Ask an expert how does asthma impact daily life? This exploration delves into the multifaceted ways asthma affects everyday routines, from physical exertion and sleep to social interactions and mental well-being. We’ll examine how varying asthma severities influence daily life, and uncover practical strategies for managing symptoms and challenges. From the subtle impact on sleep…
Author: Albert Quigley
Potential Pregnancy Complications with PCOS A Guide
Potential pregnancy complications with PCOS are a significant concern for women facing this condition. PCOS, or Polycystic Ovary Syndrome, often disrupts the natural hormonal balance crucial for conception and a healthy pregnancy. This comprehensive guide delves into the various potential issues, from the increased risk of gestational diabetes to the possible impact on placental function….
5 Components of Fitness Your Complete Guide
5 components of fitness sets the stage for a deep dive into the essential elements of a healthy lifestyle. This isn’t just about looking good; it’s about feeling amazing and achieving peak physical performance. From understanding the basics to crafting personalized workout routines, we’ll explore each component in detail, offering practical advice and insights. This…
Why Do We Have Wisdom Teeth? A Deep Dive
Why do we have wisdom teeth? This question has puzzled scientists and dental professionals for generations. These seemingly vestigial molars, erupting often in our late teens or twenties, have a complex evolutionary history. They weren’t always a source of pain and crowding, but rather, played a crucial role in our ancestors’ survival. This blog post…
Left Side Neck and Shoulder Pain Understanding the Causes
Neck and shoulder pain on left side – Neck and shoulder pain on the left side can be debilitating, impacting daily life. This in-depth exploration delves into the potential causes, symptoms, diagnosis, treatment, and prevention strategies for this common issue. We’ll uncover everything from musculoskeletal problems to neurological conditions, and discuss how lifestyle factors can…
How Long Does a Flu Shot Last? Your Guide
How long does a flu shot last? This crucial question affects everyone’s decision to get vaccinated. Understanding the duration of protection offered by flu shots is key to making informed choices about your health. Different factors, like the specific flu strain, your immune system, and even underlying health conditions, all play a role in how…
The Benefits of Hawthorn A Comprehensive Guide
The benefits of hawthorn, a versatile plant with a rich history, are now being explored more deeply than ever. From its traditional use in various cultures to modern scientific research, hawthorn’s potential for promoting cardiovascular health and well-being is truly remarkable. This comprehensive guide delves into the different aspects of hawthorn, examining its nutritional profile,…
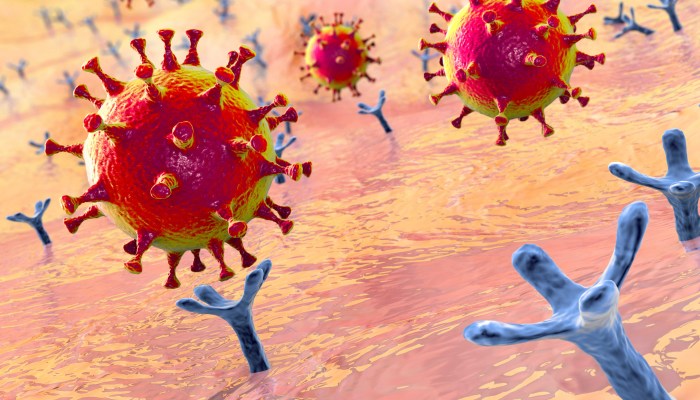
COVID-19 Coronavirus Vaccine A Comprehensive Look
Covid 19 coronavirus vaccine – COVID-19 coronavirus vaccine development has been a global race against time. From initial trials to widespread distribution, this journey has presented unprecedented challenges and triumphs. We’ll explore the scientific breakthroughs, logistical hurdles, and ethical considerations surrounding the COVID-19 vaccine rollout, including its effectiveness, impact, and the future of vaccine research….
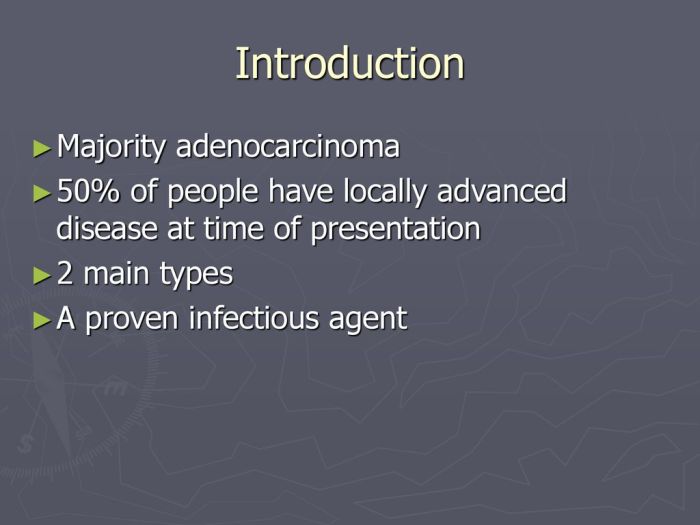
Metastatic Adenocarcinoma Overview and More
Metastatic adenocarcinoma overview and more delves into the complexities of this aggressive cancer. We’ll explore its defining characteristics, the often-devastating journey of diagnosis and treatment, and the vital support systems available for patients and families. From understanding the different stages to examining treatment options and prognosis, this comprehensive guide aims to equip readers with a…
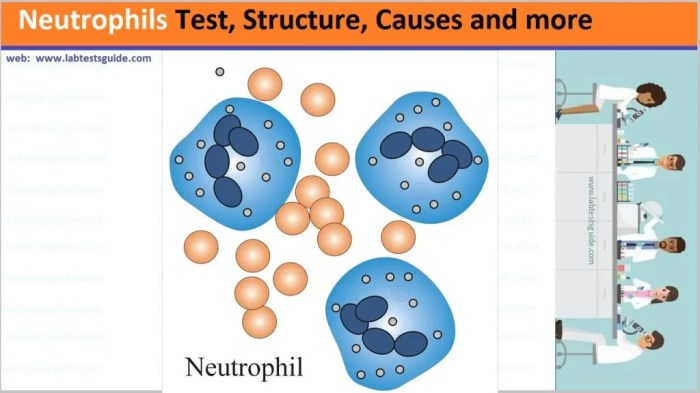
What are Neutrophils P2 A Deep Dive
What are neutrophils p2? This exploration delves into the crucial role of neutrophils, a type of white blood cell, within the context of P2. We’ll uncover their significance in the immune system, examining their structure, function, and behavior in a P2 environment. From the intricacies of their normal function to their response in P2 conditions,…