Elderly blood sugar levels chart provides a crucial guide for understanding and managing blood sugar in older adults. Aging brings physiological changes that impact glucose metabolism, making blood sugar management more complex. This comprehensive overview delves into normal ranges, common conditions, monitoring strategies, and lifestyle considerations specific to the elderly. We’ll explore how these factors…
Author: Jaiden Mayer
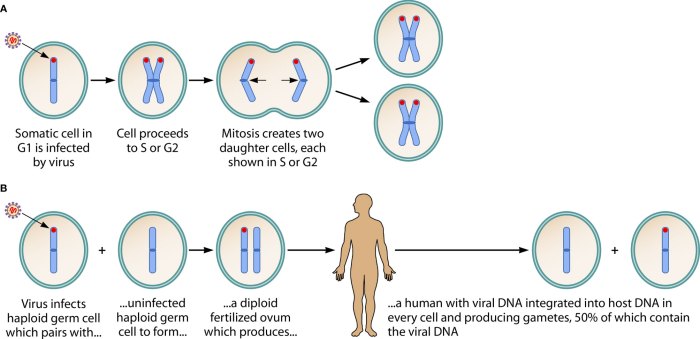
HHV-6 and Its Role in Disease A Deep Dive
Hhv 6 and its role in disease – HHV-6 and its role in disease is a fascinating area of research, exploring the intricate ways this common virus can impact human health. From its subtle presence in childhood infections to potential links with adult conditions, understanding HHV-6 is crucial for better diagnosis and treatment. This exploration…
Signs of Fibroids Breaking Down Understanding the Process
Signs of fibroids breaking down can be a complex and sometimes unsettling experience. This comprehensive guide delves into the various symptoms, potential causes, diagnostic procedures, and treatment options available. We’ll explore how these changes might manifest, potentially differing from other conditions, and examine the possible underlying factors. Understanding the process is crucial for navigating this…
When to Take Apple Cider Vinegar Your Guide
When to take apple cider vinegar is a question that often arises for those exploring its potential health benefits. This guide delves into the optimal timing for consuming apple cider vinegar, considering various factors like digestive support, weight management, and blood sugar control. We’ll explore different types, potential benefits, and crucial considerations to help you…
How Long Does It Take to Run a Marathon?
How long does it take to run a marathon? This question encapsulates a world of factors, from the runner’s training regimen to the very weather on race day. Understanding the answer requires delving into the diverse experiences of marathon runners, from beginners to seasoned veterans. A marathon is a grueling 26.2-mile test of endurance and…
IUD Use in Nulliparous Women A Deep Dive
IUD use in nulliparous women presents a unique set of considerations for women seeking long-term birth control. This comprehensive exploration delves into the various types of IUDs, their mechanisms of action, and potential side effects. We’ll specifically examine the advantages, disadvantages, and risks associated with IUD use for women who have not given birth, comparing…
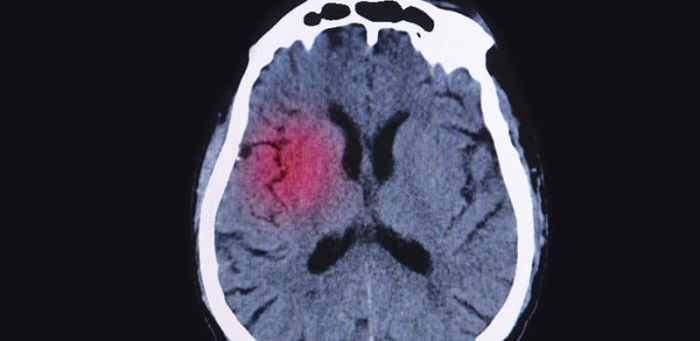
Migraine and Multiple Sclerosis Connection Unveiling the Link
Migraine and multiple sclerosis connection: This exploration delves into the intriguing relationship between these two neurological conditions. Migraines, characterized by debilitating headaches, and multiple sclerosis, a chronic autoimmune disease affecting the central nervous system, often share overlapping symptoms. Understanding this connection is crucial for accurate diagnosis and effective treatment strategies. The potential overlap in symptoms,…
Prevent Ankle Sprains Proprioception Training
Prevent ankle sprains with proprioception training is a comprehensive guide to understanding and implementing exercises that improve ankle stability and reduce the risk of injury. This in-depth exploration covers everything from the basics of ankle sprains and proprioception to practical training programs and case studies, equipping you with the knowledge to proactively safeguard your ankles….
Sign Language Games and Puzzles Fun Ways to Learn
Sign language games and puzzles offer a fantastic way to learn and practice sign language. From simple matching games to engaging charades, these activities make learning accessible and enjoyable for all ages and skill levels. This exploration delves into the history, benefits, and design of these interactive tools, highlighting how they can foster cognitive, social,…
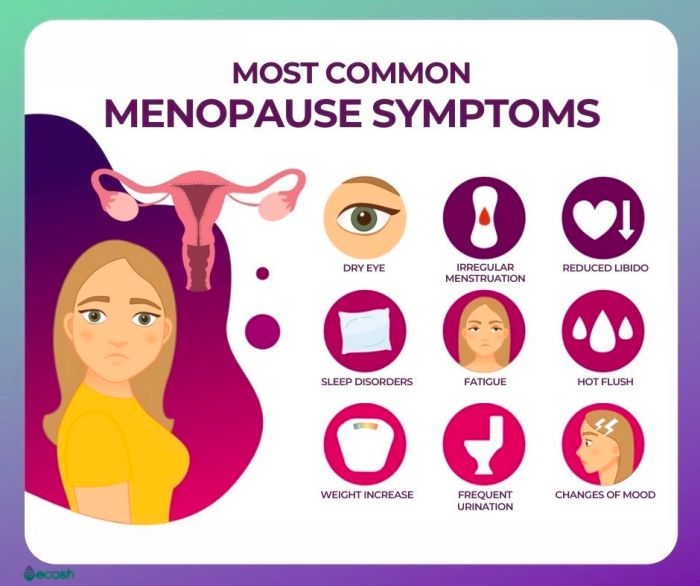
Menopause Facts and Statistics A Deep Dive
Menopause facts and statistics paint a compelling picture of this significant life transition. From global prevalence rates and demographic breakdowns to the intricate interplay of symptoms, health impacts, and management strategies, this exploration provides a comprehensive overview. Understanding the realities of menopause empowers women and healthcare professionals alike. This deep dive examines the prevalence of…