Antibiotics for sinus infection sets the stage for a deep dive into the world of sinus health. We’ll explore the causes, symptoms, and treatments, highlighting the crucial role of antibiotics in resolving bacterial infections. Understanding the different types of antibiotics, their mechanisms, and potential side effects is key to making informed decisions about your health.
This comprehensive guide will cover everything from the basics of sinus infections to the latest research on antibiotic resistance. We’ll also discuss alternative treatments and when they might be preferable to antibiotics. This isn’t just about facts; it’s about empowering you with knowledge to navigate this important health issue.
Introduction to Sinus Infections
Sinus infections, also known as sinusitis, are common respiratory illnesses that affect the air-filled spaces (sinuses) behind the nose and eyes. These infections can be incredibly uncomfortable and, if left untreated, can lead to more serious complications. Understanding the causes, symptoms, and appropriate treatment is crucial for managing these infections effectively.Sinus infections typically arise from a combination of factors, including viral infections (like the common cold), bacterial infections, or allergies.
These irritants can cause inflammation and swelling in the sinus lining, leading to a buildup of mucus and a blockage of the sinus passages. This blockage prevents the proper drainage of mucus, creating an ideal environment for bacterial growth, and further exacerbating the infection.
Causes of Sinus Infections
Viral infections are the most common culprits behind sinus infections. These infections often precede bacterial sinusitis, as the initial inflammation created by the virus can make the sinuses more susceptible to bacterial colonization. Allergies, particularly seasonal allergies, can also contribute to the development of sinusitis due to the inflammation and mucus production they trigger. Certain fungal infections can also lead to sinusitis, although less frequently.
Foreign objects, like small particles or irritants, may occasionally cause sinus infections.
Symptoms of Sinus Infections
Common symptoms of sinus infections include facial pain or pressure, especially around the forehead, cheeks, or eyes. Nasal congestion and a thick, discolored nasal discharge are also prevalent symptoms. Fever, headache, and fatigue can accompany the infection. Postnasal drip, a sensation of mucus running down the back of the throat, is another frequently reported symptom. These symptoms can vary in severity depending on the type and cause of the infection.
Types of Sinus Infections
Sinusitis can be broadly categorized into acute, subacute, and chronic forms. Acute sinusitis typically lasts for a short period, usually less than four weeks, and is often triggered by a viral infection. Subacute sinusitis lasts between four and twelve weeks, and chronic sinusitis persists for more than twelve weeks. These distinctions in duration are important for proper diagnosis and treatment.
The symptoms of each type may overlap, making diagnosis complex.
Importance of Proper Diagnosis and Treatment
Accurate diagnosis is paramount to ensure appropriate treatment. A healthcare professional can properly assess the symptoms, conduct a physical examination, and potentially order diagnostic tests to determine the underlying cause of the infection, whether it’s viral, bacterial, or fungal. Delaying or neglecting treatment can lead to complications, such as ear infections, spread of infection to surrounding tissues, or even more serious systemic issues.
Role of Antibiotics in Treating Sinus Infections
Antibiotics are typically reserved for bacterial sinusitis, as they are ineffective against viral infections. The decision to prescribe antibiotics depends on factors such as the patient’s medical history, symptom duration, and severity. In cases of viral sinusitis, symptom management with rest, hydration, and over-the-counter pain relievers is often sufficient. In bacterial cases, antibiotics can help reduce the infection’s duration and severity.
Table of Sinus Infection Types
| Infection Type | Symptoms | Duration | Typical Treatment (including antibiotics) |
|---|---|---|---|
| Acute Bacterial Sinusitis | Facial pain, nasal congestion, thick nasal discharge, fever | Less than 4 weeks | Antibiotics (e.g., amoxicillin, amoxicillin-clavulanate), pain relievers, nasal saline rinses |
| Acute Viral Sinusitis | Similar symptoms to bacterial sinusitis, but often less severe | Less than 4 weeks | Rest, hydration, over-the-counter pain relievers, nasal saline rinses |
| Subacute Sinusitis | Persistent symptoms beyond 4 weeks, but less severe than chronic | 4-12 weeks | Antibiotics (if bacterial), pain relievers, nasal corticosteroids, nasal saline rinses |
| Chronic Sinusitis | Persistent symptoms for more than 12 weeks | More than 12 weeks | Antibiotics (if bacterial), nasal corticosteroids, nasal saline rinses, possible surgery in severe cases |
Types of Antibiotics for Sinus Infections
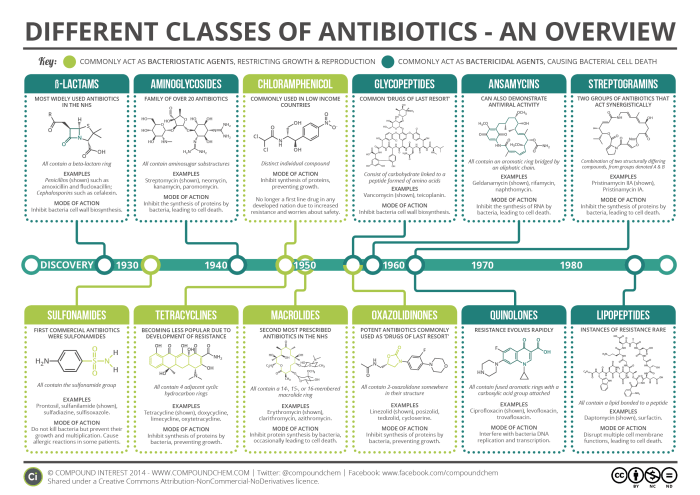
Sinus infections, also known as sinusitis, are often treated with antibiotics to combat the bacterial cause. Understanding the various types of antibiotics used, their mechanisms of action, and their potential side effects is crucial for informed decision-making regarding treatment. Choosing the right antibiotic is vital for effective therapy and minimizing adverse reactions.Different classes of antibiotics target specific bacterial mechanisms, leading to varied effectiveness and side effect profiles.
Factors like the specific bacteria causing the infection and individual patient sensitivities influence the optimal antibiotic selection. A healthcare professional will carefully consider these factors when prescribing an antibiotic.
Common Antibiotic Classes for Sinus Infections
Several classes of antibiotics are commonly prescribed for sinus infections. These antibiotics work by interfering with bacterial growth and reproduction through different mechanisms.
Mechanisms of Action
Antibiotics within different classes disrupt bacterial processes in unique ways. Penicillins, for example, inhibit the synthesis of bacterial cell walls, a crucial component for their survival. Macrolides, on the other hand, target bacterial protein synthesis, a fundamental process for bacterial growth. Cephalosporins, another important class, also target bacterial cell wall synthesis, though with a slightly different mechanism than penicillins.
Effectiveness and Side Effects Comparison
The effectiveness and side effect profiles of different antibiotic classes can vary. Penicillins, often a first-line treatment, are generally effective against many common bacterial causes of sinus infections. However, some bacteria have developed resistance to penicillins, reducing their efficacy in certain cases. Macrolides may be more effective against specific types of bacteria, but may also cause more gastrointestinal side effects.
Cephalosporins represent a broader spectrum of activity than penicillins, but also carry the risk of more potential side effects. Ultimately, the choice of antibiotic depends on the specific bacterial cause of the infection, as well as the patient’s individual medical history and sensitivities.
Antibiotic Comparison Table
| Antibiotic Class | Mechanism of Action | Typical Dosage | Potential Side Effects |
|---|---|---|---|
| Penicillins | Inhibit bacterial cell wall synthesis. | Variable, depending on the specific penicillin and severity of infection. Typically 250-500 mg every 6-8 hours. | Allergic reactions (rash, hives, itching), nausea, diarrhea, vomiting. |
| Cephalosporins | Also inhibit bacterial cell wall synthesis, but with a different mechanism than penicillins. | Variable, depending on the specific cephalosporin and severity of infection. Typically 250-500 mg every 6-8 hours. | Allergic reactions (more common than penicillins), diarrhea, nausea, vomiting, abdominal pain. |
| Macrolides | Interfere with bacterial protein synthesis. | Variable, depending on the specific macrolide and severity of infection. Typically 250-500 mg every 6-12 hours. | Gastrointestinal upset (nausea, vomiting, diarrhea), headache, dizziness, skin rash. |
Treatment Protocols and Considerations
Treating sinus infections effectively involves a multi-faceted approach, focusing on both symptom relief and the underlying cause. Understanding the typical treatment protocol, the factors influencing antibiotic choice, and the importance of completing the prescribed course are crucial for successful management. This section details these critical aspects.The treatment protocol for sinus infections often centers on addressing the symptoms while also targeting any bacterial infection.
This usually involves a combination of medication and lifestyle adjustments. Proper diagnosis is paramount, ensuring that the treatment aligns with the specific type of infection and individual patient needs.
Typical Treatment Protocol Overview
Sinus infections, especially bacterial ones, often respond well to antibiotics. A typical treatment protocol involves the administration of antibiotics to eliminate the bacteria causing the infection. This is usually combined with measures to manage symptoms like pain, fever, and nasal congestion. Rest, hydration, and over-the-counter pain relievers are frequently recommended to alleviate discomfort.
Factors Influencing Antibiotic Choice
Several factors influence the choice of antibiotics for a sinus infection. These factors include the suspected causative bacteria, the patient’s medical history, allergies, and potential drug interactions. Doctors consider the susceptibility of the bacteria to various antibiotics to ensure the most effective treatment.
Duration of Antibiotic Treatment
Completing the full course of antibiotics as prescribed is essential. Stopping treatment prematurely can allow the bacteria to potentially multiply and potentially lead to a relapse or more persistent infection. This is especially critical because incomplete treatment may lead to antibiotic resistance, rendering future treatments less effective.
Importance of Following Medical Advice and Monitoring Symptoms
Adherence to medical advice is critical for successful treatment. Regular monitoring of symptoms and reporting any changes to the prescribing physician is vital. This allows for prompt adjustments to the treatment plan if needed. Regular follow-up appointments are also important for evaluating the response to treatment.
| Patient Profile | Infection Type | Prescribed Antibiotics | Treatment Duration |
|---|---|---|---|
| Adult with no known allergies, history of sinus infections | Bacterial sinus infection (likely Streptococcus pneumoniae) | Amoxicillin | 7-10 days |
| Child with a history of penicillin allergy | Bacterial sinus infection (likely Haemophilus influenzae) | Cefuroxime | 7-10 days |
| Adult with chronic sinusitis, taking multiple medications | Bacterial sinus infection (potentially resistant strains) | Levofloxacin | 10-14 days |
| Pregnant woman with mild sinus infection | Bacterial sinus infection (likely Streptococcus pyogenes) | Amoxicillin-clavulanate | 7-10 days |
Bacterial vs. Viral Sinus Infections
Sinus infections, often causing throbbing pain and discomfort, can be either bacterial or viral in origin. Understanding the difference is crucial for proper treatment, as the approaches vary significantly. Incorrectly identifying the cause can lead to unnecessary antibiotic use or, conversely, delayed treatment for a bacterial infection.Distinguishing between these two types hinges on factors beyond the immediate symptoms.
While antibiotics are often prescribed for sinus infections, it’s crucial to understand their limitations. Sometimes, a positive herpes IGG test result can lead to confusion about the cause of symptoms, potentially delaying the appropriate treatment for a sinus infection. Understanding what a positive herpes IGG test means is key to getting the right diagnosis and effective treatment for sinus infections.
what does a positive herpes IGG test mean Ultimately, proper diagnosis and treatment of the sinus infection remain paramount.
Viral infections are the more common cause of sinus congestion, typically resolving on their own within a week or two. Bacterial infections, on the other hand, require specific antibiotic treatment to clear the infection and prevent potential complications.
Distinguishing Symptoms
Viral sinus infections often present with a gradual onset of symptoms, such as a runny nose (often initially clear, then becoming discolored), sneezing, and a mild headache. These symptoms tend to be less severe than those associated with bacterial infections. In contrast, bacterial sinus infections often manifest with a more rapid onset of symptoms, accompanied by increased pain and pressure in the face, thick, discolored nasal discharge (yellow or green), and a fever.
Severe pain and persistent symptoms that last longer than a week are strong indicators that a bacterial infection may be present.
Situations Requiring Antibiotics
Antibiotics are essential when a bacterial sinus infection is suspected, as they target the bacteria causing the infection. They are not effective against viruses. In situations where a bacterial infection is suspected, prompt antibiotic treatment is critical to reduce the duration of the illness and prevent potential complications like acute bacterial rhinosinusitis (ABRS). However, it is crucial to note that antibiotic use should be guided by a healthcare professional, as they can have side effects and contribute to antibiotic resistance if used inappropriately.
Importance of Accurate Diagnosis
An accurate diagnosis is paramount in determining the appropriate treatment for a sinus infection. A healthcare provider will typically assess the patient’s symptoms, medical history, and conduct a physical examination to determine the cause of the infection. This assessment helps differentiate between viral and bacterial causes and identify potential complications. Without a proper diagnosis, inappropriate treatment may be administered, delaying recovery and potentially causing harm.
While antibiotics are often prescribed for sinus infections, it’s crucial to understand the potential interplay with other health concerns. For example, if you have a history of grade 1 diastolic dysfunction, grade 1 diastolic dysfunction might influence the treatment approach to your sinus infection. Ultimately, proper diagnosis and personalized care remain key when considering antibiotics for sinus infections.
Treatment Considerations
Determining the right course of action for sinus infections is vital for effective recovery. Treatment protocols for viral infections typically involve supportive care, focusing on alleviating symptoms like pain and congestion. Antibiotics are only necessary for bacterial infections. Proper diagnosis and understanding of the specific type of infection is crucial to avoiding unnecessary antibiotic use, which can lead to antibiotic resistance and adverse side effects.
Bacterial vs. Viral Sinus Infection Comparison
| Infection Type | Symptoms | Typical Duration | Recommended Treatment |
|---|---|---|---|
| Viral | Runny nose (clear to discolored), sneezing, mild headache, gradual onset | 7-10 days | Rest, fluids, over-the-counter pain relievers, decongestants |
| Bacterial | Severe facial pain, pressure, thick discolored nasal discharge (yellow or green), fever, rapid onset | More than 10 days | Antibiotics, prescribed by a healthcare professional |
Side Effects and Precautions
Taking antibiotics for a sinus infection can be beneficial, but it’s crucial to understand the potential side effects and precautions. While antibiotics effectively target bacterial infections, they can also disrupt the delicate balance of your gut flora and lead to various adverse reactions. Knowing these risks empowers you to make informed decisions about your treatment plan and ensure responsible antibiotic use.
Potential Side Effects of Antibiotics
Antibiotics, though essential for combating bacterial infections, can have various side effects, ranging from mild discomfort to more serious complications. These side effects are a result of the drugs’ impact on different bodily systems. Understanding these effects helps patients and healthcare providers manage potential issues effectively.
- Gastrointestinal Issues: Antibiotics can disrupt the normal gut bacteria, leading to diarrhea, nausea, vomiting, and abdominal cramps. This is particularly true for broad-spectrum antibiotics that affect a wider range of bacteria.
- Allergic Reactions: Some individuals are allergic to specific antibiotics. Symptoms of an allergic reaction can range from mild skin rashes to more severe reactions like hives, swelling, and difficulty breathing. Severe allergic reactions, known as anaphylaxis, require immediate medical attention.
- Headaches and Dizziness: Certain antibiotics can cause headaches and dizziness, particularly in susceptible individuals. These side effects are often mild and temporary, but they can be disruptive and should be monitored.
- Yeast Infections: Antibiotics can kill beneficial bacteria in the body, leading to an overgrowth of yeast, especially in the vagina or mouth. This can result in vaginal yeast infections or oral thrush.
Precautions While Using Antibiotics
Taking antibiotics correctly is essential to maximize their effectiveness and minimize potential side effects. These precautions ensure responsible use and help prevent unnecessary complications.
- Complete the Entire Course: It’s critical to complete the full course of antibiotics, even if you feel better. Stopping prematurely can allow resistant bacteria to survive and potentially lead to a relapse of the infection.
- Proper Dosage and Timing: Adhering to the prescribed dosage and timing is vital. Taking the medication at the wrong time or in the incorrect amount can reduce its effectiveness and increase the risk of side effects.
- Avoid Mixing with Alcohol: Some antibiotics can interact negatively with alcohol, leading to unpleasant side effects. It’s crucial to avoid alcohol consumption while taking antibiotics unless advised otherwise by a healthcare professional.
- Inform Your Doctor of Other Medications: If you are taking other medications, including over-the-counter drugs or supplements, it’s important to inform your doctor. Certain combinations can lead to adverse interactions.
Importance of Avoiding Antibiotic Overuse
Antibiotic overuse contributes to the development of antibiotic-resistant bacteria, a serious global health concern. The widespread misuse of antibiotics weakens their effectiveness, making infections harder to treat in the future.
- Antibiotic Resistance: The overuse of antibiotics creates an environment where bacteria develop resistance to these drugs. This resistance can lead to treatment failures and prolonged illnesses.
- Spread of Resistance: Resistant bacteria can spread to others, potentially causing outbreaks of infections that are difficult to control.
- Treatment Challenges: As antibiotic resistance increases, treatments for various infections become less effective, potentially requiring more potent and potentially more toxic medications.
Potential Adverse Reactions to Antibiotics
Various adverse reactions can occur from antibiotic use. Recognizing these potential complications is essential for prompt medical intervention.
- Skin Rashes: Antibiotics can cause skin rashes, ranging from mild to severe. These can be accompanied by itching and other symptoms.
- Liver Damage: Some antibiotics can cause liver damage in certain individuals, which may require monitoring or adjustments to the treatment plan.
- Kidney Problems: Certain antibiotics can put a strain on the kidneys, potentially leading to kidney problems, particularly in individuals with pre-existing kidney conditions.
Antibiotic Side Effect Table
| Antibiotic | Potential Side Effects | Severity | Prevention Strategies |
|---|---|---|---|
| Penicillin | Diarrhea, Nausea, Vomiting, Rash, Allergic reactions | Mild to Moderate | Take as prescribed, monitor for symptoms, inform doctor of other medications |
| Amoxicillin | Diarrhea, Nausea, Vomiting, Abdominal cramps, Rash | Mild to Moderate | Take with food, stay hydrated, inform doctor of other medications |
| Cephalosporins | Diarrhea, Nausea, Vomiting, Rash, Allergic reactions, Yeast infections | Mild to Moderate | Take with food, monitor for symptoms, inform doctor of other medications |
| Macrolides | Diarrhea, Nausea, Vomiting, Dizziness, Rash, Allergic reactions | Mild to Moderate | Take with food, monitor for symptoms, inform doctor of other medications |
Alternatives to Antibiotics
Sometimes, a sinus infection doesn’t require the heavy artillery of antibiotics. Many effective alternatives can help alleviate symptoms and promote healing, particularly when the infection is viral or the symptoms are mild. These approaches focus on relieving discomfort, supporting the body’s natural defenses, and preventing complications.A crucial aspect of managing sinus infections is understanding that antibiotics only treat bacterial infections.
Viral infections, which are very common, often require a different approach focused on symptom relief and allowing the body to fight the infection naturally. Alternative treatments are often preferable when a bacterial infection is suspected but not confirmed, or when the patient wishes to avoid the potential side effects of antibiotics.
Nasal Rinses and Sprays
Nasal irrigation, using a saline solution to rinse the nasal passages, is a common and effective home remedy for sinus infections. Saline rinses help to clear out mucus and debris, reducing congestion and promoting drainage. Saline sprays, in contrast, provide ongoing moisture and can also help to soothe irritated nasal membranes.These methods are often safe and effective in reducing inflammation and promoting drainage, which is crucial for alleviating pressure and discomfort associated with sinus infections.
However, it’s important to use a sterile solution and to follow proper rinsing techniques to avoid potential complications.
Pain Relievers
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can effectively reduce fever and pain associated with sinus infections. These medications can provide significant relief from headaches, facial pain, and body aches, improving overall comfort and well-being.While pain relievers don’t directly address the infection, they play a vital role in managing symptoms and improving the patient’s quality of life. They are frequently used in conjunction with other treatments to provide comprehensive relief.
Home Remedies and Supportive Care
Rest, hydration, and a healthy diet play a crucial role in supporting the body’s natural healing process during a sinus infection. Getting adequate rest allows the body to allocate resources to fighting the infection. Staying hydrated helps thin mucus and promotes drainage. A diet rich in fruits, vegetables, and whole grains provides essential nutrients to support immune function.
Alternative Treatments: A Summary
- Nasal Rinses/Sprays: These treatments can help clear nasal passages, reducing congestion and promoting drainage. Benefits include reduced discomfort and potential prevention of complications. Drawbacks include the need for proper technique to avoid complications and potential discomfort during initial use.
- Pain Relievers: Effective in reducing fever and pain, improving overall comfort. Benefits include symptom relief. Drawbacks include potential side effects, especially with prolonged use, and they don’t directly address the infection.
- Home Remedies and Supportive Care: Rest, hydration, and a healthy diet support the body’s natural defenses. Benefits include overall improvement in well-being and potential acceleration of healing. Drawbacks are limited; primarily that these remedies alone may not fully resolve the infection in severe cases.
When Alternatives May Be Insufficient
While alternative treatments are often effective for managing mild to moderate sinus infections, situations exist where they may be insufficient. Severe infections, persistent symptoms, or complications like fever, high pain, or significant discomfort may require further medical intervention. This includes situations where the infection worsens or does not improve with conservative measures.In these cases, a doctor’s evaluation is crucial to determine the appropriate course of action.
Resistance and Overuse: Antibiotics For Sinus Infection
Antibiotics are powerful tools in fighting bacterial infections, but their overuse has created a serious problem: antibiotic resistance. This means that bacteria are evolving to become less susceptible to the drugs we use to treat them. This poses a significant threat to public health, making it harder to treat common infections, and potentially leading to more severe and prolonged illnesses.
Taking antibiotics for a sinus infection can be a quick fix, but what about the impact on your overall health? While we’re on the subject of inflammatory issues, did you know that certain foods might worsen gout? For example, figuring out if tomatoes are a good choice when you have gout is a crucial part of managing the condition.
You can explore this further by checking out this resource on are tomatoes bad for gout. Ultimately, consulting a doctor is key for determining the best course of action for sinus infections and any other health concerns.
This is particularly concerning for sinus infections, where responsible antibiotic use is crucial.
The Problem of Antibiotic Resistance
Antibiotic resistance occurs when bacteria develop the ability to withstand the effects of antibiotics. This happens through genetic mutations, which allow them to survive and reproduce even in the presence of the drugs. Over time, these resistant bacteria can proliferate, leading to widespread infections that are difficult or impossible to treat with standard antibiotics. For example, methicillin-resistant Staphylococcus aureus (MRSA) is a significant healthcare concern due to its resistance to many commonly used antibiotics.
Consequences of Antibiotic Overuse in Sinus Infections
The overuse of antibiotics for sinus infections, often when the infection is viral and thus unresponsive to antibiotics, contributes directly to the development of antibiotic resistance. When antibiotics are prescribed unnecessarily, bacteria are exposed to lower concentrations of the drug, allowing them to adapt and survive. This selection pressure drives the evolution of resistant strains. This not only impacts the individual with the sinus infection but also the broader community by making infections more difficult to treat in the future.
Importance of Responsible Antibiotic Use
Responsible antibiotic use is essential for preserving the effectiveness of these vital medications. This involves only taking antibiotics when they are absolutely necessary, as prescribed by a healthcare professional. Patients should also complete the full course of antibiotics, even if symptoms improve, to ensure all bacteria are eliminated and to prevent the development of resistant strains. Failing to complete a course can allow some bacteria to survive and potentially develop resistance.
Factors Contributing to Antibiotic Resistance
Several factors contribute to the development and spread of antibiotic resistance. These include:
- Inappropriate Prescribing: Antibiotics are sometimes prescribed for viral infections, such as the common cold or the flu, which do not respond to antibiotics. This unnecessary use selects for resistant bacteria.
- Incomplete Treatment Courses: Patients may stop taking antibiotics as soon as they feel better, even if the full course has not been completed. This allows some bacteria to survive and potentially develop resistance.
- Agricultural Use: Antibiotics are often used in animal agriculture to promote growth and prevent disease. This can lead to the presence of resistant bacteria in animal products, which can then be transmitted to humans.
- Poor Hygiene Practices: Poor hygiene can contribute to the spread of resistant bacteria, especially in healthcare settings. Maintaining proper handwashing and sanitation protocols can reduce the transmission of resistant bacteria.
“Responsible antibiotic use is critical in preventing the evolution of antibiotic resistance. It safeguards the effectiveness of these life-saving drugs for future generations.”
Diagnosis and Confirmation
Pinpointing the cause of sinus discomfort is crucial for appropriate treatment. A thorough evaluation by a healthcare professional, including a physical examination and potentially diagnostic tests, is essential to distinguish between viral and bacterial infections, and to rule out other potential conditions. This process ensures the most effective and targeted approach to alleviate symptoms and prevent complications.Accurate diagnosis hinges on a careful assessment of symptoms, medical history, and physical examination findings.
The healthcare provider will meticulously consider the duration and severity of the symptoms, as well as any accompanying conditions or allergies. This comprehensive approach allows for a more precise identification of the underlying cause.
Diagnostic Process Overview, Antibiotics for sinus infection
The diagnostic process for sinus infections typically begins with a detailed history taking session. This involves gathering information about the patient’s symptoms, such as the onset, duration, and characteristics of the pain, nasal discharge, and fever. The medical history is equally important, as it provides context for potential contributing factors or pre-existing conditions. A physical examination follows, focusing on the sinuses, nasal passages, and surrounding areas.
This physical assessment often includes palpation of the sinuses to identify any tenderness or swelling.
Diagnostic Tests
Several tests may be utilized to aid in the diagnosis of sinus infections. These tests help to confirm the presence of infection, determine the type of pathogen involved, and rule out other possible causes.
- Nasal endoscopy: A thin, flexible tube with a light and camera is inserted through the nose to visualize the nasal passages and sinuses. This allows for direct observation of the inflammation, discharge, and any structural abnormalities. This procedure is often used to assess the extent of the infection and identify potential complications.
- Imaging studies (e.g., CT scan): Computed tomography (CT) scans provide detailed cross-sectional images of the sinuses. They can help identify any structural abnormalities, fluid accumulation, or bone erosion, which can indicate a more severe infection or complications. A CT scan is particularly helpful in cases of suspected chronic sinusitis or complications like orbital cellulitis.
- Culture and sensitivity testing: This laboratory test involves collecting a sample of nasal discharge or mucus. The sample is then analyzed to identify the specific bacteria causing the infection. Knowing the type of bacteria is critical, as it dictates the most effective antibiotic treatment. This testing also determines the bacteria’s sensitivity to different antibiotics, guiding the selection of the most appropriate medication.
Information Required for Accurate Diagnosis
Accurate diagnosis relies on providing the healthcare professional with complete and precise information. This includes details about the onset, duration, and intensity of symptoms, any associated symptoms (e.g., fever, headache, facial pain), and any recent illnesses or exposures. This comprehensive information allows for a more informed assessment and helps differentiate between sinus infections and other conditions with similar symptoms.
Importance of Consulting a Healthcare Professional
Self-treating a sinus infection can be risky. Improper diagnosis and treatment can lead to prolonged symptoms, complications, or the development of antibiotic resistance. A healthcare professional is trained to evaluate the specific situation and determine the appropriate course of action. Consulting a doctor ensures the correct diagnosis and tailored treatment plan for the individual patient’s needs.
Diagnostic Methods Table
| Diagnostic Method | Procedure | Expected Results | Implications |
|---|---|---|---|
| Nasal Endoscopy | Visual examination of nasal passages and sinuses using a flexible endoscope. | Visualization of inflammation, discharge, and structural abnormalities. | Helps identify the extent of the infection and potential complications. |
| CT Scan | Detailed cross-sectional images of the sinuses using X-rays. | Visualization of structural abnormalities, fluid accumulation, or bone erosion. | Useful for suspected chronic sinusitis or complications like orbital cellulitis. |
| Culture and Sensitivity | Collection and analysis of nasal discharge to identify bacteria and determine antibiotic susceptibility. | Identification of specific bacteria and their sensitivity to different antibiotics. | Allows for targeted antibiotic treatment and prevents the development of antibiotic resistance. |
Patient Education and Self-Care

Understanding sinus infections and taking proactive steps towards managing symptoms are crucial for a swift recovery and to prevent complications. This involves recognizing the warning signs, following prescribed treatments, implementing self-care measures, and practicing good hygiene to prevent spreading the infection. By actively participating in your care, you can significantly improve your well-being and reduce the likelihood of long-term issues.
Recognizing the Signs and Symptoms of Sinus Infections
Sinus infections, often confused with other respiratory illnesses, present with a combination of symptoms. Identifying these early can help you seek appropriate medical attention and initiate self-care measures. Common symptoms include facial pain or pressure, particularly around the forehead, cheeks, or eyes, often accompanied by nasal congestion, a thick or discolored nasal discharge, and postnasal drip. Headaches, fever, and fatigue are also frequent companions to sinus infections.
A persistent cough and loss of smell or taste can also indicate a sinus infection, especially if coupled with other symptoms.
Following Medical Advice and Treatment Plans
Adherence to the prescribed treatment plan is paramount for effective management of sinus infections. This includes taking antibiotics as directed, even if symptoms improve, to ensure the infection is fully eradicated. Skipping doses or stopping medication prematurely can lead to the infection persisting or recurring, potentially causing more severe complications. Regular follow-up appointments with your healthcare provider are also crucial to monitor your progress and address any concerns.
Self-Care Measures to Relieve Symptoms
Various self-care strategies can alleviate the discomfort associated with sinus infections. These measures should be used in conjunction with prescribed medical treatments, not as a replacement. Rest and hydration are essential, as they support the body’s natural healing process. Warm compresses applied to the affected areas can ease pain and swelling. Using a humidifier can help moisten the nasal passages, reducing congestion.
Over-the-counter pain relievers, such as ibuprofen or acetaminophen, can help manage fever and pain. Saline nasal sprays or rinses can help clear out nasal passages and reduce inflammation.
Methods to Prevent the Spread of Infections
Preventing the spread of sinus infections, like other contagious illnesses, involves practicing good hygiene. Regular handwashing with soap and water, especially after touching your face or nose, is critical. Avoiding close contact with individuals who are ill is also important. Covering your mouth and nose when coughing or sneezing with a tissue or your elbow can prevent the spread of germs.
Maintaining a healthy lifestyle, including adequate rest, a balanced diet, and regular exercise, can strengthen your immune system, making you less susceptible to infections.
Table of Sinus Infection Symptoms and Treatment Options
| Symptom | Description | Severity | Treatment Options |
|---|---|---|---|
| Facial Pain/Pressure | Aching or throbbing sensation in the forehead, cheeks, or around the eyes. | Mild to Moderate | Warm compresses, over-the-counter pain relievers, saline nasal sprays. |
| Nasal Congestion | Difficulty breathing through the nose due to swelling and mucus buildup. | Mild to Moderate | Saline nasal sprays, humidifiers, nasal irrigation, over-the-counter decongestants (use cautiously). |
| Nasal Discharge | Thick, discolored (yellow or green) mucus draining from the nose. | Mild to Moderate | Saline nasal sprays, nasal irrigation, antibiotics (if bacterial). |
| Headache | Pain in the head, often localized around the sinuses. | Mild to Moderate | Over-the-counter pain relievers, rest, warm compresses. |
| Fever | Elevated body temperature. | Mild to Moderate | Rest, fluids, over-the-counter fever reducers (e.g., acetaminophen). Consult a doctor if fever is high or persistent. |
Concluding Remarks
In conclusion, understanding antibiotics for sinus infection requires a nuanced approach. While antibiotics are vital for bacterial sinus infections, overuse can lead to resistance. This guide has highlighted the importance of proper diagnosis, the diverse range of antibiotics available, and the significance of alternative treatments. By arming yourself with knowledge, you can make informed choices about your health and well-being.

