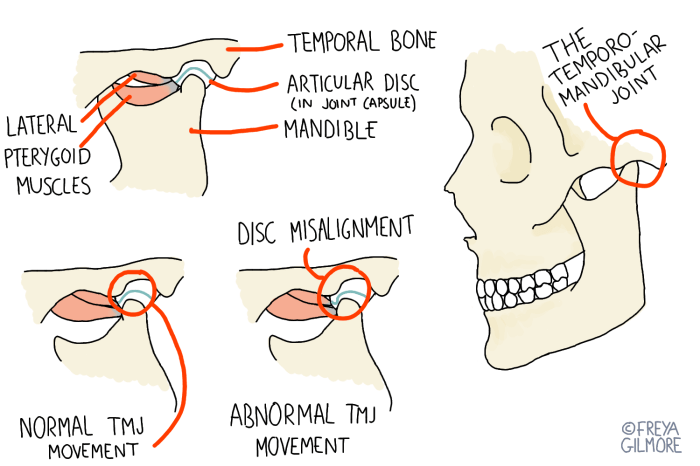
What is TMJ disorder? This comprehensive guide delves into the complexities of temporomandibular joint (TMJ) disorders, exploring everything from their intricate anatomy to effective treatment options. Understanding the structure and function of the TMJ is crucial to grasping the various types of TMJ disorders and their associated symptoms. We’ll also explore the causes, diagnosis, and…
Category: Health
Gout in the Fingers Overview and More
Gout in the fingers overview and more: Understanding this painful condition is crucial for effective management. This in-depth look explores the causes, symptoms, and treatment options for gout in the fingers, distinguishing it from other similar conditions. We’ll also delve into risk factors, prevention strategies, and the practical aspects of living with gout in the…
CLL When to Treat A Comprehensive Guide
CLL when to treat is a crucial question for patients and healthcare providers alike. This in-depth exploration delves into the complexities of chronic lymphocytic leukemia (CLL), examining the factors that influence treatment decisions, from patient characteristics to genetic mutations. We’ll explore the various treatment options available, their effectiveness, and potential side effects, ultimately providing a…
COVID-19 Coronavirus Vaccine A Comprehensive Look
Covid 19 coronavirus vaccine – COVID-19 coronavirus vaccine development has been a global race against time. From initial trials to widespread distribution, this journey has presented unprecedented challenges and triumphs. We’ll explore the scientific breakthroughs, logistical hurdles, and ethical considerations surrounding the COVID-19 vaccine rollout, including its effectiveness, impact, and the future of vaccine research….
What is the Most Common Cancer in the US?
What is the most common cancer in the US? This crucial question delves into the leading causes of cancer, highlighting the factors that influence its prevalence. We’ll explore the key statistics, examining incidence rates, mortality figures, and the role of demographics, lifestyle choices, and environmental factors in shaping these trends. Understanding the most common cancer…
Can You Get the Flu in the Summer?
Can you get the flu in the summer? While flu season is typically associated with winter, the possibility of contracting influenza during warmer months exists. Understanding the factors that influence flu transmission, and recognizing the potential symptoms, is crucial for staying healthy throughout the year. This article delves into the complexities of summer influenza, examining…
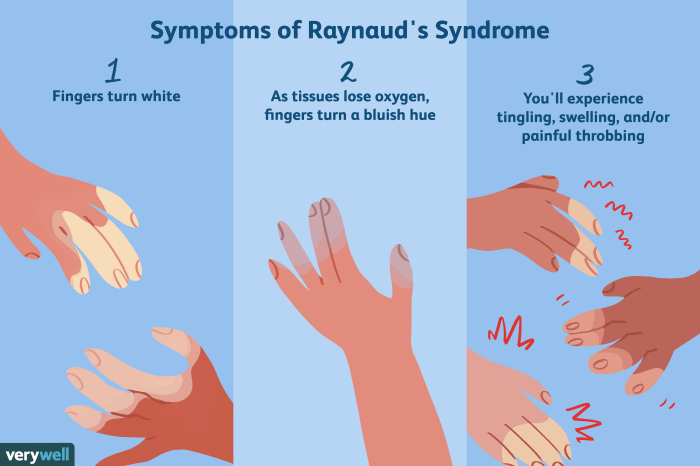
Raynauds Syndrome Chronic Fatigue A Deep Dive
Raynauds syndrome chronic fatigue – Raynaud’s syndrome chronic fatigue is a complex condition affecting many individuals. This blog post explores the overlapping symptoms, potential triggers, and challenges associated with both conditions. Understanding the potential shared mechanisms and diagnostic difficulties is crucial for effective management. Raynaud’s Syndrome manifests as episodic attacks of cold-induced numbness and color…
Can You Have Pneumonia Without a Fever?
Can you have pneumonia without a fever? This intriguing question delves into the complexities of pneumonia diagnosis, exploring the nuances of this potentially serious respiratory illness. While fever is often a prominent symptom, there are situations where pneumonia can manifest without this telltale sign. This exploration will unpack the reasons behind this variability, providing a…
Feeling of Something Stuck in Throat Causes & Solutions
Feeling of something stuck in throat can be incredibly uncomfortable and worrisome. This blog post dives deep into the possible causes, from everyday irritants to more serious medical conditions. We’ll explore potential triggers, diagnostic considerations, management strategies, and preventive measures to help you understand this common issue. From anxiety to specific foods, a variety of…
HPV Vaccine & Existing Infection Does it Help?
Does HPV vaccine help if already infected? This crucial question delves into the complex relationship between the HPV vaccine and existing infections. We’ll explore how the HPV virus works, how the vaccine protects, and the potential impact on individuals already carrying the virus. This isn’t just about preventing infection; it’s about understanding the nuanced effects…