Light therapy lamps for sad offer a unique approach to boosting mood, and this exploration delves into the science and practicalities behind this method. We’ll examine different lamp types, their potential benefits and risks, and how they might fit into your life. This guide will also compare light therapy to other treatment options, provide safety…
Category: Mental Health
What Does Low Serotonin Feel Like? Unveiling the Impact
What does low serotonin feel like? This exploration dives deep into the often-misunderstood world of low serotonin levels, revealing the multifaceted impact they can have on your well-being. We’ll examine the emotional, physical, cognitive, social, and even behavioral changes that can accompany these lower-than-normal serotonin levels. From subtle mood fluctuations to more pronounced symptoms, understanding…
How Long Do Anxiety Attacks Last? Understanding Duration
How long do anxiety attacks last? This question plagues many experiencing these intense episodes. The answer isn’t straightforward, as attack duration varies significantly based on numerous factors. Understanding these factors, from the initial trigger to the role of individual responses, is key to navigating and managing anxiety. This exploration delves into the multifaceted nature of…
Quality Sleep While Taking Cymbalta
Quality sleep while taking Cymbalta can be a challenge for many, but understanding the potential effects and strategies to manage them can make a significant difference. This comprehensive guide explores the relationship between Cymbalta and sleep, from its mechanism of action to individual experiences, and offers practical advice for navigating sleep issues effectively. This exploration…
How Depression Is Treated A Comprehensive Guide
How depression is treated sets the stage for this enthralling narrative, offering readers a glimpse into the multifaceted approaches to managing this challenging condition. From medication and therapy to lifestyle changes and support systems, this guide delves into the various strategies used to effectively treat depression. It’s a journey into understanding the diverse needs of…
How Long Does Klonopin Take to Work?
How long does klonopin take to work? Understanding the factors influencing Klonopin’s effectiveness is crucial for managing anxiety or other conditions. This journey explores the various factors impacting its onset, from dosage and administration method to individual patient responses and potential side effects. We’ll delve into the science behind Klonopin’s action and discuss how individual…
Major Depressive Disorder Medications A Comprehensive Guide
Major depressive disorder medications are a crucial aspect of treatment for those struggling with this condition. This guide delves into the various types of medications used, exploring their mechanisms of action, effectiveness, and potential side effects. We’ll also examine factors influencing medication selection, patient adherence strategies, and emerging treatment directions. Get a deeper understanding of…
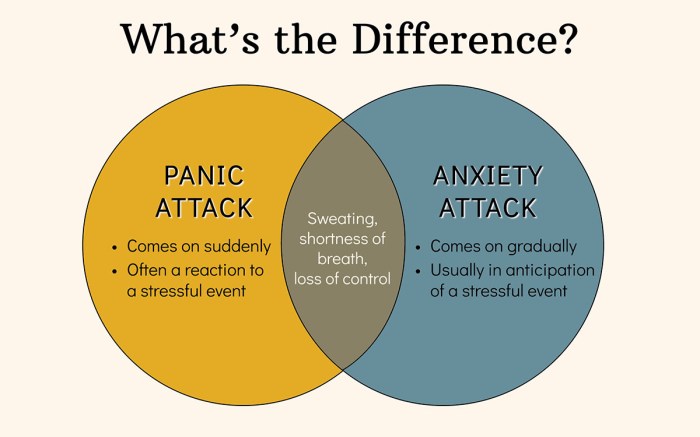
Panic Attack vs Anxiety Attack Understanding the Differences
Panic attack vs anxiety attack: This exploration delves into the nuances of these two closely related yet distinct emotional experiences. Understanding their differences is crucial for effective management and treatment. From the physiological responses to the psychological impact, we’ll unravel the complexities of each, highlighting key similarities and contrasting features. This comprehensive guide aims to…
Fear of Getting Sick A Deep Dive
Fear of getting sick sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. This fear, often rooted in psychological factors, can manifest in a variety of ways, impacting everything from daily routines to social interactions. We’ll explore the…
Fear of Lizards Herpetophobia Explained
Fear of lizards herpetophobia – Fear of lizards, herpetophobia, is a fascinating and often misunderstood anxiety. It delves into the complex world of phobias, exploring the origins, triggers, and various manifestations of this specific fear. From the biological and psychological factors to the societal and cultural influences that shape our perceptions of these creatures, we’ll…