Naloxone vs naltrexone similarities and differences are crucial for understanding their distinct roles in opioid overdose management and long-term addiction treatment. These medications, while both working to counteract opioid effects, have key distinctions in their mechanisms of action, duration of effects, and clinical applications. This exploration dives into the nuances of these life-saving drugs, highlighting…
Author: Albert Quigley
Vitamin D Two vs D Three A Deep Dive
Vitamin D two vs D three is a crucial comparison for understanding the different forms of this essential nutrient. Both play vital roles in calcium absorption and bone health, but their sources, absorption rates, and potential benefits differ. This exploration will delve into the chemical structures, dietary sources, and metabolic processes of each, ultimately helping…
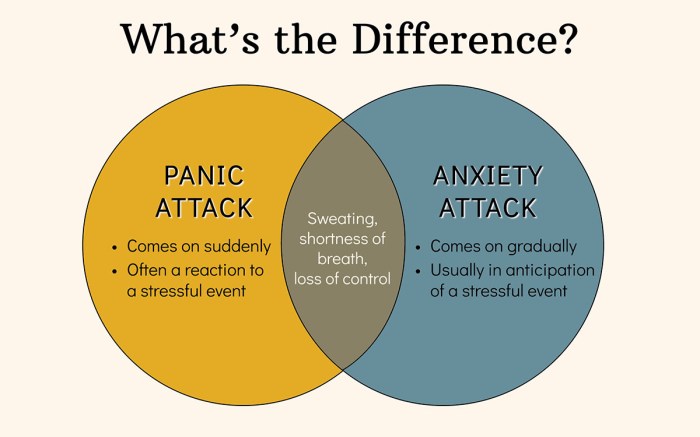
Panic Attack vs Anxiety Attack Understanding the Differences
Panic attack vs anxiety attack: This exploration delves into the nuances of these two closely related yet distinct emotional experiences. Understanding their differences is crucial for effective management and treatment. From the physiological responses to the psychological impact, we’ll unravel the complexities of each, highlighting key similarities and contrasting features. This comprehensive guide aims to…
ADHD in Women Common Signs and Symptoms
ADHD in women common signs and symptoms are often overlooked or misdiagnosed. This in-depth look delves into the unique ways ADHD presents in women, moving beyond the typical checklists and exploring how it manifests in daily life. We’ll uncover the subtle signs and symptoms, highlighting the differences in presentation compared to men, and addressing the…
The Benefits of Evening Primrose Oil A Deep Dive
The benefits of evening primrose oil are multifaceted and fascinating. Derived from the evening primrose plant, this versatile oil boasts a range of potential health advantages, from supporting skin health to potentially influencing hormonal balance and even easing joint discomfort. We’ll explore the various ways this natural remedy might improve your well-being, examining its key…
Beef Tallow vs Seed Oil A Deep Dive
Beef tallow vs seed oil: a crucial comparison for discerning cooks and health-conscious individuals. This exploration delves into the nutritional, culinary, environmental, and economic aspects of these two prevalent cooking oils, revealing their unique characteristics and potential impacts. From their origins to their practical applications, we’ll examine the nuances of each oil, providing a comprehensive…
Raw Cheese and Bird Flu A Deep Dive
Raw cheese and bird flu: a potentially dangerous combination. This post explores the risks associated with consuming raw cheese during a bird flu outbreak, examining how the delicacy can transmit the virus. We’ll also delve into the scientific understanding behind this transmission, food safety regulations, alternative dairy options, and crucial public health messaging. Understanding the…
Mosquito Bite Preferences Why Some Get Bit More
Reason mosquitoes bite some people more others is a fascinating mystery. We’ve all experienced the frustrating disparity – one person seemingly immune, another a mosquito magnet. This exploration dives into the science behind these preferences, uncovering the complex interplay of biological factors, human characteristics, and environmental influences that dictate who gets bitten and why. From…
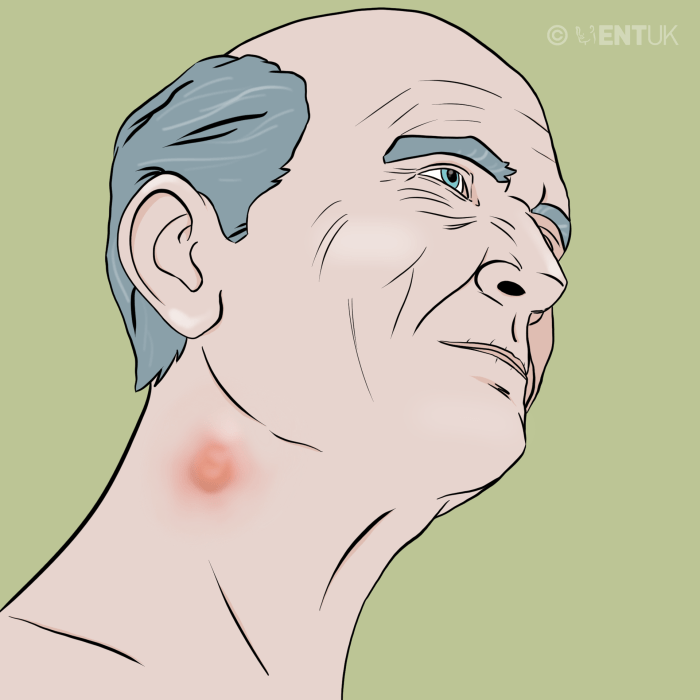
Lump Under Skin Causes & When to Worry
Lump under skin causes and when to worry about it is a crucial topic for anyone experiencing such a concern. Skin lumps can arise from a variety of factors, ranging from harmless cysts to more serious conditions. Understanding the potential causes and knowing when to seek medical attention can be vital for a quick diagnosis…
Can You Live Without Your Pancreas? A Comprehensive Guide
Can you live without your pancreas? This comprehensive guide delves into the fascinating world of pancreatic function, the medical considerations for removal, lifestyle adjustments, long-term effects, and ethical considerations. We’ll explore the vital role the pancreas plays in digestion and hormone regulation, examining the necessary dietary changes and medical procedures involved in managing life without…