Arthritis in back treatment is a crucial topic for understanding and managing spinal pain. This guide delves into the various types of back arthritis, exploring their causes, symptoms, and treatment options. We’ll cover everything from diagnosis and evaluation to lifestyle management and potential complications, offering a comprehensive perspective on this complex health issue.
Different types of arthritis, such as osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis, affect the spine in unique ways. Understanding these differences is essential for tailored treatment strategies. This article provides a thorough analysis of each type, comparing their causes, symptoms, and typical approaches to management. From non-pharmacological therapies to surgical interventions, we’ll examine all available options.
Introduction to Back Arthritis
Back arthritis encompasses a range of conditions affecting the spine, causing pain, stiffness, and reduced mobility. These conditions can impact daily life significantly, impacting everything from simple movements to more complex activities. Understanding the different types, symptoms, and potential treatments is crucial for effective management.
Types of Back Arthritis
Various forms of arthritis can affect the spine. These conditions stem from different underlying causes and manifest with varying symptoms. Knowing the specifics of each type aids in accurate diagnosis and tailored treatment plans.
Osteoarthritis
Osteoarthritis, a degenerative joint disease, is a common cause of back pain. It results from the breakdown of cartilage, the protective tissue cushioning joints. As cartilage wears away, bones rub against each other, leading to pain, stiffness, and swelling. This often occurs with age or due to repetitive stress. The gradual deterioration can manifest in the facet joints of the spine, leading to significant discomfort.
Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease where the body’s immune system mistakenly attacks its own tissues, including the joints. In the spine, this can lead to inflammation and pain, potentially causing deformities. This inflammatory condition differs from the wear-and-tear nature of osteoarthritis. The chronic inflammation can result in a variety of symptoms, including swelling, stiffness, and fatigue.
Ankylosing Spondylitis
Ankylosing spondylitis is a type of arthritis primarily affecting the spine and sacroiliac joints. It’s characterized by inflammation of the spine, leading to stiffness and fusion (ossification) of the vertebrae over time. This can cause significant limitations in spinal movement and posture. Early diagnosis and treatment are essential to manage the progression of this condition.
Comparison of Back Arthritis Types
| Type of Arthritis | Cause | Symptoms | Treatments |
|---|---|---|---|
| Osteoarthritis | Degeneration of cartilage; age, repetitive stress | Joint pain, stiffness, swelling, limited range of motion, often worse after activity | Pain relievers, physical therapy, exercise, assistive devices |
| Rheumatoid Arthritis | Autoimmune response | Inflammation, pain, stiffness, swelling, fatigue, potential joint deformities | Disease-modifying antirheumatic drugs (DMARDs), corticosteroids, physical therapy |
| Ankylosing Spondylitis | Unknown, likely genetic and environmental factors | Chronic inflammation, back stiffness, pain, reduced spinal flexibility, morning stiffness | Nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, exercise, potential surgery |
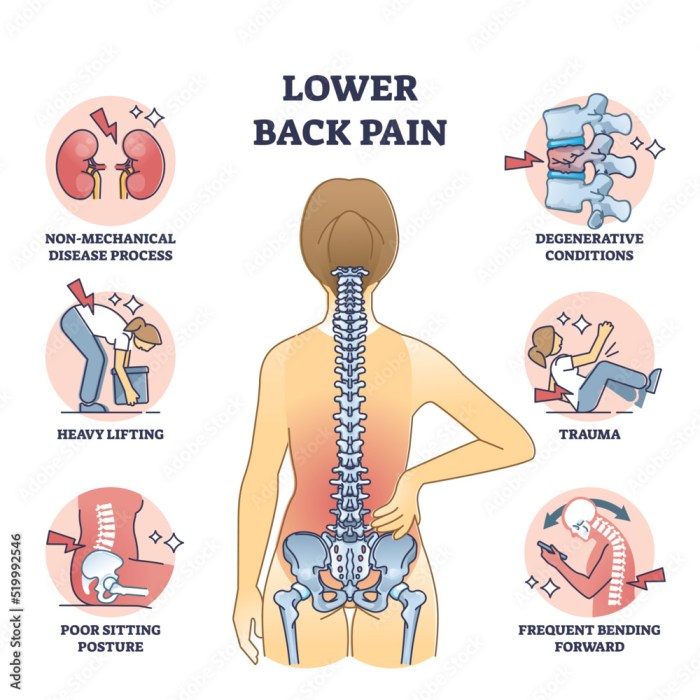
Causes and Risk Factors
Understanding the causes and risk factors for back arthritis is crucial for developing effective prevention and treatment strategies. Back arthritis isn’t a single disease, but rather a group of conditions affecting the joints and surrounding tissues in the spine. Identifying the underlying mechanisms and contributing factors allows for personalized approaches to managing the condition.The development of back arthritis is often a complex interplay of genetic predisposition, lifestyle choices, and environmental influences.
Inflammation plays a pivotal role in the progression of the disease, leading to pain, stiffness, and potential structural damage to the spine. Understanding these elements helps individuals make informed decisions about their health and well-being.
Underlying Mechanisms
Several mechanisms contribute to the development of back arthritis. Degenerative processes, such as osteoarthritis, can affect the cartilage and other tissues within the spine, leading to inflammation and pain. Autoimmune responses, where the body’s immune system mistakenly attacks healthy tissues, can also cause back arthritis, as seen in conditions like ankylosing spondylitis. Trauma or injury to the spine can initiate inflammatory processes and contribute to the development of arthritis later in life.
Risk Factors
Various factors can increase an individual’s risk of developing back arthritis. Age is a significant factor, as the risk often increases with advancing years due to the natural wear and tear on joints. Genetic predisposition plays a role; individuals with a family history of back arthritis are at higher risk. Lifestyle factors, including obesity, smoking, and a sedentary lifestyle, can also contribute to the development of back arthritis by increasing stress on the spine and potentially impacting the immune system.
Specific Conditions
Certain conditions can predispose individuals to back arthritis. Osteoarthritis, characterized by the breakdown of cartilage, is a common cause of back pain and can affect the spine, leading to degenerative changes. Rheumatoid arthritis, an autoimmune disease, can also cause inflammation in the spine. Ankylosing spondylitis, a type of inflammatory arthritis, primarily affects the spine and can cause stiffness and fusion of the vertebrae.
Infectious diseases, while less common, can also cause back arthritis through inflammation.
Role of Inflammation
Inflammation is a crucial component in the progression of back arthritis. It leads to the release of chemicals that can damage cartilage and other tissues, causing pain, stiffness, and potential structural changes in the spine. Chronic inflammation can accelerate the progression of the disease, making it more difficult to manage. Understanding the inflammatory processes involved in back arthritis is vital for developing targeted treatments to reduce inflammation and mitigate its harmful effects.
Risk Factor Table
| Risk Factor | Potential Impact |
|---|---|
| Age | Increased wear and tear on joints, potentially leading to cartilage breakdown and inflammation. |
| Genetics | Inherited predisposition to certain types of back arthritis, such as ankylosing spondylitis. |
| Obesity | Increased stress on the spine, potentially leading to joint damage and inflammation. |
| Smoking | Potential exacerbation of inflammation, hindering healing and potentially worsening the condition. |
| Sedentary Lifestyle | Reduced joint mobility, potentially increasing the risk of stiffness and pain. |
| Previous Spinal Injuries | Increased susceptibility to back arthritis due to pre-existing damage or instability. |
Diagnosis and Evaluation
Pinpointing the specific type of back arthritis and its severity is crucial for effective treatment. Accurate diagnosis relies on a thorough evaluation, combining patient history, physical examination, imaging studies, and potentially blood tests. This multi-faceted approach helps healthcare professionals understand the underlying cause and tailor a treatment plan to individual needs.The diagnostic process for back arthritis involves a systematic approach, beginning with a detailed patient history and physical examination.
These initial steps provide essential clues about the nature and extent of the condition, guiding subsequent investigations. Imaging techniques play a vital role in visualizing the affected areas, while blood tests can offer additional insights into potential systemic factors contributing to the arthritis.
Medical History and Physical Examination
A comprehensive medical history is fundamental to diagnosing back arthritis. Information about the onset, duration, location, and characteristics of pain, as well as any associated symptoms (such as stiffness, swelling, or numbness), are critical for the clinician to assess. Factors like past injuries, surgeries, family history of arthritis, and lifestyle habits (such as occupation and exercise routine) also contribute to the diagnostic puzzle.
The physical examination complements the history, focusing on range of motion, tenderness, and any visible signs of inflammation or deformity. This examination helps in identifying specific areas of concern and assessing the overall functional capacity of the patient.
Imaging Techniques
Imaging studies, such as X-rays, CT scans, and MRIs, are often employed to visualize the structures of the spine and surrounding tissues. X-rays provide basic views of bone structure, allowing identification of potential fractures, narrowing of joint spaces, or bony overgrowths. CT scans offer cross-sectional images, providing detailed views of the bone structure and soft tissues, while MRIs offer detailed images of soft tissues, including cartilage, ligaments, and tendons.
MRIs are particularly useful for identifying subtle inflammation or damage to soft tissues that might be missed by other imaging techniques. For example, an MRI might reveal a herniated disc in the spine, which could be contributing to back pain, even if X-rays appear normal.
Blood Tests
Blood tests can be valuable in evaluating the presence of systemic inflammatory markers, which can sometimes indicate underlying conditions that may contribute to back pain. These tests can measure markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are elevated in inflammatory conditions. For instance, elevated levels of these markers might suggest an autoimmune condition that is causing arthritis in the back.
It’s important to note that elevated levels do not definitively diagnose back arthritis, but they can provide valuable clues in conjunction with other diagnostic methods.
Diagnostic Flowchart
Patient presents with back pain
-----------------------------
| |
| Medical History |
| & Physical Exam |
| |
|_________________|
| |
| Suspected Arthritis |
|_________________|
| |
| Imaging Studies (X-ray, MRI) |
| |
|_________________|
| |
| Blood Tests (ESR, CRP) |
| |
|_________________|
| |
| Diagnosis Confirmed or |
| Further Evaluation Needed |
|_________________|
| ...
(Possible further tests or specialist referral) |
|_______________________________________________________|
Treatment Options

Managing back arthritis requires a multifaceted approach tailored to the individual’s specific needs and condition. A combination of therapies, from non-pharmacological methods to surgical interventions, often proves most effective in alleviating pain, improving function, and slowing disease progression.
Finding the right balance among these options is crucial for long-term well-being.
Non-Pharmacological Therapies
These approaches focus on managing pain and improving function without relying on medication. They are often a first-line strategy, as they carry fewer risks compared to pharmacological treatments.
Effective non-pharmacological therapies include:
- Exercise: Regular, low-impact exercises, such as swimming, walking, or stationary cycling, can strengthen muscles supporting the spine, improve flexibility, and reduce pain. A tailored exercise program developed by a physical therapist is highly beneficial. For example, a patient with osteoarthritis of the lumbar spine might benefit from exercises targeting core strength and improving posture. Consistent exercise routines have been shown to improve pain levels and functional capacity.
- Physical Therapy: Physical therapists provide personalized exercise programs, manual therapies (like massage or mobilization), and guidance on proper posture and body mechanics. They help patients understand how to manage their condition effectively and prevent further injury. For example, a physical therapist might teach a patient with rheumatoid arthritis of the cervical spine how to adjust their posture to reduce stress on the affected area.
This can significantly improve the quality of life and reduce flare-ups.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can temporarily reduce pain and inflammation. Heat promotes blood flow, which can ease muscle tension and pain, while cold reduces inflammation. For instance, a patient with an acute flare-up of ankylosing spondylitis in the thoracic spine could find relief by alternating between heat and ice packs.
- Assistive Devices: Using assistive devices, such as canes, walkers, or back braces, can help support the spine and reduce stress on painful joints. For example, a patient with lumbar spinal stenosis might find a supportive back brace helpful during activities that strain the back.
- Weight Management: Maintaining a healthy weight is crucial for individuals with back arthritis, as excess weight puts extra stress on the spine and joints. For example, a person with psoriatic arthritis who is overweight might experience significant relief from pain and inflammation after losing weight.
Pharmacological Treatments
Medications play a significant role in managing back arthritis symptoms. The choice of medication depends on the specific type of arthritis, its severity, and the patient’s overall health.
Finding the right arthritis in back treatment can be a journey, but understanding potential lifestyle factors can help. For instance, did you know that caffeine intake might play a role in other health conditions, like ADHD? Learning more about caffeine and its impact on your body, particularly in relation to conditions like ADHD, might provide valuable insight into overall wellness, which can be incredibly beneficial when considering arthritis in back treatment options.
Check out this helpful resource on caffeine and ADHD what you should know for a deeper dive. Ultimately, a holistic approach, considering factors like caffeine consumption, is key to managing arthritis in the back.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): These medications, like ibuprofen and naproxen, reduce pain and inflammation. They are often the first-line medication for mild to moderate pain. However, long-term use can have potential side effects, such as stomach ulcers or kidney problems. For instance, a patient with osteoarthritis of the spine might find relief from mild pain using ibuprofen, but this should be discussed with a physician.
- Corticosteroids: These potent anti-inflammatory medications can provide rapid relief from severe pain and inflammation. However, they are typically used for short-term relief due to potential side effects. A patient experiencing a severe flare-up of reactive arthritis in the lumbar spine might receive a short course of corticosteroids to manage the acute pain.
- Disease-Modifying Antirheumatic Drugs (DMARDs): These medications are used for more severe cases of back arthritis, especially those with a progressive inflammatory component. They aim to slow or halt the progression of the disease. For example, a patient with rheumatoid arthritis of the spine would likely be prescribed DMARDs to help control the disease’s progression.
Physical Therapy
Physical therapy is an integral part of back arthritis management. It aims to improve joint mobility, strengthen supporting muscles, and enhance overall function. A tailored physical therapy program can significantly impact a patient’s quality of life. For example, a patient with ankylosing spondylitis would benefit from physical therapy to improve spinal flexibility and reduce stiffness.
Surgical Interventions
Surgical interventions are considered when non-pharmacological and pharmacological treatments fail to provide adequate pain relief or improve function. The type of surgery depends on the specific type of arthritis and the location of the affected area.
- Spinal Fusion: This procedure involves fusing two or more vertebrae to stabilize the spine and reduce pain. It’s typically reserved for severe cases of spinal instability or severe degeneration. A patient with severe spinal stenosis might undergo spinal fusion to improve spinal stability and alleviate symptoms.
- Joint Replacement: In cases of significant joint damage, joint replacement surgery may be an option to alleviate pain and improve mobility. For example, a patient with severe osteoarthritis of the hip joint might consider hip replacement surgery to improve mobility and reduce pain.
Treatment Summary
| Treatment Approach | Benefits | Limitations |
|---|---|---|
| Non-Pharmacological Therapies | Reduced risk of medication side effects, often a first-line approach | May not be effective for severe cases, results may be gradual |
| Pharmacological Treatments (NSAIDs) | Effective pain and inflammation relief | Potential side effects (stomach ulcers, kidney problems), not suitable for all types of arthritis |
| Pharmacological Treatments (Corticosteroids) | Rapid pain relief | Short-term use recommended due to potential side effects |
| Pharmacological Treatments (DMARDs) | Slows disease progression | Can have significant side effects, may not be suitable for all patients |
| Physical Therapy | Improves joint mobility, strengthens muscles, enhances function | May not provide immediate relief, requires commitment and adherence to program |
| Surgical Interventions | Provides long-term pain relief and improved function in severe cases | Involves risks, may not be suitable for all patients |
Lifestyle Management and Self-Care
Managing back arthritis effectively goes beyond medication and treatments. A holistic approach encompassing lifestyle choices plays a crucial role in pain management and improving overall spinal health. This section details key strategies for maintaining a healthy lifestyle to cope with back arthritis.
A proactive approach to managing back arthritis includes understanding the importance of maintaining a healthy lifestyle. This involves not only physical activity but also dietary choices, stress management, and adopting ergonomic principles. By making conscious decisions about these areas, individuals can significantly improve their quality of life and reduce the impact of back arthritis.
Importance of a Healthy Lifestyle
A healthy lifestyle is paramount in managing back arthritis. Maintaining a balanced diet, exercising regularly, and maintaining a healthy weight contribute to reducing inflammation, improving joint function, and boosting overall well-being. These lifestyle choices work synergistically with medical treatments to maximize the effectiveness of care. The body’s overall health and resilience directly impact its ability to manage pain and discomfort.
Strategies for Managing Pain and Discomfort
Effective pain management is a cornerstone of managing back arthritis. Implementing strategies to reduce pain and discomfort is essential for maintaining a good quality of life. These strategies often include using heat or ice packs, employing relaxation techniques, and maintaining good posture. Regularly practicing stress-reducing activities like yoga or meditation can also be helpful in managing pain.
Proper sleep hygiene is crucial, as adequate rest allows the body to recover and heal.
Role of Exercise and Physical Activity
Regular exercise and physical activity are vital for improving spinal health and managing back arthritis symptoms. Low-impact exercises, such as swimming, walking, or cycling, are often recommended. These activities strengthen the muscles that support the spine, improve flexibility, and increase endurance. Strengthening core muscles is particularly important for maintaining spinal stability and reducing pain. Consulting a physical therapist is crucial to develop a safe and effective exercise routine tailored to individual needs.
Significance of Maintaining a Healthy Weight
Maintaining a healthy weight is crucial for managing back arthritis. Excess weight puts extra strain on the spine, increasing pain and inflammation. Losing even a small amount of weight can significantly reduce pressure on the joints and lessen the symptoms of back arthritis. A balanced diet, combined with regular exercise, is key to achieving and maintaining a healthy weight.
Consult a nutritionist or dietitian for personalized dietary advice.
Ergonomic Principles for Preventing and Managing Back Pain
Applying ergonomic principles can prevent and manage back pain associated with back arthritis. Proper posture when sitting, standing, and lifting objects is crucial. Using supportive furniture, such as ergonomic chairs, can reduce strain on the spine. Appropriate lifting techniques should always be employed, lifting objects close to the body and using the legs, not the back. Proper workspace setup, including adequate lighting and appropriate desk height, also plays a crucial role.
Tips for Managing Back Arthritis at Home
Implementing these home strategies can aid in managing back arthritis:
- Regular stretching exercises can improve flexibility and reduce stiffness.
- Using supportive pillows and mattresses can provide better spinal alignment during sleep.
- Employing heat or ice packs can alleviate pain and inflammation.
- Maintaining a consistent sleep schedule helps the body recover and manage pain.
- Practicing relaxation techniques, such as deep breathing exercises or meditation, can reduce stress and muscle tension.
- Avoiding prolonged periods of sitting or standing can reduce strain on the spine.
- Using assistive devices, such as grab bars in the bathroom, can prevent falls and injuries.
- Taking breaks and listening to the body’s signals are crucial for preventing exacerbations.
- Eating a balanced diet rich in anti-inflammatory foods can help manage inflammation.
Potential Complications
Back arthritis, while often manageable, can lead to a range of complications if not properly addressed. These complications can significantly impact a person’s quality of life and overall health. Understanding these potential issues and the importance of early intervention is crucial for proactive management and preventing long-term consequences.
Impact on Mobility and Function
Back arthritis can restrict movement and diminish physical function. Pain, stiffness, and inflammation can make everyday tasks challenging, impacting activities like walking, climbing stairs, and even simple movements like bending over. This can lead to decreased independence and a reduced ability to participate in social activities and work. Individuals may experience limitations in their daily routines, impacting their overall well-being and sense of accomplishment.
Dealing with arthritis in the back can be tough, but understanding potential underlying issues like umbilical cord compression signs and complications might be surprisingly relevant. While seemingly unrelated, some back pain symptoms can stem from issues elsewhere in the body. Focusing on proper diagnosis and treatment tailored to the specific cause of the back pain is key to effective arthritis management.
Development of Spinal Instability
Prolonged inflammation and damage to the spinal structures caused by back arthritis can compromise the stability of the spine. This instability can increase the risk of falls, fractures, and further damage to the spinal tissues. The spine may become more susceptible to misalignment, leading to chronic pain and discomfort. Patients with significant spinal instability may require specialized support or interventions to maintain spinal alignment.
Neurological Complications
In some cases, back arthritis can impinge on nerves within the spinal canal. This compression can result in pain, numbness, tingling, or weakness in the limbs, often following a specific nerve distribution pattern. If left untreated, neurological complications can lead to significant functional impairments and impact the ability to perform everyday tasks. Regular monitoring and prompt medical intervention are vital to prevent severe neurological deficits.
Osteoporosis Risk
Long-term use of certain medications for arthritis, such as corticosteroids, can increase the risk of osteoporosis. Osteoporosis weakens bones, making them more prone to fractures. This risk is particularly relevant for individuals with back arthritis who may already experience reduced bone density due to the disease itself. Careful monitoring of bone health and proactive measures to prevent osteoporosis are crucial.
Chronic Pain and Depression
The persistent pain and limitations associated with back arthritis can lead to chronic pain conditions. This ongoing pain can have a significant impact on mental health, potentially contributing to feelings of anxiety, depression, and reduced quality of life. Chronic pain can significantly impact a person’s mood, relationships, and ability to participate in daily activities. Mental health support and coping strategies are often necessary for individuals experiencing chronic pain.
Dealing with arthritis pain in my back can be tough. Finding relief is key, and sometimes stronger medications like oxycodone are necessary. Knowing how quickly oxycodone takes effect is crucial for managing the pain effectively. For more information on how quickly oxycodone works, check out this helpful resource: using oxycodone how quickly does it work.
Ultimately, though, the best approach to managing back arthritis pain involves a holistic strategy that considers various treatment options.
Surgical Complications
Surgical interventions for back arthritis, while often necessary, can also carry potential complications. These complications can include infection, blood clots, nerve damage, and persistent pain. Careful consideration of the risks and benefits, coupled with thorough pre- and post-operative care, is essential to minimize these complications. A strong support system and adherence to the prescribed post-operative care plan are key to a successful recovery.
Importance of Early Intervention
Early intervention in managing back arthritis complications is crucial. Prompt diagnosis and treatment of the underlying condition can help prevent or mitigate the development of severe complications. Regular check-ups, adherence to prescribed therapies, and lifestyle modifications can significantly impact the progression of the disease and its associated complications. By addressing the issue early, individuals can better maintain their overall health and well-being.
Research and Future Directions
The quest for effective treatments for back arthritis continues to drive significant research efforts. Understanding the complex interplay of genetic predisposition, environmental factors, and lifestyle choices in the development and progression of the disease is crucial. This exploration is paving the way for innovative therapies and a more personalized approach to patient care.
Current Research Focuses
Research in back arthritis is multifaceted, encompassing various approaches to understanding and treating the condition. Scientists are investigating the molecular mechanisms underlying inflammation and cartilage damage, exploring potential biomarkers for early detection, and developing novel therapeutic targets. A key area of focus involves identifying specific genetic markers that can predict an individual’s susceptibility to developing back arthritis, thereby allowing for targeted preventative strategies.
Promising Research Areas
Several promising areas of research hold the potential to revolutionize the treatment of back arthritis. One area is the development of targeted therapies that specifically address the inflammatory pathways implicated in the disease process. Another is the exploration of regenerative medicine approaches, such as stem cell therapy and gene therapy, aiming to repair damaged cartilage and promote tissue regeneration.
Furthermore, research into non-invasive imaging techniques and diagnostic tools is yielding promising results in early detection and disease monitoring.
Advancements in Understanding the Disease Process
Significant advancements in understanding the disease process of back arthritis have led to a more comprehensive understanding of the underlying mechanisms. Researchers are uncovering new pathways involved in the development of inflammation and joint damage. This knowledge is crucial for developing more precise and effective treatments, tailored to the specific needs of individual patients. Detailed analysis of genetic variations associated with back arthritis is also revealing insights into susceptibility and disease progression.
Timeline of Significant Milestones in Back Arthritis Research
- 1990s-2000s: Increased understanding of the role of cytokines and inflammatory mediators in the disease process. Early studies on the genetic basis of back arthritis began to emerge. Development of disease-modifying anti-rheumatic drugs (DMARDs) for other forms of arthritis provided initial hope for potential application in back arthritis.
- 2010s: Advancements in imaging techniques, such as MRI and CT scans, provided more detailed insights into the structural changes occurring in the affected joints. Growing recognition of the importance of lifestyle factors, like exercise and weight management, in managing back arthritis. The development of targeted biologics for other inflammatory conditions led to increased interest in exploring similar approaches for back arthritis.
- 2020s: Ongoing research focuses on personalized medicine approaches, using genetic profiling to identify individuals at high risk. Exploration of novel therapies targeting specific inflammatory pathways. Development of innovative diagnostic tools for early detection and disease monitoring. Studies evaluating the effectiveness of regenerative medicine techniques, such as stem cell therapy, are showing promising results.
Potential of New Therapies and Treatments
The potential of new therapies and treatments for back arthritis is significant. One example is the development of targeted biologics, designed to block specific inflammatory pathways, potentially offering greater efficacy and reduced side effects compared to traditional therapies. Further exploration of regenerative medicine approaches, such as stem cell therapy and gene therapy, holds promise for restoring damaged cartilage and promoting tissue repair.
Furthermore, advancements in nanotechnology may lead to the development of novel drug delivery systems that improve treatment efficacy. Early trials of such approaches have shown promising results, providing a glimmer of hope for improved outcomes in the future.
Illustrative Case Studies
Understanding the diverse presentations of back arthritis requires exploring real-world examples. Case studies offer valuable insights into the clinical course, diagnostic challenges, and treatment responses of individuals affected by this condition. They provide a tangible way to connect theoretical knowledge with practical application.
Case studies allow for a detailed examination of individual experiences, highlighting the variability in symptoms, severity, and responses to treatment. They can also shed light on the potential complications and long-term outcomes associated with various types of back arthritis.
Case Study 1: Ankylosing Spondylitis
This case involves a 27-year-old male presenting with persistent low back pain, stiffness, and morning joint pain. The pain had progressively worsened over several months, affecting his mobility and daily activities. He also reported pain radiating to his buttocks and thighs. Physical examination revealed limited spinal mobility and tenderness over the lumbar spine. X-rays revealed characteristic changes consistent with ankylosing spondylitis, such as sacroiliitis and syndesmophytes.
Treatment included nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy, aiming to reduce pain and improve spinal mobility. Over the next year, the patient experienced significant improvement in pain and functional capacity. Continued physical therapy and medication management helped maintain this improvement.
Case Study 2: Rheumatoid Arthritis
A 45-year-old female experienced progressive low back pain, accompanied by swelling and stiffness in the small joints of her hands and feet. She also reported fatigue and general malaise. Laboratory tests revealed elevated inflammatory markers, characteristic of rheumatoid arthritis. Imaging studies, including MRI and X-rays, demonstrated erosive changes in the sacroiliac joints and surrounding tissues. The treatment plan focused on disease-modifying antirheumatic drugs (DMARDs), in addition to NSAIDs, to manage inflammation and prevent further joint damage.
The patient experienced a reduction in pain and joint swelling, and her overall functional capacity improved.
Case Study 3: Psoriatic Arthritis
A 32-year-old male presented with back pain and stiffness, along with a history of psoriasis on his scalp and elbows. Physical examination revealed dactylitis (sausage-like swelling of the fingers) and tenderness in the lower back. Blood tests showed elevated inflammatory markers. Imaging revealed characteristic changes in the sacroiliac joints, indicative of psoriatic arthritis. The treatment involved a combination of topical therapies for psoriasis, NSAIDs, and methotrexate to manage the inflammatory response in the back and other affected joints.
The patient’s back pain significantly improved, and he regained a considerable amount of functional capacity over the course of treatment.
Comparison of Case Studies, Arthritis in back treatment
| Characteristic | Case Study 1 (Ankylosing Spondylitis) | Case Study 2 (Rheumatoid Arthritis) | Case Study 3 (Psoriatic Arthritis) |
|---|---|---|---|
| Age | 27 | 45 | 32 |
| Presenting Symptoms | Low back pain, stiffness, morning joint pain, radiating pain | Low back pain, joint swelling, stiffness, fatigue | Back pain, stiffness, dactylitis, psoriasis history |
| Diagnostic Findings | Sacroiliitis, syndesmophytes (x-ray) | Erosive changes in sacroiliac joints (MRI, X-ray), elevated inflammatory markers | Sacroiliitis changes (imaging), elevated inflammatory markers, psoriasis |
| Treatment Approach | NSAIDs, physical therapy | DMARDs, NSAIDs | Topical psoriasis treatments, NSAIDs, methotrexate |
| Outcomes | Significant improvement in pain and function | Reduction in pain and swelling, improved function | Improved back pain, regained functional capacity |
Final Summary: Arthritis In Back Treatment
In conclusion, arthritis in back treatment necessitates a multi-faceted approach that considers the specific type of arthritis, individual needs, and potential complications. By understanding the underlying mechanisms, diagnostic procedures, and available treatments, individuals can work collaboratively with healthcare professionals to manage their condition effectively. Maintaining a healthy lifestyle, coupled with appropriate medical interventions, is key to mitigating long-term consequences and improving overall well-being.
This guide aims to provide a solid foundation for informed decision-making in the journey toward managing back arthritis.

