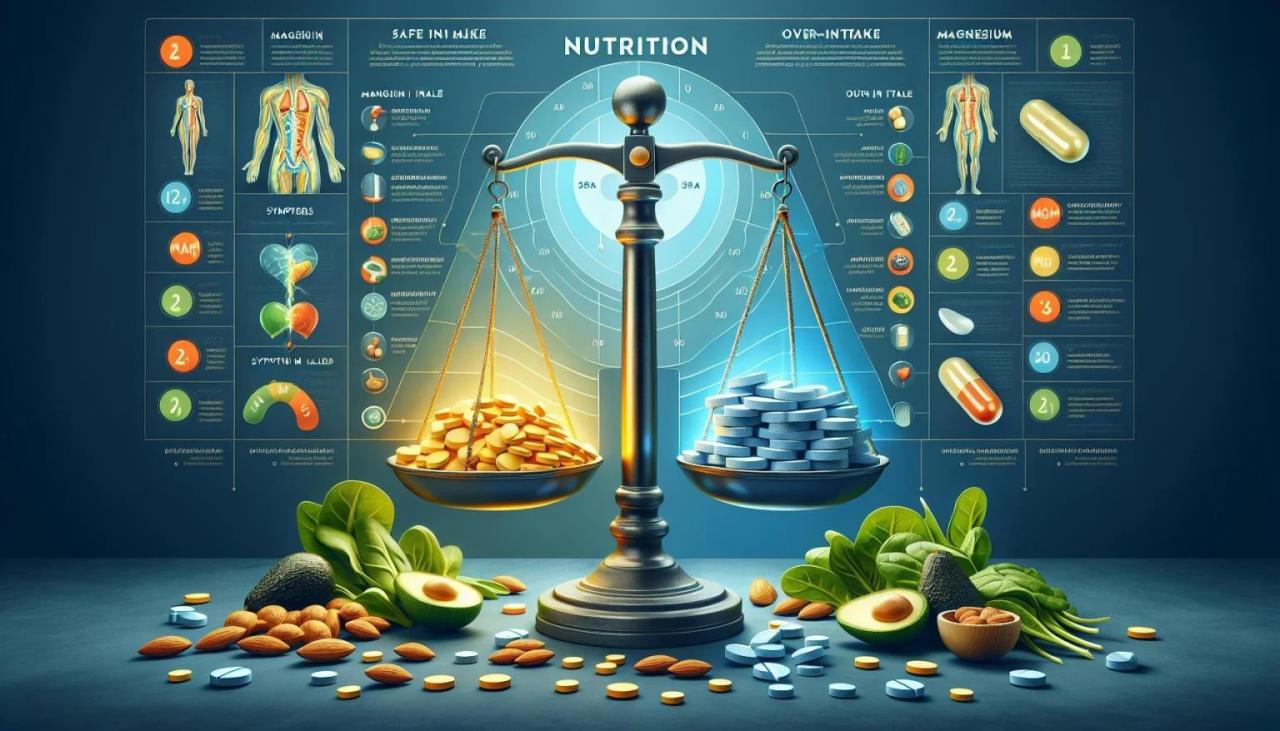
Can you take too much magnesium? This question delves into the potential dangers of excessive magnesium intake, exploring the symptoms, causes, and management strategies. We’ll cover everything from the subtle signs of overdose to medical interventions and preventive measures, empowering you with knowledge to maintain healthy magnesium levels. Understanding magnesium’s role in the body is…
Author: Albert Quigley
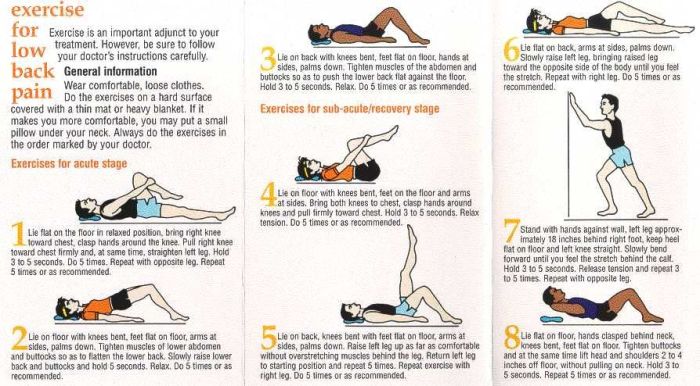
Physical Therapy and Exercises for Low Back Pain A Comprehensive Guide
Physical therapy and exercises for low back pain offer a powerful approach to managing and alleviating discomfort. This guide delves into the various types of exercises, tailored programs, and crucial lifestyle considerations to effectively address low back pain. We’ll explore everything from understanding the different types of back pain to creating a personalized home exercise…
Do I Need a Knee Brace? A Comprehensive Guide
Do I need a knee brace? This comprehensive guide delves into the complexities of knee pain and when a brace might be the right solution. We’ll explore various types of knee pain, potential causes, and the importance of consulting a healthcare professional. Beyond simply answering the question, we’ll equip you with the knowledge to make…
How to Stop an Eye Twitch A Complete Guide
How to stop an eye twitch? This comprehensive guide dives into the fascinating world of involuntary eye twitches, exploring everything from the underlying physiology to effective home remedies and when professional help is crucial. We’ll uncover the common causes, potential triggers, and practical strategies for managing and preventing these often-annoying spasms. Understanding the different types…
Six Signs of a Heart Attack a Month Before
Six signs of a heart attack a month before can be subtle, often appearing as common physical or emotional changes. Understanding these potential warning signals is crucial for early detection and intervention. This exploration delves into the nuances of premonitory signs, examining how lifestyle factors and underlying health conditions might contribute to their emergence. We’ll…
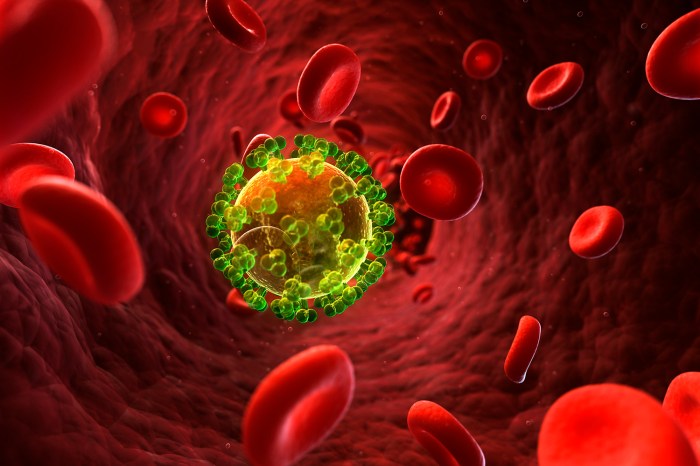
HIV in Black Men Increased Risk, Facts, Testing
HIV in black men increased risk facts testing resources is crucial for understanding the complexities surrounding this health issue. This exploration delves into the historical context, examining social and economic factors that contribute to higher risk. We’ll look at healthcare access disparities and the importance of culturally competent care. Further, we’ll analyze key risk factors,…
Understanding Thyroid Fluctuations
When your thyroid levels are fluctuating, your body can experience a whirlwind of changes. This insightful exploration delves into the complexities of thyroid level variations, covering everything from the underlying causes and symptoms to the crucial diagnostic process, treatment options, and long-term management strategies. We’ll also examine patient experiences, case studies, and visual representations of…
Eat Before or After Workout Timing is Key
Eat before or after workout sets the stage for optimal performance and recovery. This in-depth exploration delves into the science behind when to fuel your body for peak results, considering factors like workout type, individual needs, and even dietary restrictions. We’ll unpack the impact of different macronutrients, pre- and post-workout snack ideas, and how to…
Foods That Make You Feel Full Your Guide to Satiety
Foods that make you feel full are crucial for managing your appetite and achieving a healthy weight. This guide dives deep into the science behind satiety, exploring the types of foods that promote fullness, the mechanisms involved, and practical strategies for incorporating them into your diet. We’ll uncover how different foods, from high-fiber options to…
Vacuum Therapy Pros and Cons A Deep Dive
Vacuum therapy pros and cons are a fascinating subject, exploring a treatment method that’s gaining traction in various health circles. From its historical roots to modern applications, this treatment involves using suction to stimulate the body. Different types of vacuum therapy, like cupping and suction therapy, have various purported benefits and potential risks. This exploration…