiffness in multiple joints; often symmetrical joint involvement; fatigue, fever, and loss of appetite are common systemic symptoms. | Disease-modifying antirheumatic drugs (DMARDs); corticosteroids; physical therapy; supportive care. |
Other Potential Causes
Lower leg pain can stem from a wide range of factors, some less common than others. While conditions like muscle strains and fractures are prevalent, there are other possibilities that require careful consideration. A thorough evaluation by a healthcare professional is crucial for accurate diagnosis and appropriate treatment.
Less Common Conditions
Certain less frequent conditions can also manifest as lower leg pain. These include infections, tumors, and allergic reactions, among others. Recognizing the potential for these less common causes is vital for comprehensive patient care.
Infections
Infections, such as cellulitis or osteomyelitis, can cause significant lower leg pain. Cellulitis is a bacterial infection of the skin and underlying tissues, while osteomyelitis is a bone infection. Symptoms may include redness, swelling, warmth, and tenderness in the affected area. Prompt medical attention is essential to prevent complications.
Tumors
Tumors, both benign and malignant, can occasionally cause lower leg pain. While rare, tumors can exert pressure on nerves or blood vessels, leading to discomfort. Benign tumors typically grow slowly, whereas malignant tumors can progress more rapidly. Accurate diagnosis requires imaging studies and often a biopsy.
Allergies
Allergic reactions can sometimes present as lower leg pain, although this is less common. An allergic reaction may manifest as swelling and inflammation in the affected area. The pain could be accompanied by other symptoms, such as hives, itching, or difficulty breathing. Identifying the allergen is critical for effective treatment.
Importance of a Thorough Evaluation
A thorough evaluation by a healthcare professional is crucial for accurately diagnosing the cause of lower leg pain. A proper examination, including a detailed medical history, physical examination, and potentially imaging studies, helps distinguish between various potential causes. This process is essential to determine the most appropriate treatment plan.
Table of Potential Causes
| Cause | Description | Symptoms | Diagnosis |
|---|---|---|---|
| Infections (e.g., cellulitis, osteomyelitis) | Bacterial or fungal infections of the skin, tissues, or bone. | Redness, swelling, warmth, tenderness, fever. | Physical examination, blood tests, imaging studies (X-rays, CT scans). |
| Tumors (benign or malignant) | Abnormal growths that can press on nerves or blood vessels. | Persistent pain, swelling, changes in skin appearance, numbness. | Physical examination, imaging studies (MRI, CT scans), biopsy. |
| Allergic Reactions | An immune response to an allergen. | Swelling, inflammation, itching, hives, difficulty breathing. | Medical history, physical examination, allergy testing. |
Diagnostic Considerations
Pinpointing the exact cause of lower leg pain is crucial for effective treatment. A thorough evaluation involves understanding the patient’s medical history, performing a detailed physical examination, and potentially utilizing various diagnostic tests. This multifaceted approach helps healthcare professionals narrow down the possibilities and develop a personalized treatment plan.A comprehensive understanding of the patient’s medical history is paramount.
This includes details about any prior injuries, surgeries, or chronic conditions. The onset and duration of the pain, any associated symptoms (like swelling, redness, numbness, or tingling), and lifestyle factors (like activity level and work habits) all contribute to a more accurate diagnosis.
Medical History and Physical Examination
A detailed medical history and a thorough physical examination are essential initial steps. These evaluations provide crucial information about the potential cause of the pain. The physical examination includes careful palpation of the affected area, assessment of range of motion, neurological function checks (including sensation and reflexes), and vascular assessments. These evaluations help identify specific areas of concern and guide further diagnostic procedures.
Diagnostic Tests
Various diagnostic tests aid in identifying the underlying cause of lower leg pain. These tests provide objective data, helping to distinguish between different potential causes. The choice of test depends on the suspected etiology and the results of the initial evaluation.
| Diagnostic Test | Purpose | Limitations |
|---|---|---|
| X-rays | Detect bone fractures, dislocations, and other bony abnormalities. | May not reveal soft tissue injuries like ligament tears or muscle strains. May not show subtle stress fractures in early stages. |
| Magnetic Resonance Imaging (MRI) | Provides detailed images of soft tissues, including muscles, tendons, ligaments, and nerves. Excellent for identifying tears, inflammation, and nerve impingements. | Can be expensive and may not be suitable for patients with certain metal implants or claustrophobia. Interpretation can be complex and require specialized knowledge. |
| Computed Tomography (CT) Scan | Creates cross-sectional images of the body, revealing bony structures and soft tissues with greater detail than X-rays. Useful for identifying complex fractures and bony abnormalities. | May expose the patient to higher radiation doses compared to X-rays. May not provide as detailed soft tissue information as MRI. |
| Ultrasound | Provides real-time images of soft tissues using sound waves. Useful for evaluating tendons, muscles, and blood vessels. Can be used to guide procedures like biopsies or injections. | Limited penetration depth, making it less suitable for deep structures. Image quality can be affected by body habitus and overlying structures. |
| Blood Tests | Assess for inflammation markers (like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP)), infections, or other systemic conditions. | May not always pinpoint the specific cause of lower leg pain, but they can help rule out certain systemic conditions. Results may not always correlate immediately with the onset of pain. |
Imaging Techniques
Imaging techniques are crucial for visualizing the structures of the lower leg. X-rays provide basic views of bones, while MRI offers detailed images of soft tissues. CT scans offer a balance between bone and soft tissue visualization. Ultrasound provides real-time images of moving structures, like blood vessels. These techniques are often used in combination to gain a comprehensive picture of the injury or condition.For example, a patient with a suspected stress fracture might undergo X-rays to confirm the presence of a fracture line.
If soft tissue involvement is suspected, an MRI might be performed to evaluate the surrounding tendons and ligaments. An ultrasound might be used to evaluate blood flow in the affected area if vascular issues are suspected.
Final Thoughts
In conclusion, lower leg pain can stem from a multitude of factors, emphasizing the need for a thorough evaluation to pinpoint the underlying cause. This guide has explored the diverse range of potential culprits, from common overuse injuries to less frequent conditions. Remember, proper diagnosis and treatment are crucial for alleviating pain and promoting overall well-being. Seeking professional medical advice is essential for accurate diagnosis and effective management of lower leg pain.

