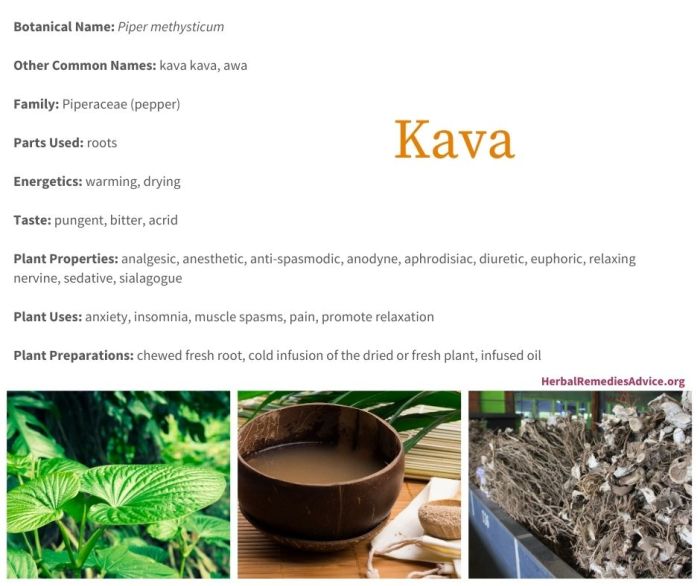
Kava uses risks and more are a complex topic, and this exploration dives deep into the world of kava, from its traditional uses to potential modern applications, alongside the important risks associated with its consumption. We’ll look at the rich history and cultural significance of kava, and examine the chemical compounds that make it unique….
Author: Albert Quigley
How to Interpret RAST Test Results
How to interpret the RAST test results is crucial for accurate allergy diagnosis. This comprehensive guide dives into the intricacies of understanding these results, from the different components measured to the significance of positive and negative findings. We’ll explore the vital connection between RAST results, patient history, symptoms, and the limitations of the test itself….
Foods to Avoid with UTI A Dietary Guide
Foods to avoid with UTI can significantly impact your recovery. Understanding which foods might worsen your symptoms is key to managing this common infection effectively. This guide explores the relationship between diet and UTIs, providing insights into specific foods to limit or avoid, along with strategies for hydration and balanced meal plans. We’ll delve into…
Spending the First Night Using CPAP
Spending the first night using CPAP sets the stage for a transformative journey toward better sleep. This experience, while potentially daunting, can be smoother than you imagine with the right preparation. We’ll explore everything from essential equipment and setup to troubleshooting common issues, and ultimately, how your first night with CPAP affects your overall sleep…
Enriching Lives Activities for Nursing Homes and Assisted Living
Activities for nursing homes and assisted living are crucial for resident well-being. They offer opportunities for engagement, socialization, and enjoyment, fostering a positive and stimulating environment. This exploration dives deep into various activity types, from passive relaxation to active participation, catering to diverse needs and preferences. From memory care to general residents, we’ll discuss adapting…
The Health Benefits of Boswellia A Deep Dive
The health benefits of boswellia, a resinous extract from the Boswellia tree, have captivated herbalists and health enthusiasts for centuries. This ancient remedy, often used in traditional medicine, boasts a range of potential applications, from easing arthritis pain to supporting digestive health. We’ll explore the science behind this intriguing plant, delving into its anti-inflammatory properties,…
Benefits of Essential Oils A Deep Dive
Benefits of essential oils are gaining popularity, and this comprehensive guide delves into the fascinating world of these natural extracts. From their ancient uses to modern scientific research, we’ll explore their origins, properties, potential benefits, and crucial safety considerations. Understanding the diverse ways essential oils can impact our well-being requires a nuanced approach, so let’s…
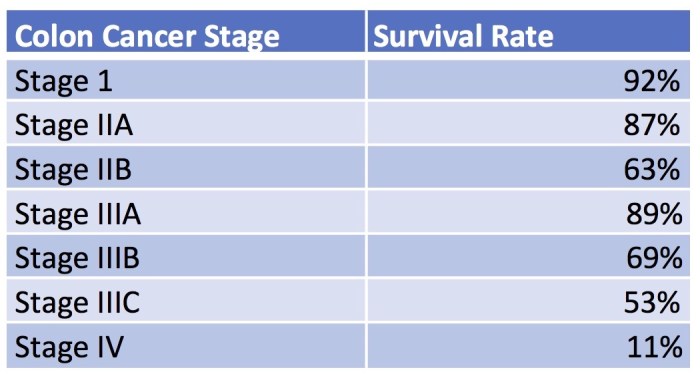
Rectal Cancer Survival Rates A Comprehensive Guide
Rectal cancer survival rates are a critical factor for patients and their families. This blog post delves into the intricacies of survival, examining factors like stage at diagnosis, treatment approaches, and even geographical influences. We’ll explore the 5-year survival rates across different stages, discuss the impact of treatment options, and analyze recent advancements in treatment….
Why There Will Never Be a Cold Vaccine
Why there will never be a vaccine for the common cold? This exploration delves into the intricate nature of the rhinovirus, the immune system’s response, and the significant challenges in vaccine development. The complexity of viral evolution and the sheer genetic diversity of cold viruses make a preventative vaccine a near-impossible feat. The common cold,…
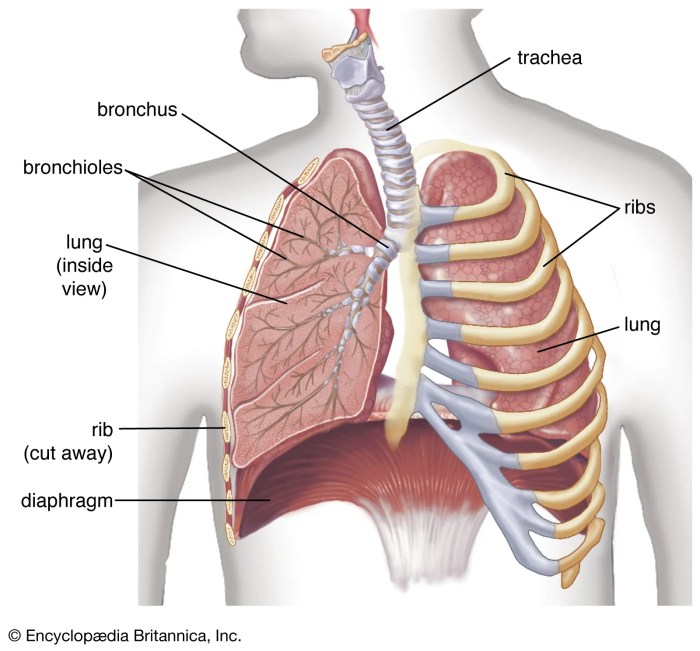
Maintenance Therapy for Lung Cancer A Deep Dive
Maintenance therapy for lung cancer is a crucial aspect of treatment, aiming to prevent the cancer from returning or spreading. It’s a strategy that seeks to keep the cancer at bay after initial treatment, often by targeting specific mechanisms that drive the disease. This in-depth look explores the various types, mechanisms, patient considerations, protocols, side…