Understanding your PSA results is crucial for prostate health. This comprehensive guide delves into what a PSA test is, how results are interpreted, and the factors that can influence them. We’ll cover everything from normal ranges and potential causes of elevated PSA to the relationship between PSA levels and prostate cancer risk, as well as…
Category: Health and Wellness
Low Iron Level Causes Understanding the Factors
Low iron level causes are multifaceted, stemming from a variety of dietary, physiological, and medical factors. From dietary deficiencies to blood loss, and absorption issues, this comprehensive guide explores the intricate web of causes contributing to low iron levels. We’ll delve into the specific roles of diet, blood loss, absorption, and other potential contributing factors,…
Asthmas Daily Impact Expert Insights
Ask an expert how does asthma impact daily life? This exploration delves into the multifaceted ways asthma affects everyday routines, from physical exertion and sleep to social interactions and mental well-being. We’ll examine how varying asthma severities influence daily life, and uncover practical strategies for managing symptoms and challenges. From the subtle impact on sleep…
Gluten Intolerance vs Celiac A Deep Dive
Gluten intolerance vs celiac sets the stage for a detailed exploration of two related but distinct conditions. Understanding the nuances between them is crucial for proper diagnosis and management. This exploration will delve into the differences in their nature, mechanisms, and the impact they have on daily life. This comprehensive guide will cover the defining…
The Role of Support in Weight Loss A Crucial Factor
The role of support in weight loss sets the stage for a successful journey, highlighting how crucial encouragement and guidance are to achieving and maintaining a healthy weight. This journey isn’t just about dieting and exercise; it’s about building a support system that fosters motivation, provides practical assistance, and helps navigate the emotional ups and…
Physical Therapy for Pectus Excavatum A Deep Dive
Physical therapy for pectus excavatum provides a vital pathway to managing this condition, offering a blend of exercises and techniques to address both the physical and emotional aspects of the condition. It’s a crucial component in the overall treatment plan, helping individuals regain strength, improve posture, and enhance breathing capacity. This comprehensive guide delves into…
Can Allergies Cause Loss of Taste and Smell?
Can allergies cause loss of taste and smell? This intriguing question delves into the complex interplay between our immune system and sensory perception. Allergies, triggered by our bodies’ overreaction to harmless substances, can manifest in a wide range of symptoms, from the familiar runny nose to more subtle effects like changes in taste and smell….
Left Side Neck and Shoulder Pain Understanding the Causes
Neck and shoulder pain on left side – Neck and shoulder pain on the left side can be debilitating, impacting daily life. This in-depth exploration delves into the potential causes, symptoms, diagnosis, treatment, and prevention strategies for this common issue. We’ll uncover everything from musculoskeletal problems to neurological conditions, and discuss how lifestyle factors can…
The Benefits of Red Clover A Comprehensive Guide
The benefits of red clover extend far beyond its charming name. This comprehensive guide delves into the fascinating world of red clover, exploring its historical uses, nutritional profile, potential health benefits, and even its culinary applications. We’ll uncover the secrets of this versatile plant, from its botanical classification to its role in various industries. From…
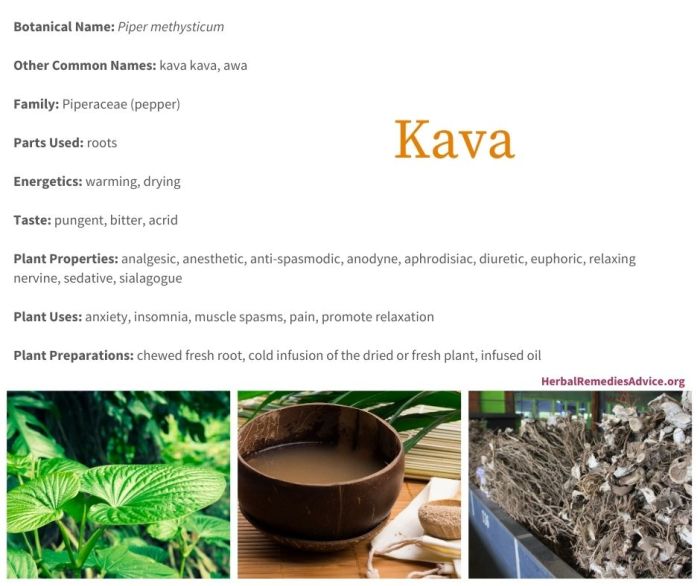
Kava Uses Risks and More
Kava uses risks and more are a complex topic, and this exploration dives deep into the world of kava, from its traditional uses to potential modern applications, alongside the important risks associated with its consumption. We’ll look at the rich history and cultural significance of kava, and examine the chemical compounds that make it unique….