Ozempic dosage strength forms and how to use is a crucial aspect of managing this medication effectively. Understanding the various strengths, forms (like injection pens and pre-filled syringes), and proper administration techniques is key to achieving optimal results. This guide delves into the details, covering everything from dosage calculations to potential side effects and storage…
Author: Ceasar Ritchie
Drugs That Cause Erectile Dysfunction A Comprehensive Guide
Drugs that cause erectile dysfunction are a significant concern for many men. This issue is often overlooked, but understanding the various medications that can lead to erectile problems is crucial for maintaining overall health and well-being. This guide will explore the mechanisms by which certain drugs impact erectile function, examining specific drug categories, underlying mechanisms,…
PCOS Truths Hidden in Plain Sight
Things no one tells you about PCOS. This isn’t just about the obvious symptoms like irregular periods and acne. It’s about the hidden struggles, the emotional toll, and the often-overlooked challenges women face navigating this condition. We’ll delve into the nuances, separating fact from fiction, and sharing real experiences that shed light on the often-unseen…
Can Receding Gums Grow Back? A Comprehensive Guide
Can receding gums grow back? This question sets the stage for a fascinating exploration into the world of gum health. We’ll delve into the causes, treatments, and long-term management strategies for receding gums, providing insights into the potential for regrowth and overall gum health. Understanding the factors that contribute to gum recession, from genetics to…
Internal Jugular Vein Anatomy A Deep Dive
Internal jugular vein anatomy sets the stage for this enthralling narrative, offering readers a glimpse into the intricate network of vessels that power our bodies. We’ll explore the vein’s position amidst other neck structures, examining its crucial role in venous return and its significance in various clinical scenarios. From anatomical landmarks to surgical considerations, this…
Surgery Not Needed for Rotator Cuff Tears Alternatives Explored
Surgery not needed for rotator cuff tears is a growing area of interest for those experiencing pain and discomfort in their shoulders. This in-depth exploration delves into the various non-surgical treatment options available, providing a comprehensive overview of how to effectively manage rotator cuff tears without resorting to surgery. From physical therapy and medication to…
Psoriatic Arthritis Differential Diagnosis Explained
Psoriatic arthritis differential diagnosis is crucial for accurate treatment. Understanding the subtle distinctions between PsA and similar conditions like reactive arthritis, lupus, or even osteoarthritis is key to effective management. This guide dives deep into the various facets of diagnosing PsA, exploring its clinical presentation, potential overlaps with other conditions, and the diagnostic tools used…
Tylenol vs Advil for Headache Relief
Tylenol vs Advil for treating a headache is a common question for those seeking pain relief. Both are over-the-counter options, but they differ in their active ingredients and how they work. Understanding these differences can help you choose the best medicine for your headache. This comparison explores the efficacy, side effects, and safety considerations of…
Maximize Dry Eye Treatment A Comprehensive Guide
Maximize dry eye treatment is crucial for achieving optimal comfort and vision. This comprehensive guide explores the multifaceted aspects of dry eye, from understanding its causes and symptoms to maximizing treatment outcomes and embracing emerging therapies. We’ll delve into the science behind dry eye, compare current treatments, and discuss personalized approaches to management. The article…
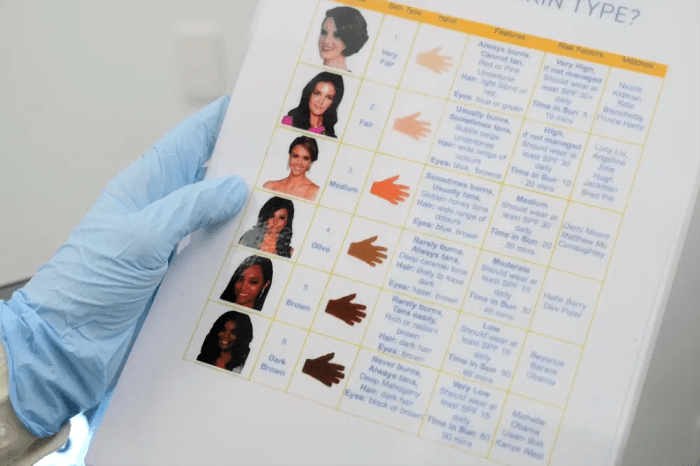
Itchy Moles Skin Cancer Symptom?
Is an itchy mole a symptom of skin cancer? This question is a crucial one for anyone concerned about their skin health. Moles, those common skin markings, can sometimes be a source of worry, especially if they change or become itchy. Understanding the differences between benign and cancerous moles, and recognizing the warning signs, is…