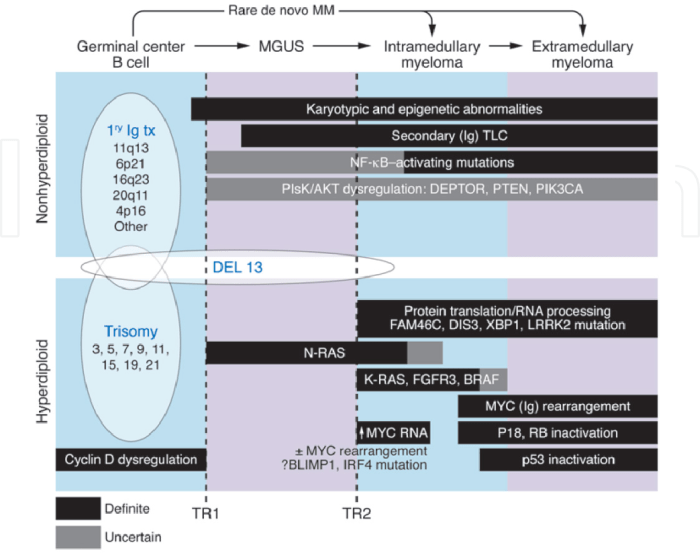
Monoclonal gammopathy of undetermined significance (MGUS) is a condition where a type of protein called a monoclonal immunoglobulin is produced in excess in the blood. While often asymptomatic, MGUS can sometimes progress into more serious conditions like multiple myeloma. Understanding the characteristics, diagnostics, and management strategies for MGUS is crucial for both patients and healthcare…
Author: Carlos Schuster
The History of Surgery Timeline A Journey Through Time
The history of surgery timeline sets the stage for this enthralling narrative, offering readers a glimpse into the evolution of surgical techniques throughout history. From ancient civilizations to modern marvels, this journey explores the incredible advancements, the courageous pioneers, and the constant quest for better healing. We’ll uncover the fascinating stories behind the development of…
The 30 Most Prescribed Drugs in Pediatrics
The 30 most prescribed drugs in pediatrics play a crucial role in treating various childhood illnesses. Understanding the factors influencing these prescriptions, including dosage adjustments specific to children, is essential for optimal patient care. This exploration delves into the selection process, highlighting safety profiles, and examining the potential for drug interactions. We will also discuss…
Anti-Inflammatory Diet for Psoriasis A Guide
Anti inflammatory diet for psoriasis – Anti-inflammatory diet for psoriasis is a powerful approach to managing this chronic skin condition. It’s not just about avoiding certain foods, but about understanding how your diet directly impacts inflammation and your psoriasis symptoms. This comprehensive guide explores the principles, food choices, and practical strategies to create a personalized…
How Does Bird Flu Spread to Humans? A Deep Dive
How does bird flu spread to humans? This critical question demands our attention, as understanding the transmission pathways is crucial for prevention and control. From direct contact with infected birds to contaminated environments, this blog post will explore the multifaceted ways this virus can jump species. We’ll delve into the various risk factors, clinical manifestations,…
Gout in the Fingers Overview and More
Gout in the fingers overview and more: Understanding this painful condition is crucial for effective management. This in-depth look explores the causes, symptoms, and treatment options for gout in the fingers, distinguishing it from other similar conditions. We’ll also delve into risk factors, prevention strategies, and the practical aspects of living with gout in the…
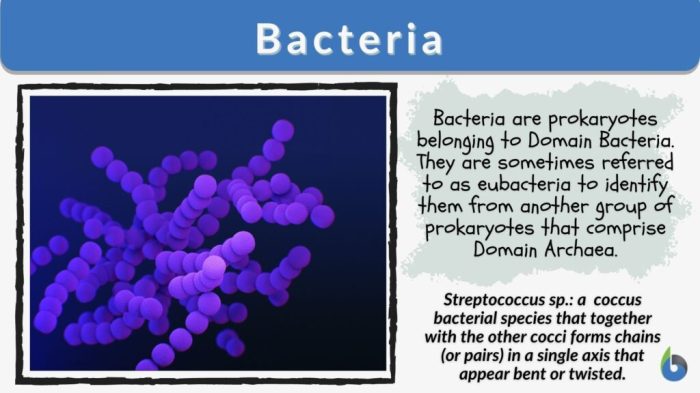
Bacterial Vaginosis Keeps Coming Back Understanding Recurrence
Bacterial vaginosis keeps coming back, frustrating many women. This recurring infection can be challenging to manage, impacting quality of life. This blog post delves into the reasons behind these recurring episodes, exploring everything from lifestyle factors to potential underlying health conditions. We’ll also look at diagnostic considerations, treatment strategies, and preventive measures you can take…
Exercises for Arthritic Knees A Guide
Exercises for arthritic knees are crucial for managing pain and improving mobility. This guide provides a comprehensive overview of various exercises, tailored to different levels of knee arthritis severity. We’ll explore different types of exercises, safety precautions, and how to design a personalized program to help you stay active and comfortable. From strengthening to flexibility,…
L-Theanine and Magnesium A Powerful Duo
L theanine and magnesium – L-theanine and magnesium, a powerful duo for well-being. This exploration dives into the individual properties of each, delving into their potential synergistic effects when combined. We’ll uncover the science behind their interaction, exploring their impact on stress, cognition, and sleep. Expect a detailed look at dosage ranges, potential benefits, and…
How to Eat During an IBD Flare-Up
How to eat during an ibd flare up – How to eat during an IBD flare-up is crucial for managing symptoms and promoting healing. This guide provides a comprehensive overview of dietary strategies, from understanding the disease to specific recommendations and safe food preparation. It delves into the nuances of IBD flare-ups, highlighting the importance…