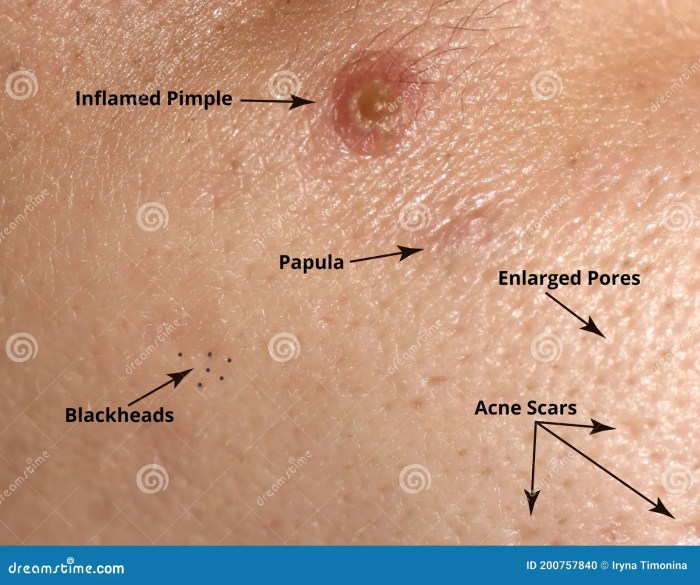
Papule definition of an acne papule delves into the specifics of this skin condition. Understanding what constitutes an acne papule is key to effective management and treatment. This in-depth exploration covers everything from defining the papule itself to examining its causes, symptoms, and available treatments. Acne papules are small, solid bumps on the skin. They’re…
Category: Skin Conditions
Ringworm vs Eczema Symptoms A Deep Dive
Ringworm vs eczema symptoms: Understanding the differences between these skin conditions is crucial for proper diagnosis and treatment. Both can cause frustrating itching, redness, and scaling, making it challenging to distinguish them at first glance. This comprehensive guide will explore the overlapping symptoms, unique characteristics, and diagnostic considerations for each condition, helping you gain a…
Sebaceous Hyperplasia Causes, Symptoms, and Treatments
Sebaceous hyperplasia causes symptoms and treatments are explored in detail. This comprehensive guide dives into the causes, symptoms, and various treatment options for sebaceous hyperplasia, a common skin condition. We’ll examine the underlying reasons for its development, the visible signs it presents, and the different approaches to managing it. Understanding this condition empowers individuals to…
Skin Pain in Psoriasis A Deep Dive
Skin pain in psoriasis is a significant concern for many sufferers, impacting their daily lives and overall well-being. This detailed exploration delves into the various types of pain, their mechanisms, and the factors that exacerbate them. We’ll also examine the profound impact on daily routines, mental health, and social interactions. Further, we’ll discuss diagnosis, management…
Atopic Dermatitis vs Eczema A Deep Dive
Atopic dermatitis vs eczema – are they the same thing? This exploration delves into the similarities and differences between these skin conditions, highlighting their often-overlapping nature. We’ll uncover the historical understanding, examine the underlying causes, and explore the nuances of diagnosis and management. Understanding these distinctions is key to providing the best possible care for…
How to Diagnose Hidradenitis Suppurativa
How to diagnose hidradenitis suppurativa is a crucial step in receiving appropriate treatment. This comprehensive guide delves into the various methods used by healthcare professionals to identify this chronic skin condition. From initial symptoms and physical examinations to diagnostic imaging and histological evaluations, we’ll explore the key aspects of accurate diagnosis. Understanding the diverse presentations…
Psoriasis Treatments That Are Fast
Psoriasis treatments that are fast are a top priority for those seeking relief from this chronic skin condition. This guide delves into various treatment approaches, from topical creams to systemic medications and phototherapy, highlighting methods known for quicker results. We’ll explore the mechanisms of action, potential side effects, and typical timelines for each, ultimately empowering…
What is Acral Peeling Skin Syndrome? A Deep Dive
What is acral peeling skin syndrome? This condition, characterized by skin peeling primarily on the extremities, presents a fascinating interplay of genetics, environment, and potential causes. Understanding its characteristics, causes, diagnosis, management, and prognosis is crucial for those affected and healthcare professionals alike. This comprehensive exploration delves into the complexities of this often-misunderstood syndrome, offering…