What to wear to physical therapy is more important than you might think. Choosing the right clothes can significantly impact your comfort, performance, and even your mindset during your sessions. This guide will equip you with the knowledge to select clothing that optimizes your therapy experience, from comfortable fabrics to temperature regulation and specific exercise…
Author: Jaiden Mayer
Can Fingering Give You an STD? The Truth
Can fingering give me an STD? This is a crucial question for anyone engaging in this type of intimate contact. Understanding the potential risks and taking preventative measures is key to maintaining sexual health. This discussion will explore the transmission of STIs through skin-to-skin contact, focusing on the specifics of fingering. We’ll delve into the…
Do Standing Desks Actually Help or Hype?
Do standing desks actually help or is it just hype? This question sparks debate in the world of work, and the answer isn’t as simple as a yes or no. We’ll delve into the features of standing desks, exploring the potential health benefits and drawbacks, along with ergonomic considerations for a comfortable and productive workspace….
How to Fix Ingrown Toenail A Complete Guide
How to fix ingrown toenail? This comprehensive guide dives into the world of ingrown toenails, offering insights into causes, symptoms, and effective treatment options. From simple home remedies to professional procedures, we’ll explore every aspect of managing and preventing this common foot ailment. Understanding the different types of ingrown toenails and their characteristics is crucial…
Health Insurance Birthday Rule Your Guide
The health insurance birthday rule dictates when you become eligible for coverage. It’s a crucial factor in understanding your insurance options, especially if you’re a new enrollee, have dependents, or are navigating the complexities of different insurance plans. This comprehensive guide will walk you through everything you need to know, from the basics of the…
Urine Glucose Test What It Measures, Results, Next Steps
Urine glucose test what it measures results next steps provides a crucial understanding of blood sugar levels and potential health conditions. This guide delves into the specifics of the test, from its purpose and methods to interpreting results and determining appropriate next steps. We’ll explore what the test measures, how results are interpreted, and what…
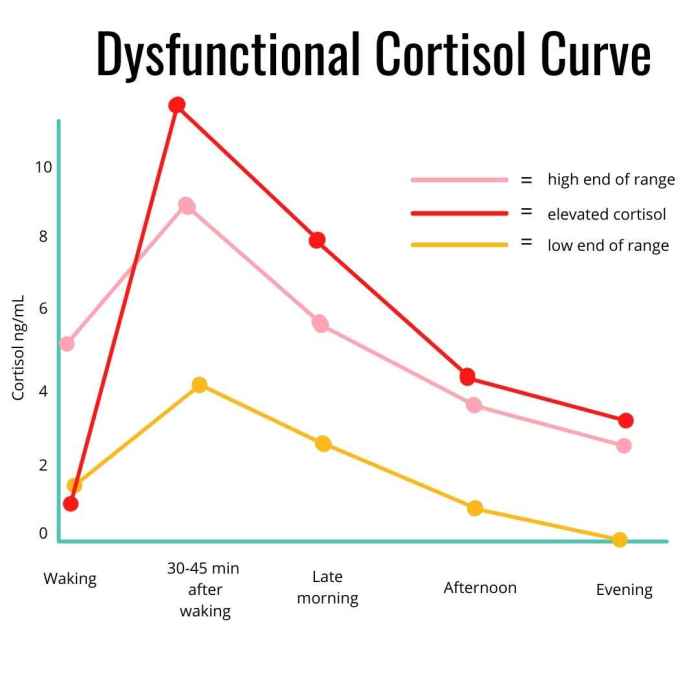
How to Lower Cortisol Your Guide
How to lower cortisol is a crucial question for anyone experiencing stress or its negative health effects. This comprehensive guide dives deep into understanding the complexities of cortisol, identifying potential causes of elevated levels, and exploring natural and lifestyle adjustments for effective management. We’ll cover everything from understanding cortisol’s role in the body to specific…
Do Fevers Cause Brain Damage? Exploring the Risks
Do fevers cause brain damage? This question is a crucial one for parents and healthcare professionals alike. While fevers are a natural part of the immune response, understanding the potential risks and protective factors is key to ensuring a healthy outcome. This blog post delves into the complex relationship between fever and brain damage, exploring…
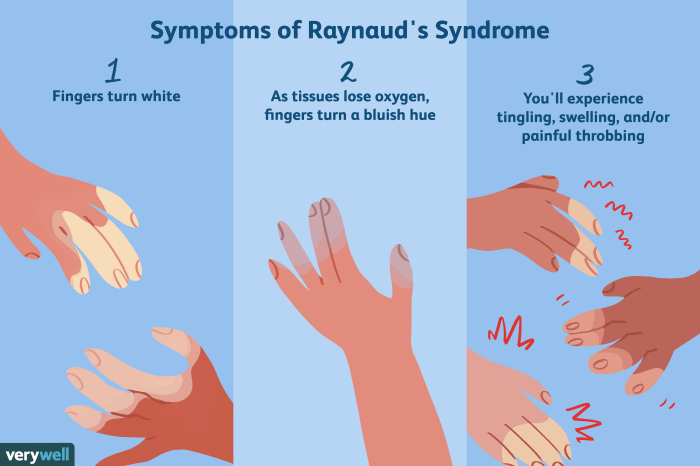
Raynauds Syndrome Chronic Fatigue A Deep Dive
Raynauds syndrome chronic fatigue – Raynaud’s syndrome chronic fatigue is a complex condition affecting many individuals. This blog post explores the overlapping symptoms, potential triggers, and challenges associated with both conditions. Understanding the potential shared mechanisms and diagnostic difficulties is crucial for effective management. Raynaud’s Syndrome manifests as episodic attacks of cold-induced numbness and color…
Ovarian Pain Causes and Treatment Explained
Ovary pain causes and treatment – Ovarian pain causes and treatment is a complex issue affecting many women. Understanding the intricacies of the female reproductive system, the various potential causes of discomfort, and the available treatment options is crucial for effective management. This exploration delves into the different types of ovarian pain, their potential origins,…