Why am I so tired after my cardiac ablation? This question plagues many patients who undergo this procedure. The recovery process can be surprisingly complex, with a range of factors contributing to post-procedure fatigue. From the physiological effects of the ablation itself to pre-existing health conditions and lifestyle choices, understanding the reasons behind this fatigue…
Author: Carlos Schuster
Chemotherapy for Metastatic Breast Cancer A Deep Dive
Is chemotherapy used to treat metastatic breast cancer? This in-depth exploration delves into the role of chemotherapy in managing this aggressive form of breast cancer. We’ll uncover the complexities of metastatic breast cancer, examining its progression from localized disease, and explore the specific chemotherapy regimens employed to combat the spread of cancer cells. Understanding the…
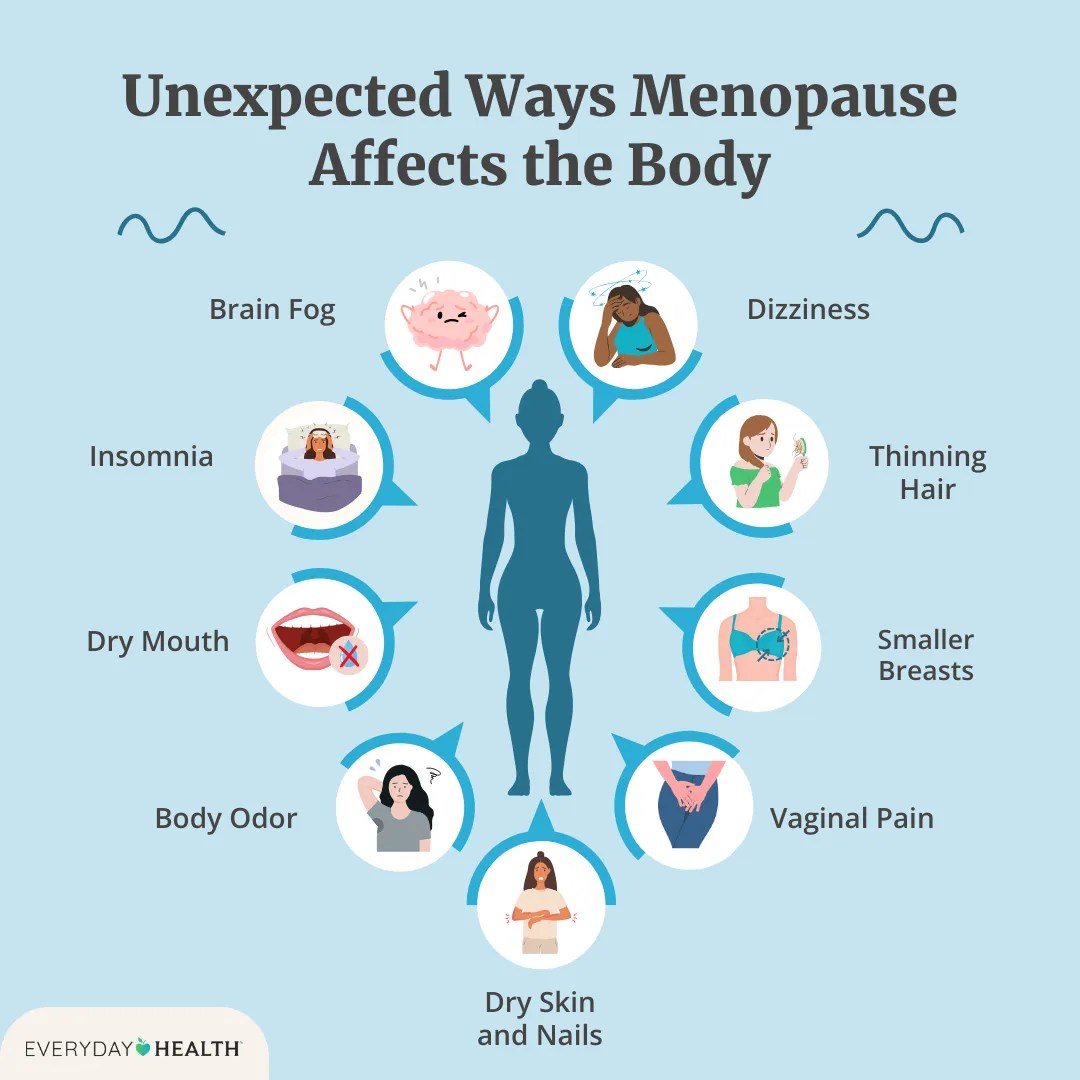
Menopause and Joint Pain Understanding the Connection
Menopause and joint pain often go hand-in-hand, creating a complex interplay of symptoms and underlying mechanisms. This exploration delves into the physiological changes during menopause that can affect joints, examining the types of pain experienced, and exploring the connection between hormonal fluctuations and discomfort. We’ll also look at diagnosis, treatment strategies, and crucial lifestyle recommendations…
Weight Loss Plateau Ozempic Wegovy Strategies & Solutions
Weight loss plateau Ozempic Wegovy is a common challenge for those using these medications. This detailed guide explores the reasons behind these plateaus, examining the complex interplay between medication, lifestyle, and potential metabolic adaptations. We’ll delve into the mechanisms of Ozempic and Wegovy, comparing their profiles and potential side effects, while addressing the unique considerations…
Perils of Using the Internet to Self-Diagnose
Perils of using the internet to self diagnose: Navigating the vast ocean of online health information can be tempting, but it’s crucial to understand the potential pitfalls. From misinterpreting symptoms to delaying professional care, the consequences of self-diagnosing online can be far-reaching and potentially harmful. This exploration delves into the risks associated with seeking medical…
Boutique Medicine Concierge Doctor Practices Explained
What is boutique medicine a concierge doctor practice – What is boutique medicine, a concierge doctor practice? It’s a personalized healthcare model that offers a unique experience compared to traditional practices. Patients gain access to a dedicated doctor with extended appointment times, after-hours support, and tailored care plans. This approach emphasizes a strong doctor-patient relationship,…
Should You Put Mouthwash in Your Water Flosser?
Should you put mouthwash in your water flosser? This intriguing question sparks a fascinating debate about enhancing oral hygiene. Adding mouthwash to your water flosser might seem like a logical next step, but is it actually beneficial, or could it introduce unwanted complications? Let’s dive deep into the potential benefits, risks, and practical considerations of…
Opill OTC Available for Retail A Deep Dive
Opill OTC available for retail is a significant development with implications for consumer access and healthcare. This post explores the legal frameworks, pharmacy practices, consumer demand, supply chain management, and marketing strategies surrounding the retail availability of these medications. We’ll examine the differences in regulations across various regions and how these factors impact the retail…
Pediatric Migraines Symptoms & Treatment
Pediatric migraines symptoms and treatment methods is a crucial topic for parents and healthcare professionals alike. Understanding the various symptoms, diagnostic processes, and effective treatment options is key to managing these debilitating headaches in children. This exploration dives deep into the complexities of pediatric migraines, offering a comprehensive overview for a better understanding. This article…
Spring Cleanings Dirty Dozen
The 10 dirtiest places to hit during spring cleaning are about to be revealed! This deep dive into the most neglected corners of your home will equip you with the knowledge and strategies to tackle even the toughest grime. From the refrigerator’s hidden nooks to the bathroom’s stubborn stains, we’ll explore the science behind dirt…