Herniated disc physical therapy is a crucial aspect of managing and recovering from a herniated disc. It’s a personalized approach, focusing on restoring function, relieving pain, and improving overall well-being. This guide delves into the various facets of herniated disc physical therapy, from understanding the condition itself to exploring different treatment methods and patient education.
We’ll cover everything from the different types of herniated discs and their symptoms to the specific exercises, manual therapies, and patient self-management strategies used in treatment. We’ll also examine the role of equipment and technology, case studies, potential complications, and prevention strategies. This comprehensive guide aims to equip you with the knowledge to navigate this journey effectively.
Introduction to Herniated Disc Physical Therapy

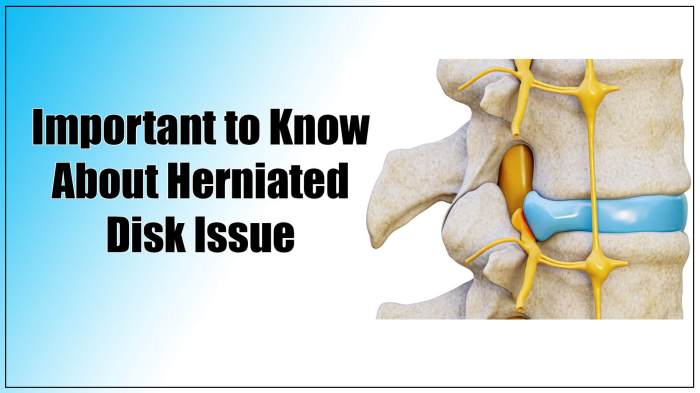
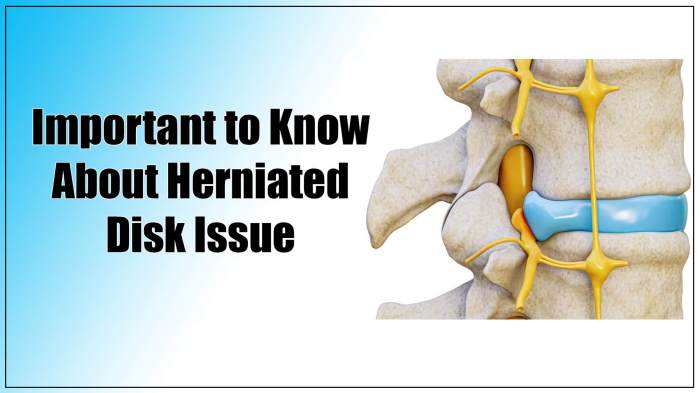
A herniated disc, also known as a slipped disc, is a common spinal condition. It occurs when the soft, jelly-like center of a spinal disc bulges or ruptures through a tear in the tough outer layer. This can put pressure on nearby nerves, causing pain and other symptoms. Understanding the causes, symptoms, and importance of early intervention can significantly impact recovery.Herniated discs are a significant concern for individuals of all ages, from young athletes to older adults.
The consequences of untreated herniated discs can range from chronic pain to long-term disability. Early detection and proactive management, including physical therapy, are crucial for minimizing the impact of this condition and restoring function.
Causes of Herniated Discs
Several factors contribute to the development of herniated discs. Age-related degeneration of the spinal discs, often accelerated by repetitive stress or trauma, is a major cause. Repetitive heavy lifting, poor posture, and prolonged sitting can strain the spine and increase the risk of herniation. Obesity, smoking, and certain occupations with significant physical demands are also linked to a higher incidence of herniated discs.
Symptoms of Herniated Discs
Herniated discs manifest in a variety of symptoms, often depending on the location and severity of the herniation. Common symptoms include lower back pain, radiating pain down the leg (sciatica), numbness or tingling in the affected leg or foot, and muscle weakness. Pain intensity can vary greatly, from mild discomfort to debilitating agony. The specific symptoms experienced by an individual can differ depending on the location of the affected disc and the severity of the herniation.
Importance of Early Intervention and Physical Therapy
Early intervention in managing a herniated disc is crucial. Physical therapy plays a vital role in restoring function, relieving pain, and preventing further damage. A structured physical therapy program can strengthen core muscles, improve posture, and increase flexibility, all of which contribute to a more stable spine and reduced risk of future herniations. The program can also help to manage pain, increase range of motion, and improve overall spinal health.
Types of Herniated Discs
Understanding the different types of herniated discs can help in tailoring treatment plans. A proper diagnosis is critical to ensuring the most effective course of action.
| Type | Description | Symptoms |
|---|---|---|
| Bulging Disc | The soft inner material of the disc bulges outward, but does not rupture the outer layer. | May cause mild to moderate back pain, often with minimal radiating symptoms. |
| Prolapsed Disc | The inner material of the disc protrudes through a tear in the outer layer. | Can cause moderate to severe back pain, often accompanied by radiating pain and numbness in the legs. |
| Sequestered Disc | A portion of the inner disc material breaks away and moves further from the disc. | Usually more severe than prolapsed or bulging discs, with significant pain and potential neurological compromise. |
Goals and Objectives of Physical Therapy
Physical therapy for herniated discs focuses on restoring function and alleviating pain. The primary goal is to improve the patient’s quality of life by enabling them to perform daily activities without limitations. This involves addressing the underlying causes of the herniation and its symptoms.Effective physical therapy programs for herniated discs aim for significant improvements in pain management, reduced inflammation, and enhanced mobility.
A key aspect of success is patient engagement and adherence to the prescribed exercises and lifestyle modifications.
Primary Goals of Physical Therapy
Physical therapy for herniated discs aims to reduce pain, improve range of motion, and strengthen supporting muscles. These goals are interconnected and crucial for restoring normal function. By addressing these key areas, patients can anticipate significant improvements in their ability to perform daily tasks and engage in desired activities.
Expected Outcomes of Effective Physical Therapy
Effective physical therapy for herniated discs leads to measurable improvements in pain levels, functional capacity, and overall well-being. Patients often report a substantial decrease in pain intensity and frequency. Improved posture and core strength contribute to long-term stability and reduced risk of recurrence.
Measurable Objectives for a Physical Therapy Program
These objectives provide a framework for assessing the effectiveness of the physical therapy program. They are crucial for monitoring progress and ensuring the program aligns with the patient’s needs.
- Reduce pain intensity by 50% within 4 weeks, measured using a visual analog scale (VAS).
- Increase range of motion in the affected area by 25% within 6 weeks, measured by goniometry.
- Improve functional capacity by achieving a 10-meter walk test time within 8 weeks.
- Increase core muscle strength (e.g., abdominal muscles) by 30% within 12 weeks, measured by manual muscle testing.
- Patient reports reduced limitations in daily activities, such as lifting, bending, and sitting, within 8 weeks.
Key Areas of Focus in Physical Therapy
This table Artikels the key areas of focus in physical therapy for herniated discs. Addressing these areas comprehensively helps in the recovery process.
| Area of Focus | Description | Examples of Interventions |
|---|---|---|
| Pain Management | Reducing pain intensity and frequency through various modalities. | Heat therapy, cold therapy, transcutaneous electrical nerve stimulation (TENS), medication management (if applicable). |
| Posture and Spinal Stabilization | Improving posture and strengthening core muscles to reduce stress on the spine. | Postural exercises, core strengthening exercises (e.g., planks, bridges), proper lifting techniques. |
| Range of Motion Exercises | Increasing flexibility and mobility in the affected area. | Gentle stretching exercises, range of motion exercises, mobilization techniques. |
| Strengthening Exercises | Building strength in muscles surrounding the spine and core. | Isometric exercises, dynamic exercises, resistance training (with proper precautions). |
| Education and Lifestyle Modification | Providing guidance on posture, ergonomics, and daily activities. | Instruction on proper body mechanics, ergonomic adjustments in the workplace, and advice on sleep positions. |
Types of Physical Therapy Exercises
Herniated discs often cause pain and discomfort, limiting movement and daily activities. A crucial component of recovery involves targeted physical therapy exercises. These exercises, when performed correctly, can strengthen supporting muscles, improve flexibility, and promote healing. Understanding the different types of exercises and their proper application is vital for a successful recovery journey.
Strengthening Exercises, Herniated disc physical therapy
Strengthening exercises are fundamental for herniated disc recovery. They help build core strength, which is essential for supporting the spine and reducing pressure on the affected disc. Strengthening the muscles around the spine and core can significantly improve stability and reduce pain. Examples of exercises include planks, bird-dogs, and bridges. Proper form is critical to prevent further injury.
- Plank: Hold a straight line from head to heels, engaging your core. Keep your body aligned, avoiding sagging or arching your back. Maintain a neutral spine throughout the exercise.
- Bird-dog: Start on your hands and knees. Extend one arm forward and the opposite leg backward, maintaining a straight line from head to heels. Engage your core to stabilize your spine. Return to the starting position and repeat on the other side.
- Bridges: Lie on your back with knees bent and feet flat on the floor. Lift your hips off the ground, squeezing your glutes and engaging your core. Hold for a few seconds, then slowly lower your hips back down.
Stretching Exercises
Stretching exercises are vital for improving flexibility and range of motion, which can help reduce pain and stiffness associated with a herniated disc. Stretching tight muscles can alleviate pressure on the affected area. Examples of stretching exercises include hamstring stretches, spinal twists, and quadriceps stretches.
- Hamstring Stretches: Sit on the floor with one leg extended straight in front of you. Lean forward from your hips, keeping your back straight, until you feel a stretch in the back of your thigh. Hold for 20-30 seconds.
- Spinal Twists: Sit with your legs extended or bent. Gently twist your torso from side to side, keeping your back straight. Hold for 20-30 seconds per side.
- Quadriceps Stretches: Stand with one leg slightly bent behind you. Grab your ankle with your hand and pull your heel towards your buttock. Hold for 20-30 seconds.
Stabilization Exercises
Stabilization exercises are crucial for improving the stability of the spine. These exercises focus on engaging the deep core muscles that help support the spine and reduce the risk of further injury. These muscles play a critical role in preventing herniations or exacerbating existing ones. Examples of exercises include pelvic tilts, curl-ups, and side planks.
- Pelvic Tilts: Lie on your back with knees bent and feet flat on the floor. Tighten your abdominal muscles and gently tilt your pelvis upward, pressing your lower back into the floor. Hold for a few seconds and repeat.
- Curl-ups: Lie on your back with knees bent and feet flat on the floor. Slowly curl your upper body towards your knees, engaging your core. Lower your upper body back down to the floor.
- Side Planks: Lie on your side with your elbow directly under your shoulder. Lift your hips off the ground, forming a straight line from head to heels. Engage your core to maintain stability. Hold for a few seconds and repeat.
Exercises to Avoid
Certain exercises can exacerbate a herniated disc. Avoid any exercise that causes sharp or increasing pain. Examples include lifting heavy objects, twisting your torso abruptly, or bending over at the waist without proper support. Always consult with your physical therapist for a personalized exercise plan.
| Exercise Type | Description | Why to Avoid |
|---|---|---|
| Sudden twisting movements | Rapid torso rotation | Can place undue stress on the injured disc. |
| Heavy lifting without proper form | Lifting heavy objects with poor posture. | Increases pressure on the spine. |
| Overextension | Excessive bending at the waist. | Can exacerbate the herniation. |
Manual Therapy Techniques
Manual therapy plays a crucial role in herniated disc physical therapy, aiming to restore proper movement, reduce pain, and improve function. These techniques are often used in conjunction with other therapies like exercise and lifestyle modifications to achieve optimal outcomes. Careful consideration of the patient’s specific condition and overall health is paramount when implementing manual therapy.Manual therapy for herniated discs encompasses a variety of techniques designed to address the underlying causes of pain and dysfunction.
These techniques often focus on restoring spinal mobility, reducing inflammation, and improving the overall biomechanics of the spine. Understanding the rationale, potential benefits, and risks associated with each technique is essential for effective and safe treatment.
Types of Manual Therapy Techniques
Manual therapy techniques for herniated discs are tailored to the specific location and severity of the herniation. The techniques aim to address the pain, reduce muscle spasm, and improve spinal mobility. Careful consideration of the patient’s individual response and overall health is crucial.
Spinal Mobilization/Manipulation
Spinal mobilization and manipulation techniques are commonly used in herniated disc care. These techniques involve controlled movements applied to the affected spinal segments to restore joint mobility and reduce pain. Gentle, controlled movements are applied to specific spinal segments to address restrictions and improve joint mechanics. Spinal mobilization typically involves a gradual application of force, while manipulation often involves a more forceful thrust.
The rationale is that restoring normal joint mechanics can decrease pain and improve function. Potential benefits include pain reduction, improved range of motion, and reduced muscle spasm. Potential risks include further injury, if not performed by a qualified professional.
Myofascial Release
Myofascial release techniques focus on the soft tissues surrounding the spine, such as muscles, tendons, and ligaments. These techniques aim to address muscle tension, reduce inflammation, and improve the overall flexibility of the surrounding tissues. The rationale is that releasing restrictions in these soft tissues can reduce pain and improve function. Potential benefits include pain reduction, improved range of motion, and reduced muscle spasm.
Potential risks include discomfort or soreness in the treated area.
Trigger Point Therapy
Trigger point therapy involves the identification and treatment of trigger points, which are hypersensitive areas within muscles that can refer pain to other areas of the body. The rationale is that addressing these trigger points can reduce pain and improve function. Potential benefits include pain reduction, improved muscle function, and reduced muscle spasm. Potential risks include discomfort or soreness in the treated area.
Table of Manual Therapy Techniques in Herniated Disc Care
| Technique | Rationale | Potential Benefits | Potential Risks |
|---|---|---|---|
| Spinal Mobilization/Manipulation | Restore joint mobility, reduce pain | Pain reduction, improved range of motion, reduced muscle spasm | Further injury, if not performed by a qualified professional |
| Myofascial Release | Address muscle tension, reduce inflammation | Pain reduction, improved range of motion, reduced muscle spasm | Discomfort or soreness in the treated area |
| Trigger Point Therapy | Address hypersensitive areas in muscles | Pain reduction, improved muscle function, reduced muscle spasm | Discomfort or soreness in the treated area |
Importance of Thorough Evaluation
A thorough evaluation is essential before implementing any manual therapy technique. This evaluation should include a comprehensive assessment of the patient’s medical history, physical examination, and imaging studies. The evaluation helps to determine the appropriate techniques and ensures that the treatment plan is safe and effective for the individual patient. A thorough evaluation helps in identifying the specific needs of the patient and allows for the selection of appropriate manual therapy techniques, thereby reducing the risk of complications.
Patient Education and Self-Management
Effective herniated disc management hinges significantly on patient education and active participation in their recovery. A well-informed patient is better equipped to understand their condition, adhere to treatment plans, and actively contribute to pain management and symptom reduction. This empowers them to take control of their health journey and promotes long-term well-being.Understanding the complexities of a herniated disc, and the importance of consistent effort in managing pain and symptoms, is crucial.
A proactive approach, guided by proper education, enables patients to effectively cope with daily activities, prevent exacerbations, and foster a positive outlook on their recovery.
Importance of Patient Education
Patient education is fundamental to successful herniated disc recovery. It fosters a deeper understanding of the condition, its potential impact on daily life, and the importance of adhering to treatment plans. Educated patients are more likely to actively participate in their care, leading to improved outcomes and a quicker return to normal activities.
Key Topics in Patient Education
Patient education should cover various aspects of the condition. This includes an explanation of the anatomy and physiology of the spine, the mechanisms that lead to a herniated disc, and the role of posture and body mechanics in pain management. Understanding the condition allows patients to make informed choices and take proactive steps toward recovery. Crucially, education should encompass available treatment options, including the roles of physical therapy, medication, and lifestyle modifications.
- Anatomy and Physiology of the Spine: Understanding the structure and function of the spine, including the role of intervertebral discs, is essential. This knowledge empowers patients to grasp the mechanics of a herniated disc and how it affects their bodies.
- Causes and Risk Factors: Identifying potential causes and risk factors for herniated discs allows patients to take preventive measures and understand the importance of maintaining good posture and healthy lifestyle choices.
- Symptoms and Diagnosis: Recognizing and understanding the common symptoms of a herniated disc, such as back pain, leg pain, numbness, or tingling, helps patients promptly seek medical attention and manage their condition effectively.
- Treatment Options: Detailed information about various treatment options, including physical therapy, medication, and surgery, should be provided. Understanding the advantages and disadvantages of each option will enable patients to make informed decisions.
- Pain Management Techniques: Teaching patients about effective pain management strategies, such as medication, heat/ice therapy, and relaxation techniques, empowers them to proactively manage their pain.
- Posture and Body Mechanics: Understanding proper posture and body mechanics is crucial for preventing future injuries and managing pain. This includes instruction on how to lift objects correctly, maintain good posture while sitting and standing, and perform daily activities safely.
Strategies for Home Pain Management
Implementing strategies for managing pain and symptoms at home is crucial for continued progress and preventing exacerbations. This includes practicing relaxation techniques, using heat or ice packs, and following a consistent exercise regimen. These techniques, when implemented correctly, can substantially reduce pain and discomfort.
- Heat/Ice Therapy: Applying heat or ice packs to the affected area can help reduce pain and inflammation. Heat promotes blood flow, while ice reduces swelling.
- Relaxation Techniques: Techniques such as deep breathing exercises, progressive muscle relaxation, and mindfulness can help manage stress and reduce pain perception.
- Gentle Exercise: Following a consistent exercise program, as prescribed by a physical therapist, can strengthen the back muscles, improve flexibility, and reduce pain.
- Proper Posture and Body Mechanics: Practicing proper posture and body mechanics during daily activities can prevent further injury and reduce pain.
Do’s and Don’ts for Herniated Discs
This table Artikels key guidelines for patients with herniated discs. Adhering to these recommendations can significantly contribute to pain management and recovery.
| Do’s | Don’ts |
|---|---|
| Engage in gentle exercise, as directed by a healthcare professional. | Lift heavy objects with improper form. |
| Maintain good posture while sitting, standing, and walking. | Perform strenuous activities without proper warm-up. |
| Use heat or ice packs as needed, following professional advice. | Sit for prolonged periods without movement breaks. |
| Practice relaxation techniques to manage stress and pain. | Ignore pain signals and push through discomfort. |
| Follow a healthy diet and maintain a healthy weight. | Engage in activities that aggravate pain. |
Self-Management Techniques for Posture and Pain Reduction
Specific self-management techniques can help improve posture and reduce pain. Practicing these techniques regularly can significantly impact the patient’s overall well-being and recovery.
- Postural Exercises: Incorporate exercises focusing on strengthening core muscles and improving spinal alignment. Examples include pelvic tilts, back extensions, and side bends.
- Stretching: Regular stretching can improve flexibility and range of motion in the spine, reducing stiffness and discomfort.
- Ergonomic Adjustments: Adjusting your workspace and daily activities to minimize strain on the spine can greatly contribute to pain management. Examples include using a supportive chair, maintaining proper posture while working at a desk, and arranging furniture to reduce twisting motions.
- Mindfulness and Stress Management: Chronic stress can exacerbate pain. Practicing mindfulness techniques, such as meditation and deep breathing, can help reduce stress and promote relaxation.
Equipment and Technology in Physical Therapy
Physical therapy for herniated discs utilizes a variety of equipment and technologies to assess the condition, tailor treatment plans, and enhance recovery. This diverse range of tools helps to optimize patient outcomes by providing targeted interventions and promoting active participation in the rehabilitation process. From simple, supportive devices to sophisticated imaging and diagnostic tools, the integration of technology and equipment plays a vital role in managing herniated discs effectively.
Common Equipment Used in Physical Therapy
Various tools are employed to address the specific needs of individuals with herniated discs. These tools aid in exercises, manual therapy, and patient education. This includes devices for strengthening, stretching, and pain management.
- Resistance Bands and Weights: These tools provide progressive resistance, enabling patients to safely and effectively build strength in the core, back, and surrounding muscles. By gradually increasing the resistance, patients can improve muscle endurance and stability, reducing the risk of further injury and promoting functional recovery.
- Therabands: These elastic bands offer variable resistance levels, making them ideal for a wide range of exercises, from gentle stretches to strengthening routines. The progressive resistance feature allows for tailoring the intensity of the exercise to the patient’s individual needs and progress.
- Balance Boards and Balls: These devices promote proprioception and balance, crucial for improving stability and reducing the risk of falls. This is particularly important for individuals with herniated discs who may have compromised core strength and balance. Patients can practice balance exercises on these tools to improve stability and coordination.
- Exercise Machines: Machines like stationary bikes, elliptical trainers, and rowing machines can be incorporated into a physical therapy program to improve cardiovascular health and overall fitness. These exercises help to strengthen the muscles supporting the spine, which can further reduce the load on the affected area.
Manual Therapy Techniques
Manual therapy involves hands-on techniques employed by physical therapists to address musculoskeletal issues. These techniques can include massage, mobilization, and manipulation.
- Massage Therapy: Soft tissue massage can help to alleviate muscle tension and pain, improve circulation, and promote relaxation. This can be beneficial for individuals experiencing muscle spasms and pain associated with a herniated disc.
- Mobilization and Manipulation: These techniques involve specific movements to restore joint mobility and reduce pain. Manual mobilization and manipulation can be effective in restoring spinal motion and reducing pain and stiffness related to the herniated disc.
Role of Technology in Assessment and Treatment
Technological advancements play an integral role in assessing and treating herniated discs. From imaging techniques to sophisticated diagnostic tools, technology allows for precise diagnosis and personalized treatment plans.
- Imaging Techniques: MRI (Magnetic Resonance Imaging) scans and CT (Computed Tomography) scans are commonly used to visualize the spine and identify the location and extent of a herniated disc. These images provide detailed information about the affected area, enabling therapists to develop a targeted treatment plan.
- Electromyography (EMG): This technique measures the electrical activity of muscles. EMG can be used to assess muscle strength and identify any nerve impingements contributing to pain or weakness. This helps in determining the extent of muscle involvement and the possible need for further interventions.
Assistive Devices for Daily Activities
Assistive devices can significantly improve the quality of life for individuals with herniated discs by facilitating daily activities.
- Back Supports and Braces: These devices provide additional support to the spine, reducing strain on the affected area and promoting better posture. Proper use of these devices can lessen the load on the spine, allowing for improved mobility and comfort.
- Adaptive Equipment: Assistive devices like raised toilet seats, grab bars, and long-handled utensils can make daily tasks easier, reducing stress on the back and promoting independence. These devices enable individuals to perform activities of daily living without exacerbating their condition.
Case Studies and Examples
Understanding the effectiveness of physical therapy for herniated discs requires looking at real-life patient journeys. These case studies highlight the individualized approach, demonstrating how tailored programs can lead to positive outcomes and recovery. Each example showcases the critical role of evaluation, treatment planning, and patient engagement in achieving successful results.A successful physical therapy program for a herniated disc isn’t a one-size-fits-all solution.
Individualized plans consider factors like the location and severity of the herniation, the patient’s overall health, lifestyle, and goals. This approach ensures the program is both safe and effective, promoting healing and restoring function.
Dealing with a herniated disc can be tough, but physical therapy is often a game-changer. Finding ways to manage the accompanying pain and discomfort is key, and sometimes that involves exploring different options. For example, some people find relief from anxiety by looking into alternative treatments like using CBD versus THC, which can be a complex topic, check out this article for more details on treating anxiety with CBD vs THC what to know.
Ultimately, though, a tailored physical therapy plan is crucial for a successful recovery from a herniated disc.
Initial Evaluation and Diagnosis
The initial evaluation is crucial in determining the best course of action. A thorough assessment involves a patient’s medical history, a physical examination, and diagnostic imaging (such as MRI or CT scans). This process allows therapists to identify the specific location and extent of the herniation, understand associated symptoms, and evaluate the patient’s overall physical condition. The evaluation also assesses functional limitations, pain levels, and mobility restrictions.
The therapist carefully considers the patient’s current ability to perform daily activities, such as walking, lifting, and sitting. This detailed analysis forms the basis for creating a personalized treatment plan.
Physical Therapy Program Tailored to Patient Needs
A tailored physical therapy program addresses the specific needs of each patient. This personalized approach focuses on pain management, improving range of motion, and strengthening the core muscles. The program typically includes a combination of exercises, manual therapy techniques, and patient education. For example, exercises might include specific stretches to alleviate pressure on the affected nerves, strengthening exercises to stabilize the spine, and postural training to improve body mechanics.
Manual therapy techniques, such as soft tissue mobilization and spinal manipulation, can help reduce pain and improve mobility.
Progress and Outcomes of Physical Therapy
Progress in physical therapy is often gradual and varies depending on the individual. Measurable improvements can include decreased pain intensity, increased range of motion, and improved functional ability. For instance, a patient might experience a reduction in pain levels after several sessions, allowing them to perform daily tasks with less discomfort. Increased flexibility and strength may also be observed as the program progresses.
Patients should actively participate in their treatment plan to achieve the best possible outcomes.
Importance of Individualized Physical Therapy Programs
Individualized physical therapy programs are essential for optimal results. A program tailored to an individual’s specific needs, considering their medical history, current condition, and goals, ensures a safe and effective treatment plan. A generic approach may not address the underlying causes of the herniated disc, potentially leading to suboptimal outcomes or even exacerbating the condition. The program should incorporate patient education, focusing on proper body mechanics and lifestyle modifications, to prevent future occurrences.
For example, a patient with a sedentary job might benefit from specific exercises and education on ergonomic adjustments to reduce strain on the spine.
Potential Complications and Considerations: Herniated Disc Physical Therapy
Navigating the path to recovery from a herniated disc often involves a delicate balance between aggressive treatment and careful consideration of potential risks. While physical therapy is generally safe and effective, understanding potential complications and knowing when to adjust the treatment plan is crucial for optimal outcomes. This section delves into the possible hurdles and strategies for minimizing them.Careful monitoring and proactive communication with your healthcare provider are paramount.
So, I’ve been doing herniated disc physical therapy, and it’s been surprisingly helpful. One thing I’ve noticed though, is I’m sweating way more than usual. Could this be related to the physical exertion? Maybe it’s something else entirely, like why do I sweat so much ? Either way, I’m hoping the therapy continues to ease the pain and discomfort, and I can get back to my normal routine.
Hopefully, addressing the increased sweating will be part of the overall solution.
Early identification of any adverse effects allows for timely intervention, preventing potential long-term problems.
Herniated disc physical therapy is crucial for regaining strength and mobility. However, underlying health conditions like obesity can significantly impact recovery. This is because obesity is linked to a variety of health issues, including increased cancer risk, why does obesity increase cancer risk which can indirectly affect the effectiveness of physical therapy. Ultimately, addressing any contributing factors like weight management, alongside the physical therapy, is key for optimal results.
Potential Adverse Reactions to Treatment
Physical therapy, while beneficial, can sometimes lead to temporary discomfort. Muscle soreness, stiffness, and mild pain are common, but severe or persistent pain warrants immediate attention. Uncommon but possible adverse reactions include increased inflammation, nerve irritation, or exacerbating existing symptoms.
Recognizing Signs of Worsening Condition
A key aspect of successful physical therapy is recognizing when symptoms worsen. Monitoring for changes in pain intensity, location, or duration is essential. Changes in neurological function, such as numbness, tingling, or weakness in the limbs, should be reported immediately. This proactive approach ensures that the therapy remains effective and avoids further complications.
When to Seek Additional Medical Advice
Persistent or worsening pain, new neurological symptoms, or a lack of improvement after a reasonable period of time necessitates a visit to your physician. Additional diagnostic testing or a change in treatment plan may be necessary. Your healthcare provider can evaluate the situation and determine the appropriate course of action.
Importance of Monitoring and Adapting the Treatment Plan
Physical therapy is not a one-size-fits-all approach. Regular evaluation and adjustments to the treatment plan are essential. The therapist should assess the patient’s response to exercises, manual therapy, and overall progress. This adaptive approach ensures that the treatment remains effective and safe. A patient’s body responds differently to various treatments.
This adaptability ensures the treatment is tailored to the patient’s individual needs.
Surgical Intervention as a Last Resort
Surgery for a herniated disc is a significant decision and is generally considered a last resort. Physical therapy plays a vital role in helping patients avoid surgery. However, if conservative treatments fail to provide significant relief or if neurological deficits worsen, surgical intervention may be necessary. Your healthcare provider will evaluate the situation and discuss the benefits and risks of surgery with you.
The decision to undergo surgery is ultimately a personal one, made after careful consideration of the pros and cons.
Prevention and Risk Reduction
Preventing a herniated disc involves proactive strategies that focus on maintaining spinal health and reducing the risk factors. By understanding the contributing elements and implementing preventative measures, individuals can significantly lower their chances of experiencing this debilitating condition. This section explores key strategies for maintaining a healthy spine and avoiding herniated discs.Effective strategies for preventing herniated discs are crucial for long-term spinal health.
These strategies emphasize the importance of good posture, appropriate body mechanics, and proactive core strengthening. Recognizing and addressing underlying risk factors further enhances preventative measures.
Maintaining Good Posture and Body Mechanics
Proper posture is essential for distributing weight evenly across the spine, minimizing stress on the discs. Maintaining an upright posture throughout the day, whether sitting, standing, or walking, significantly reduces strain on the spinal structures. Avoiding prolonged periods of slouching or awkward postures is crucial. Proper body mechanics, encompassing the coordinated movements of the spine, limbs, and core muscles, play a significant role in minimizing the risk of injury.
Consistent practice of good posture and body mechanics in daily activities can prevent disc injuries.
Appropriate Lifting Techniques
Safe lifting practices are critical in preventing herniated discs. When lifting objects, it’s essential to bend at the knees and hips, keeping the back straight. Avoid twisting while lifting, and maintain a neutral spine position. Proper lifting techniques involve using the leg muscles to lift rather than the back muscles. Proper lifting technique is paramount to avoid straining the spine and reducing the risk of herniated discs.
For heavy objects, consider using mechanical aids like lifting straps or dollies.
Core Strengthening Exercises
Core strengthening exercises are fundamental in supporting the spine and maintaining stability. Strong core muscles act as a natural support system for the spine, distributing forces and reducing stress on the discs. Exercises targeting abdominal, back, and pelvic floor muscles are crucial for spinal health. Core strengthening exercises, when integrated into a regular routine, contribute significantly to the prevention of herniated discs.
These exercises include planks, crunches, and bridges.
Recognizing and Addressing Underlying Conditions
Certain underlying conditions can increase the risk of herniated discs. Conditions like obesity, osteoporosis, and certain medical conditions can negatively affect spinal health and increase the likelihood of herniated discs. It is essential to consult a healthcare professional for diagnosis and management of any underlying conditions that might increase risk. Addressing any pre-existing conditions that may contribute to a herniated disc is crucial in preventing future issues.
Examples of Prevention
“A consistent workout routine, incorporating core strengthening exercises and appropriate lifting techniques, can drastically reduce the likelihood of a herniated disc.”
- Regular exercise, including activities like swimming, walking, or yoga, can help maintain spinal flexibility and strength.
- Maintaining a healthy weight through a balanced diet and regular exercise can reduce stress on the spine.
- Avoiding prolonged periods of sitting or standing in awkward positions can prevent muscle imbalances and reduce the risk of injury.
Outcome Summary
In conclusion, herniated disc physical therapy is a multi-faceted approach to managing this condition. It involves a thorough understanding of the condition, personalized treatment plans, and active patient participation. By combining various therapies, exercises, and patient education, individuals can significantly improve their quality of life and recover from a herniated disc. Remember, consistency and adherence to the treatment plan are key to achieving positive outcomes.
This guide provided a solid foundation for understanding the complexities of this condition and the important role physical therapy plays in recovery.