The role of support in weight loss sets the stage for a successful journey, highlighting how crucial encouragement and guidance are to achieving and maintaining a healthy weight. This journey isn’t just about dieting and exercise; it’s about building a support system that fosters motivation, provides practical assistance, and helps navigate the emotional ups and…
Author: Herman Swift
Christina Herreras Diabetes Journey
Christina herrera my journey with type 2 diabetes – Christina Herrera’s journey with type 2 diabetes sets the stage for this enthralling narrative, offering readers a glimpse into a story rich in personal detail and insightful reflections. She shares her experiences, challenges, and triumphs in managing this condition, providing valuable insights and inspiration for others…
Causes of Lower Leg Pain A Comprehensive Guide
Causes of lower leg pain can range from simple overuse injuries to more complex conditions. This guide delves into the various potential culprits behind lower leg discomfort, providing a detailed overview of the anatomy, common causes, traumatic injuries, overuse syndromes, nerve-related issues, vascular problems, inflammatory conditions, and other possibilities. We’ll explore the symptoms, diagnostic considerations,…
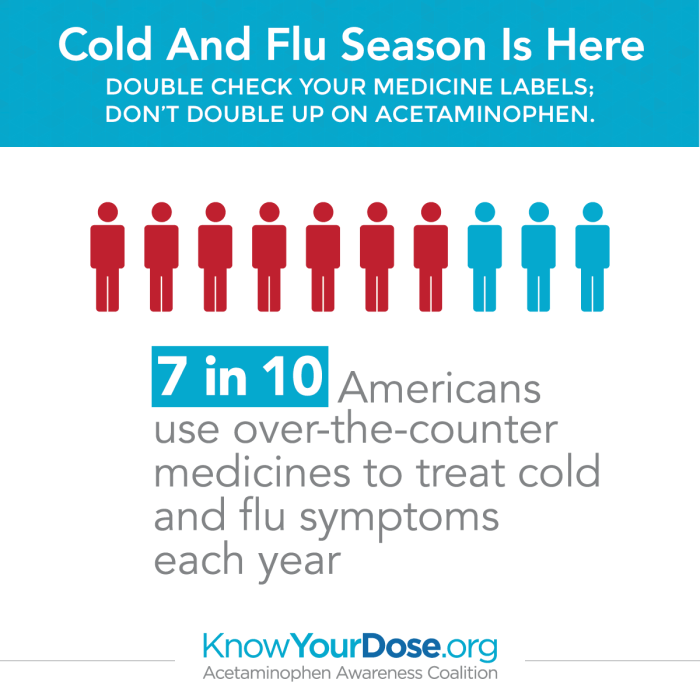
Overdosing on Cold and Flu Medications A Guide
Overdosing on cold and flu medications is a serious issue that can have severe consequences. Many people take these medications without fully understanding the risks involved. This guide explores the dangers of exceeding recommended dosages, detailing the various types of cold and flu medications prone to overdose, potential symptoms, and steps to take in case…
Tirzepatide Heart Failure Data A Deep Dive
Tirzepatide heart failure data is generating considerable interest, raising important questions about the drug’s potential cardiovascular risks. This comprehensive analysis explores the evidence, examining key studies, potential mechanisms, and the clinical implications for patients and healthcare professionals. Understanding the complexities of this emerging data is crucial for informed decision-making. This overview delves into the mechanism…
Mohs Surgery on Nose A Comprehensive Guide
Mohs surgery on nose is a specialized procedure used to treat skin cancers on the delicate nasal area. This in-depth guide explores every facet of the process, from the initial evaluation to long-term management. We’ll delve into the reasons for choosing Mohs surgery, the surgical technique, and the crucial post-operative care required for optimal outcomes….
Hypochlorous Acid Acne Body Odor A Deep Dive
Hypochlorous acid acne body odor is a topic gaining traction as a potential new treatment. This in-depth exploration examines the science behind HOCl, its potential benefits and risks for acne and body odor, and compares it to existing methods. We’ll delve into the chemical properties of HOCl, its mechanisms of action, and crucial safety considerations….
Nicotine Patches Long COVID Treatment A Deep Dive
Nicotine patches long COVID treatment is a burgeoning area of research, exploring a potential link between nicotine and alleviating the symptoms of Long COVID. This complex topic delves into the mechanisms of nicotine’s effects on the body, compares them to the symptoms of Long COVID, and examines the potential benefits, risks, and existing research. The…
Physical Therapy After Ankle Fracture Your Recovery Guide
Physical therapy after ankle fracture is crucial for a successful recovery. This comprehensive guide provides a detailed overview of the entire process, from initial rehabilitation to advanced exercises and returning to pre-injury activities. We’ll explore the different phases, common exercises, and important considerations for managing pain and potential complications. Understanding the specific exercises, the progression…
Benefits of Jumping Rope A Complete Guide
Benefits of jumping rope are surprisingly extensive, impacting both physical and mental well-being. This comprehensive guide delves into the numerous advantages, from cardiovascular improvements to stress reduction, and explores how to maximize your jump rope routine for optimal results. From boosting heart health and building muscle to aiding weight management and mental clarity, jumping rope…