Rehabilitation protocol after a total knee replacement is crucial for a successful recovery. This guide breaks down the process into distinct phases, from the initial weeks to long-term considerations. Understanding the exercises, activities, and important aspects of recovery can help you achieve optimal results and minimize potential complications. This protocol covers everything from the early…
Category: Health & Fitness
The Six-Minute Walk Test A Comprehensive Guide
The six minute walk test – The six-minute walk test (6MWT) is a valuable assessment tool used to measure a person’s functional capacity, particularly in individuals with respiratory conditions or other health concerns. This test provides a standardized measure of how far a person can walk in six minutes, offering crucial insights into their physical…
Exercises for Arthritic Knees A Guide
Exercises for arthritic knees are crucial for managing pain and improving mobility. This guide provides a comprehensive overview of various exercises, tailored to different levels of knee arthritis severity. We’ll explore different types of exercises, safety precautions, and how to design a personalized program to help you stay active and comfortable. From strengthening to flexibility,…
Swimming for Weight Loss Your Aquatic Journey
Swimming for weight loss is a fantastic way to shed pounds and sculpt a healthier you. It’s a low-impact exercise that’s easy on the joints, making it ideal for all fitness levels. This comprehensive guide dives deep into the world of aquatic workouts, exploring the science behind calorie burning, various swimming strokes, effective workout plans,…
Does Drinking Water Help You Lose Weight?
Does drinking water help you lose weight? This intriguing question delves into the surprising ways hydration can influence your body’s metabolism, appetite, and overall calorie intake. We’ll explore the science behind how water impacts your body’s functions and whether it can truly be a key player in your weight loss journey. From boosting metabolism to…
Start Exercising for Obesity Treatment A Guide
Start exercising for obesity treatment is crucial for a healthier lifestyle. This comprehensive guide dives deep into the physiological benefits of exercise for weight management, exploring various exercise types and personalized plans. We’ll uncover how exercise impacts metabolism and calorie expenditure, and how to seamlessly integrate it with a balanced diet. Beyond weight loss, we’ll…
How to Increase Lung Capacity Your Guide
How to increase lung capacity is a journey to better respiratory health, opening doors to enhanced athletic performance and overall well-being. Understanding the factors influencing lung capacity, from breathing techniques to lifestyle choices, is key to unlocking your body’s full potential. This guide delves into various aspects, from the science behind breathing exercises to the…
What to Wear to Physical Therapy Your Guide
What to wear to physical therapy is more important than you might think. Choosing the right clothes can significantly impact your comfort, performance, and even your mindset during your sessions. This guide will equip you with the knowledge to select clothing that optimizes your therapy experience, from comfortable fabrics to temperature regulation and specific exercise…
Exercises for Ankylosing Spondylitis A Guide
Exercises for ankylosing spondylitis are crucial for managing this chronic inflammatory condition. This guide delves into the types of exercises, routines, and considerations needed to effectively incorporate movement into your life with AS. We’ll explore everything from personalized programs to lifestyle integration and how exercise impacts your overall well-being. Understanding the specific needs of those…
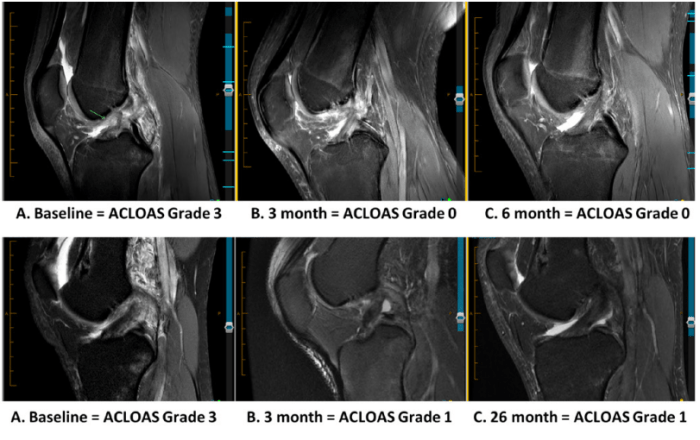
ACL Tears After Surgery A Comprehensive Guide
ACL tears after surgery present a unique challenge, requiring careful consideration of the recovery process. This guide delves into the complexities of ACL reconstruction, from surgical techniques to potential complications and the crucial role of post-surgical rehabilitation. Understanding the nuances of this journey is key to successful outcomes. Anterior cruciate ligament (ACL) tears are a…