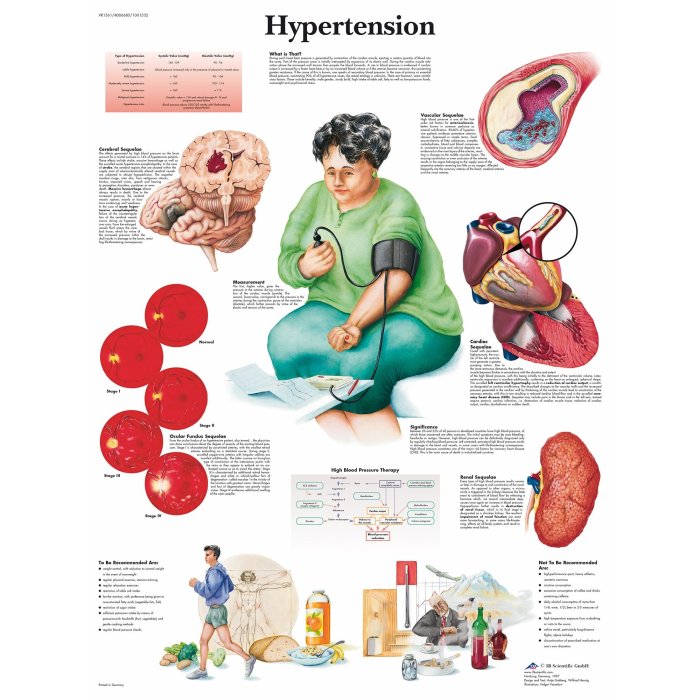
All about hypertension diagnosis: Understanding high blood pressure is crucial for maintaining good health. This in-depth guide explores the complexities of diagnosing hypertension, from initial evaluation to specialized testing and considerations for specific populations. We’ll delve into the different methods, from clinical assessments to lab tests, and provide a clear picture of the diagnostic process….
Category: Health and Wellness
Ringing in Ears Symptoms, Causes, and Treatment
Ringing in ears symptoms causes and treatment is a complex issue affecting many people. This comprehensive guide explores the various aspects of tinnitus, from understanding its different types and symptoms to exploring potential causes, diagnosis methods, and a range of treatment options. We’ll delve into lifestyle modifications and management strategies, including coping mechanisms and stress…
Are Smoothies Good for You? A Deep Dive
Are smoothies good for you? This exploration delves into the nutritional value, health benefits, potential drawbacks, and more. We’ll examine the ingredients, preparation methods, and how smoothies fit into a balanced lifestyle. From the vitamins and minerals packed into various fruits and vegetables, to the potential pitfalls of excessive consumption, this guide will equip you…
Waist Circumference and Diabetes A Comprehensive Guide
Waist circumference and diabetes are intricately linked. Understanding the relationship between abdominal fat, insulin resistance, and the risk of developing diabetes is crucial. This guide delves into the various aspects of waist circumference measurement, its impact on diabetes risk assessment, and strategies for effective management. Waist circumference is a simple yet powerful indicator of central…
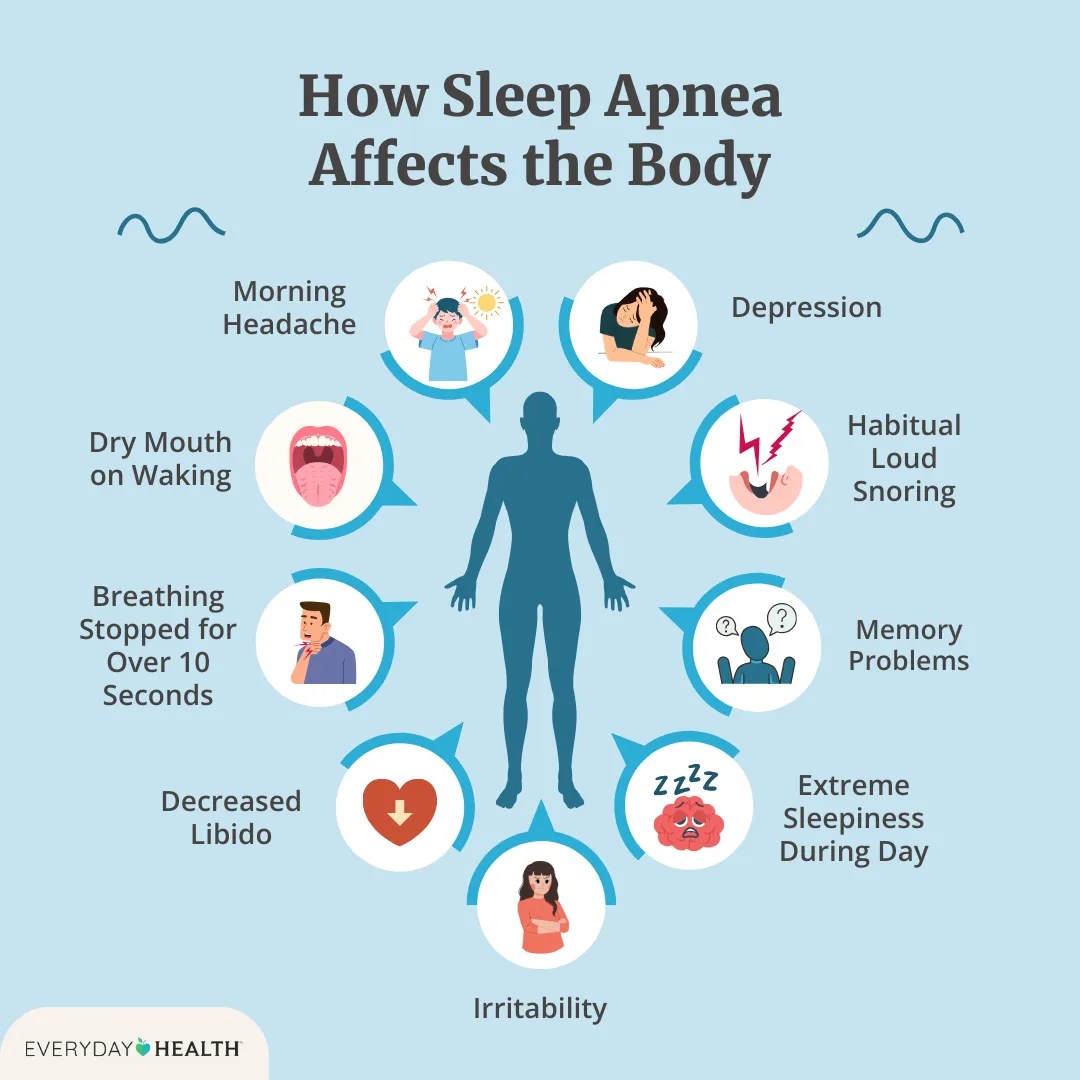
Effects of Sleep Apnea A Deep Dive
Effects of sleep apnea extend far beyond just feeling tired. This comprehensive exploration delves into the various ways sleep apnea impacts your overall health, from the cardiovascular system to cognitive function. We’ll uncover the different types, symptoms, and potential long-term consequences of this often-overlooked condition. Understanding these effects is crucial for early detection and effective…
HER2 Negative Breast Cancer Diet A Guide
HER2 negative breast cancer diet is crucial for navigating treatment and recovery. This guide delves into essential dietary considerations, covering everything from balanced nutrition to managing treatment side effects. We’ll explore specific nutrients, food groups, and dietary approaches, along with practical tips and recipes to support your journey. From understanding the impact of different foods…
Netflix Apple Cider Vinegar Cancer Treatment A Critical Look
Netflix Apple Cider Vinegar Cancer Treatment claims are circulating widely, sparking concern and confusion. This blog delves into the prevalence of these claims on Netflix and other platforms, examining the scientific basis, potential misinformation, public perception, and the broader health implications of such beliefs. We’ll analyze the potential harm of substituting proven cancer treatments with…
Exercise for Dementia Prevention
How regular exercise could lower your risk of dementia is a compelling topic. Physical activity isn’t just good for your body; it’s crucial for brain health, potentially staving off cognitive decline. This exploration delves into the mechanisms by which exercise might protect against dementia, highlighting different types of exercise, their impact, and the science behind…
Two Dates a Day for Health Benefits A Deep Dive
Two dates a day for health benefits: This post explores the potential advantages of incorporating two dates daily into your diet. From understanding the nutritional powerhouse that dates are, to learning how to incorporate them into various meals and snacks, we’ll cover everything you need to know. We’ll examine different date types, preparation methods, potential…
MCT Oil Benefits, Side Effects, and More
Mct oil benefits side effects and more – MCT oil benefits, side effects, and more – a comprehensive exploration awaits. This in-depth look dives into the world of medium-chain triglycerides (MCTs), examining their potential health benefits, possible drawbacks, and practical applications. From weight management to cognitive function, we’ll cover it all, providing a balanced perspective…