Breast cancer treatment aging study examines how age impacts the effectiveness and side effects of various therapies. This in-depth exploration considers the diverse factors influencing treatment decisions for patients of different ages, from the available treatment options today to the challenges faced by older adults. It delves into research findings, highlighting the varying responses to…
Category: Health and Wellness
Information and History About Vaccination and Vaccines A Deep Dive
Information and history about vaccination and vaccines sets the stage for this enthralling narrative, offering readers a glimpse into a story that is rich in detail and brimming with originality from the outset. We’ll journey through time, examining the groundbreaking scientific advancements, the societal impact, and the ongoing challenges and opportunities in the field of…
Collagen for Rheumatoid Arthritis A Deep Dive
Collagen for rheumatoid arthritis: Understanding this potential treatment option requires a deep dive into the complexities of both conditions. Rheumatoid arthritis, a chronic autoimmune disease, attacks the body’s own tissues, particularly the joints. This inflammation can lead to significant pain, stiffness, and decreased mobility. The body’s natural collagen production, crucial for joint health, may be…
Understanding Atonic Seizures What You Need to Know
What are atonic seizures? These are a type of seizure characterized by a sudden loss of muscle tone, leading to a brief period of falling or collapsing. Understanding their causes, symptoms, and treatment is crucial for those affected and their loved ones. This comprehensive guide delves into the intricacies of atonic seizures, providing valuable insights…
Rheumatoid Arthritis Treatment Not Working A Guide
Rheumatoid arthritis treatment not working can be incredibly frustrating. It’s a journey filled with emotional ups and downs, where hope clashes with disappointment. This guide delves into the complexities of ineffective treatment, offering practical strategies for navigating the challenges and exploring alternative pathways. Understanding the reasons why a treatment isn’t working is crucial. We’ll explore…
What Should My Normal Peak Flow Be? A Guide
What should my normal peak flow be? This question is crucial for anyone concerned about their lung health, particularly those with conditions like asthma. Understanding your peak flow readings is essential for monitoring your respiratory function and taking proactive steps towards better well-being. This guide dives deep into peak flow measurement, from the basics to…
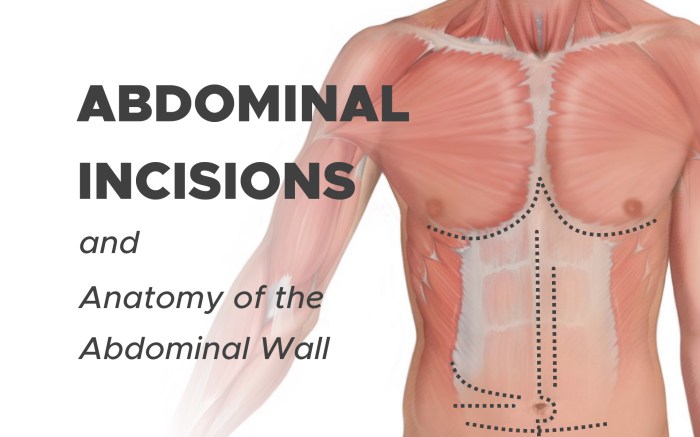
Abdominal Swelling and Bloating Understanding the Causes
Abdominal swelling and bloating can be uncomfortable and frustrating. This comprehensive guide explores the various aspects of this common issue, from defining the symptoms to understanding potential causes, diagnostic procedures, and effective treatment options. We’ll delve into the physiological mechanisms behind the distention, differentiate between types of swelling, and discuss the role of different organs…
RSV and Rash Symptoms Link and Treatment
RSV and rash symptoms link and treatment is a crucial topic for parents and caregivers. Understanding the connection between Respiratory Syncytial Virus (RSV) and skin rashes can help in early diagnosis and appropriate management. This comprehensive guide explores the various types of rashes associated with RSV, their symptoms, potential causes, diagnostic methods, treatment strategies, and…
Can Allergies Cause a Fever? Understanding the Link
Can allergies cause a fever? This question delves into the intricate relationship between allergic reactions and elevated body temperature. Allergies, encompassing a spectrum of immune responses to foreign substances, often manifest as uncomfortable symptoms like sneezing, itching, and rashes. However, the connection to fever is less straightforward. While a fever is frequently associated with infections,…
Study Links Sleep Pattern to Successful Aging
Study links this sleep pattern to successful aging, revealing a fascinating connection between slumber and healthy aging. This research delves into a specific sleep pattern, exploring its characteristics, correlations with successful aging, and potential mechanisms. Understanding this sleep pattern could lead to valuable interventions for promoting healthy aging and well-being in older adults. The study…