Neck and shoulder pain on left side – Neck and shoulder pain on the left side can be debilitating, impacting daily life. This in-depth exploration delves into the potential causes, symptoms, diagnosis, treatment, and prevention strategies for this common issue. We’ll uncover everything from musculoskeletal problems to neurological conditions, and discuss how lifestyle factors can…
Category: Health and Wellness
The Benefits of Red Clover A Comprehensive Guide
The benefits of red clover extend far beyond its charming name. This comprehensive guide delves into the fascinating world of red clover, exploring its historical uses, nutritional profile, potential health benefits, and even its culinary applications. We’ll uncover the secrets of this versatile plant, from its botanical classification to its role in various industries. From…
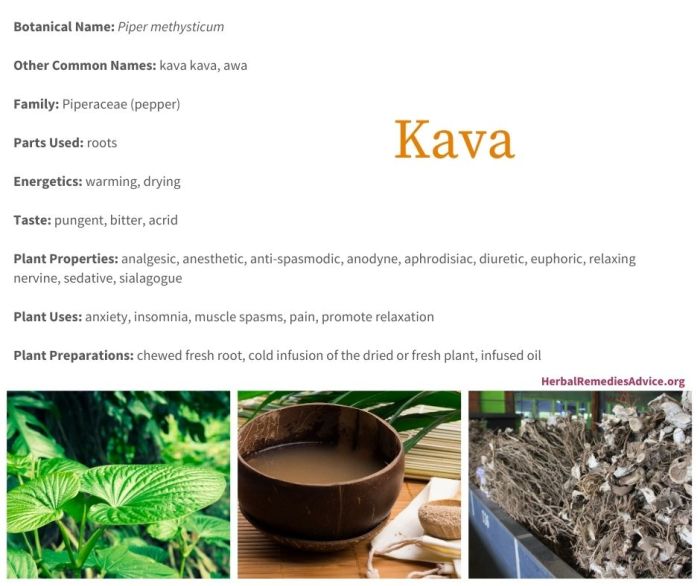
Kava Uses Risks and More
Kava uses risks and more are a complex topic, and this exploration dives deep into the world of kava, from its traditional uses to potential modern applications, alongside the important risks associated with its consumption. We’ll look at the rich history and cultural significance of kava, and examine the chemical compounds that make it unique….
The Benefits of Carnosine A Deep Dive
The benefits of carnosine, a naturally occurring compound, are increasingly recognized for its potential impact on muscle function, cellular health, and even neurological well-being. This exploration delves into the science behind carnosine, examining its various roles and potential applications. We’ll uncover how carnosine impacts everything from athletic performance to the aging process. Carnosine, a dipeptide…
Natural Remedies and Supplements for Gallbladder Issues
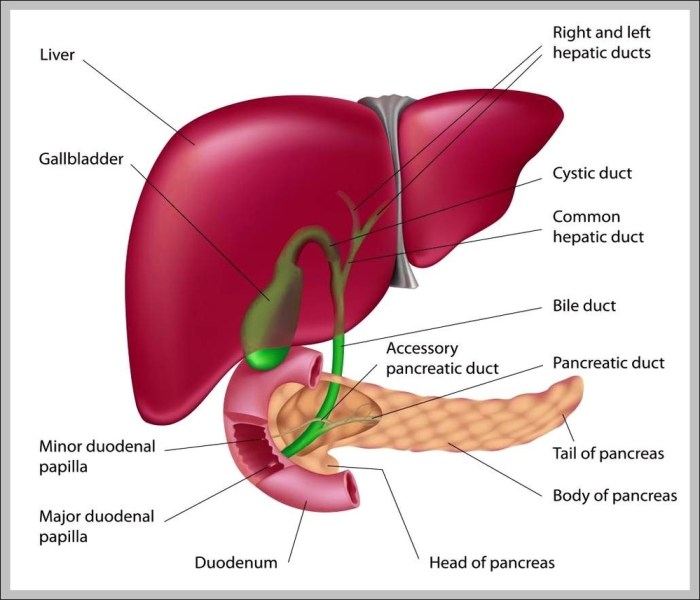
Natural remedies and supplements for gallbladder issues offer a range of potential solutions, from dietary changes to herbal remedies. Understanding how these approaches work and their potential benefits, along with potential risks, is key to making informed choices. This exploration delves into various natural strategies for gallbladder support, emphasizing the importance of consulting with a…
Gallbladder Anatomy, Function, and Treatment
The gallbladder anatomy function and treatment is a crucial topic for understanding digestive health. This exploration delves into the gallbladder’s role in the human body, from its intricate structure to the various disorders that can affect it. We’ll cover everything from its location and function in the digestive process to the different treatment options available…
What is Full Spectrum CBD? A Deep Dive
What is full spectrum CBD? It’s more than just a buzzword; it’s a complex topic encompassing plant extraction, potential benefits, and important safety considerations. This exploration delves into the intricacies of full spectrum CBD, from its definition and production methods to its potential applications and the regulations surrounding it. We’ll cover everything from the science…
The Benefits of Arnica A Deep Dive
The benefits of arnica, a plant with a long history of use in traditional medicine, are now being explored through a modern lens. This comprehensive exploration delves into the various forms of arnica, its purported healing properties, and the scientific evidence behind its use. From muscle soreness to joint pain, we’ll examine how arnica might…
Conjugated Linoleic Acid Weight Loss A Deep Dive
Conjugated linoleic acid weight loss is a popular topic, but understanding the science behind it is key. This post explores the potential benefits, drawbacks, and considerations surrounding CLA supplementation for weight management. We’ll delve into the science, examine different types of CLA, and look at how diet and exercise play a crucial role in achieving…
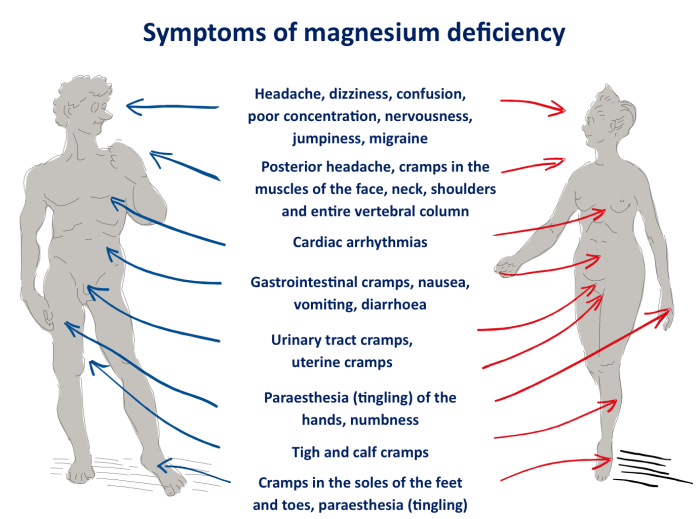
What Vitamin Deficiency Causes Muscle Cramps?
What vitamin deficiency causes muscle cramps? This comprehensive guide delves into the fascinating connection between essential vitamins and those painful muscle spasms. We’ll explore the various vitamins crucial for muscle function, and how their deficiency can trigger cramps. Understanding the specific roles of vitamins like calcium, magnesium, potassium, and vitamin D, along with their impact…