Pain in back of knee when walking can be debilitating, impacting daily activities and overall well-being. This comprehensive guide delves into the various potential causes, from simple muscle strains to more complex conditions, offering insights into diagnosis, treatment, and prevention strategies. We’ll explore the anatomy of the knee, differentiating between different types of pain, and…
Category: Health & Wellness
Recording Family Medical History A Guide
Recording family medical history sets the stage for proactive health management. This detailed guide explores the crucial importance of documenting family health information, from understanding its significance to practical methods for collection, storage, and sharing. It will equip you with the knowledge and tools to create a comprehensive family health record, empowering you to make…
Best Time to Take Collagen Your Absorption Guide
Best time to take collagen sets the stage for a deep dive into optimizing your collagen supplement routine. Understanding how your body absorbs collagen is key to maximizing its benefits. Factors like meal timing, blood sugar levels, digestive health, and even the specific form of collagen you choose all play a role in how effectively…
How to Shrink Fibroids A Comprehensive Guide
How to shrink fibroids? This comprehensive guide delves into the various methods, medical treatments, and lifestyle adjustments that can help manage and potentially reduce fibroid size. We’ll explore the science behind fibroids, from their causes and diagnosis to the potential benefits and drawbacks of different approaches. Understanding the complexities of fibroids is crucial for anyone…
Abdominal Migraine in Adults Causes & Prevention
Abdominal migraine in adults causes and prevention is a crucial topic for understanding and managing this often-misunderstood condition. It’s not just about stomach aches; it’s a complex neurological event that can significantly impact daily life. This in-depth look explores the causes, symptoms, and potential preventative measures for abdominal migraines, helping you understand how to navigate…
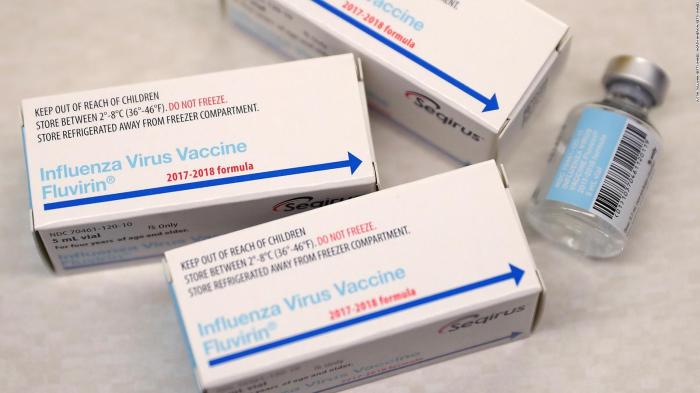
Preservative-Free Flu Vaccine A Deep Dive
Preservative free flu vaccine – Preservative-free flu vaccine is a significant advancement in immunization, offering a potentially safer alternative to traditional flu shots. This exploration delves into the history, safety, manufacturing, and public health implications of this evolving approach to influenza prevention. We’ll examine the reasons behind the shift towards preservative-free options and compare them…
Does Pickle Juice Help With Cramps? A Deep Dive
Does pickle juice help with cramps? This question sparks curiosity and debate, especially among those seeking natural remedies for menstrual discomfort. This comprehensive exploration delves into the science, history, and potential risks associated with using pickle juice to ease cramps. We’ll examine the possible mechanisms, potential risks, and compare this folk remedy with conventional pain…
Gargling Salt Water for Sore Throat A Guide
Gargling salt water for sore throat is a time-honored remedy, often used to soothe a scratchy or painful throat. This guide delves into the history, process, safety, and potential benefits of this simple yet effective practice. We’ll explore the science behind its effectiveness, compare it to other home remedies, and highlight important safety considerations. Whether…
Vitiligo vs Albinism Whats the Difference?
Vitiligo vs albinism what s the difference – Vitiligo vs albinism: what’s the difference? This exploration delves into the distinct characteristics, underlying mechanisms, and impacts of these conditions. Understanding the nuances between vitiligo and albinism is crucial for accurate diagnosis and effective support. We’ll examine their physical manifestations, genetic origins, and the challenges faced by…
Thyroid Disease Dry Mouth A Deep Dive
Thyroid disease dry mouth is a common issue that affects many people. This comprehensive guide explores the connection between these two conditions, delving into the causes, symptoms, diagnosis, treatment, and impact on quality of life. We’ll look at the role of the thyroid gland, understand how it affects saliva production, and explore the various ways…