Do ADHD symptoms differ in boys and girls? This question sparks a crucial discussion about how the condition manifests differently across genders. Early research often presented a skewed picture, influenced by societal expectations and diagnostic biases. Understanding the nuances of how ADHD presents in both boys and girls is vital for accurate diagnoses and effective…
Author: Albert Quigley
Does Iron Cause Constipation? A Deep Dive
Does iron cause constipation? This exploration delves into the complex relationship between iron intake and digestive health. Understanding the role of iron in the body, the various forms of iron, and their absorption processes is crucial to comprehending this connection. We’ll also examine how individual differences, diet, and medications might influence this relationship. Iron, an…
How to Become an Endocrinologist A Comprehensive Guide
How to become an endocrinologist? This in-depth guide will equip you with the knowledge and steps needed to embark on this rewarding medical career. From the initial educational requirements to specialized training, professional development, and crucial skills, we’ll cover every aspect of this fascinating journey. Prepare to delve into the intricacies of this field and…
Signs of Depression in Men Hidden Struggles
Signs of depression in men often manifest differently than in women, leading to delayed recognition and treatment. Societal pressures and cultural norms frequently discourage men from seeking help, masking the underlying issue. This in-depth exploration delves into the various signs, from emotional and behavioral changes to subtle physical indicators. We’ll also discuss the challenges men…
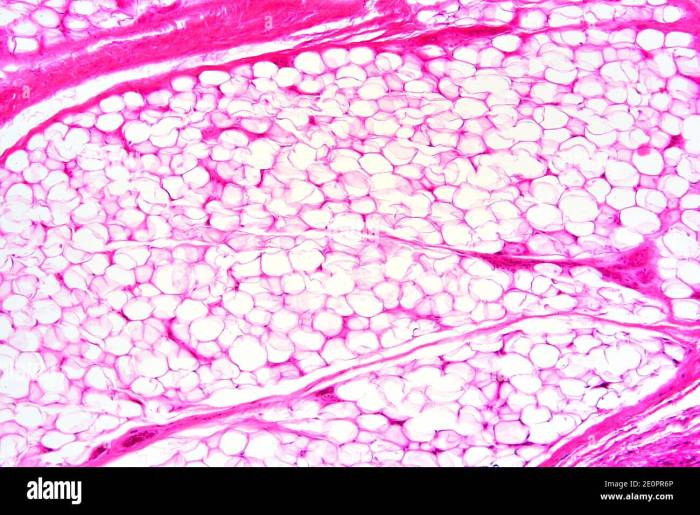
What is Adipose Tissue A Deep Dive
What is adipose tissue? It’s more than just fat; it’s a complex and crucial tissue in the human body, playing a vital role in energy storage, hormone regulation, and overall health. This exploration delves into the fascinating world of white, brown, and beige adipose tissue, uncovering their distinct characteristics, functions, and relationship to various health…
What is Barretts Esophagus A Deep Dive
What is barretts esophagus – What is Barrett’s esophagus? This condition occurs when the lining of your esophagus, the tube connecting your mouth and stomach, changes. It’s a significant health concern that can lead to serious complications if not properly managed. This in-depth exploration will delve into the causes, symptoms, diagnosis, complications, treatment options, and…
Is Coconut a Tree Nut? Unveiling the Truth
Is coconut a tree nut? This question sparks curiosity and debate, especially among those with allergies or a keen interest in botany. Unraveling the truth requires a deep dive into botanical classifications, nutritional comparisons, and historical contexts. This exploration will demystify the differences between coconuts and true tree nuts. We’ll dissect the scientific characteristics that…
How to Get Rid of Peeling Skin A Comprehensive Guide
How to get rid of peeling skin? This comprehensive guide delves into the various causes, home remedies, medical treatments, and preventive measures for this common skin issue. From understanding the different types of peeling to exploring dietary considerations and tailored skincare routines, we’ll cover everything you need to know to restore healthy, smooth skin. We’ll…
How Autoimmune Hepatitis Is Diagnosed A Comprehensive Guide
How autoimmune hepatitis is diagnosed is a crucial step in ensuring timely and effective treatment. This intricate process involves a multifaceted approach, combining various tests and assessments to pinpoint the presence and severity of this condition. Understanding the diagnostic journey is vital for both patients and healthcare professionals alike, and this guide delves into the…
Favorite Leg Strengthening Exercises Your Ultimate Guide
Favorite leg strengthening exercises are crucial for overall fitness and well-being. Strong legs contribute to improved posture, balance, and athletic performance. This comprehensive guide explores the most effective exercises, proper form, safety precautions, and even nutrition tips to maximize your leg strength training journey. We’ll delve into the science behind these exercises, examining the specific…