Does iron cause constipation? This exploration delves into the complex relationship between iron intake and digestive health. Understanding the role of iron in the body, the various forms of iron, and their absorption processes is crucial to comprehending this connection. We’ll also examine how individual differences, diet, and medications might influence this relationship.
Iron, an essential mineral for red blood cell production, comes in different forms, each absorbed differently. Heme iron, found in animal products, is absorbed more readily than non-heme iron, present in plant-based foods. The digestive system plays a vital role in this absorption process, impacting how much iron our bodies utilize. This journey will uncover potential links between iron and constipation, examining factors that might influence the connection, and providing practical tips for managing iron intake to maintain healthy bowel movements.
Introduction to Iron and Digestion
Iron is an essential mineral for human health, playing a crucial role in oxygen transport throughout the body. It’s a component of hemoglobin, the protein in red blood cells that carries oxygen, and myoglobin, the protein that stores oxygen in muscles. Without sufficient iron, the body struggles to deliver oxygen effectively, leading to fatigue, weakness, and various other health problems.Different forms of iron are absorbed differently in the body.
Understanding these forms and their absorption pathways is key to comprehending how iron impacts digestion and overall health. The digestive system plays a vital role in this process, breaking down food and absorbing the necessary nutrients, including iron.
Iron Forms and Absorption
Iron exists in two primary forms: heme iron and non-heme iron. Heme iron is bound to a protein called heme, primarily found in animal products like red meat, poultry, and fish. Non-heme iron is found in plant-based foods such as leafy greens, beans, and lentils. The absorption mechanisms for these two forms differ significantly.
- Heme iron is absorbed more efficiently than non-heme iron. The body directly absorbs heme iron from the intestines, bypassing the need for further breakdown. This process is more straightforward and allows for quicker assimilation into the bloodstream.
- Non-heme iron absorption is influenced by several factors, including the presence of other nutrients and compounds in the diet. For instance, vitamin C enhances non-heme iron absorption, while phytates and polyphenols (found in certain plant foods) can hinder it.
The Digestive Process
The digestive system is a complex network of organs working together to break down food and absorb nutrients. The process begins in the mouth, where food is chewed and mixed with saliva. Then, it travels down the esophagus to the stomach, where it’s further broken down by stomach acid and enzymes. From the stomach, the partially digested food moves to the small intestine, the primary site for nutrient absorption.
The small intestine contains specialized cells that absorb iron, along with other essential nutrients, into the bloodstream. The large intestine absorbs water and electrolytes before the waste products are eliminated.
- The mouth mechanically breaks down food through chewing and mixes it with saliva. Saliva contains enzymes that begin the initial breakdown of carbohydrates.
- The esophagus transports food from the mouth to the stomach via peristalsis.
- The stomach produces gastric juices, including hydrochloric acid, which denatures proteins and activates enzymes.
- The small intestine is the primary site for nutrient absorption. The duodenum, jejunum, and ileum each play specific roles in this process.
- The large intestine absorbs water and electrolytes before waste is eliminated.
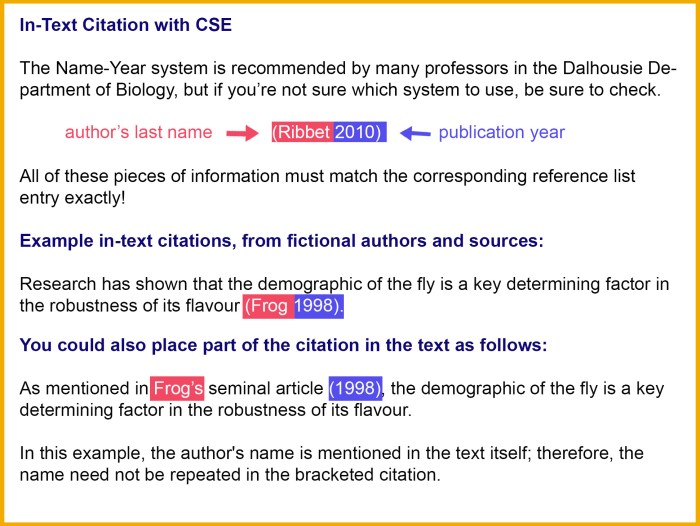
Comparison of Heme and Non-Heme Iron Absorption
The following table illustrates the differing absorption rates of heme and non-heme iron.
| Iron Type | Absorption Rate (%) | Factors Affecting Absorption |
|---|---|---|
| Heme Iron | 15-35% | Generally well-absorbed; not significantly influenced by other dietary components. |
| Non-Heme Iron | 2-20% | Absorption is influenced by vitamin C (enhances), phytates and polyphenols (inhibit). |
Absorption rates can vary based on individual needs and dietary factors.
Iron and Constipation
Iron, a crucial component for red blood cell production, is often taken as a supplement, especially for those with iron deficiency. However, this essential nutrient can sometimes have an unexpected side effect: constipation. Understanding the potential mechanisms behind this connection is vital for those looking to optimize their iron intake while maintaining healthy bowel habits.Iron supplements and high iron intake can potentially impact gut motility and the gut microbiome, leading to constipation.
This impact can vary depending on the type of iron supplement and individual factors. Examining these interactions can help individuals manage potential side effects and maintain overall digestive health.
Potential Mechanisms of Iron-Induced Constipation
Iron’s interaction with the digestive system can contribute to constipation in several ways. One key mechanism involves the impact on gut motility. Iron, particularly in its ionic form, can potentially alter the normal contractions of the intestines, leading to slower transit time and a harder stool consistency. This slower transit time allows more water to be absorbed from the stool, making it harder and more difficult to pass.
While iron is essential for good health, some wonder if it can contribute to constipation. It’s a common concern, but the truth is often more nuanced than a simple yes or no. For example, consider how swimming can boost your metabolism and aid in weight loss. Swimming for Weight Loss Your Aquatic Journey is a fantastic way to incorporate exercise into your daily routine and support overall well-being.
Ultimately, whether or not iron causes constipation depends on individual factors and dietary habits.
Interaction with Gut Motility
Iron absorption can sometimes affect the movement of food through the digestive tract. Certain forms of iron, like ferrous iron, can bind to intestinal lining components and slow down the natural peristaltic contractions that propel stool through the colon. This effect can manifest as decreased frequency of bowel movements and potentially harder stools. For example, individuals experiencing iron deficiency and taking supplements may notice a change in bowel habits, which may be related to iron’s effect on gut motility.
Connection to Gut Microbiota
The gut microbiota plays a vital role in digestion and overall health. Changes in gut motility and the environment within the intestines, which can occur with high iron intake, may negatively impact the delicate balance of gut bacteria. This disturbance could lead to a less efficient breakdown of food and reduced regularity of bowel movements. Some studies suggest a potential link between alterations in the gut microbiota and constipation.
Negative Effects of High Iron Intake on Bowel Health
High iron intake, whether from supplements or dietary sources, can have negative consequences on bowel health. Excess iron can potentially irritate the intestinal lining, leading to discomfort, bloating, and abdominal cramps. In some cases, it may even exacerbate existing digestive issues, particularly in individuals prone to digestive sensitivities.
Impact of Different Iron Supplements on Constipation
| Type of Iron Supplement | Potential Impact on Constipation |
|---|---|
| Ferrous Sulfate | Generally considered to have a higher potential for constipation compared to other forms. |
| Ferrous Fumarate | May have a slightly lower risk of constipation than ferrous sulfate. |
| Ferric Citrate | Often associated with a lower incidence of constipation. |
| Iron Polymaltose | Potential for less constipation than ferrous sulfate. |
| Iron Sucrose Phosphate | May have a lower risk of constipation compared to ferrous sulfate. |
Note: Individual responses to iron supplements vary greatly. Consult a healthcare professional for personalized advice.
Factors Influencing Iron-Constipation Relationship
Iron deficiency and constipation often go hand-in-hand, but the connection isn’t always straightforward. Many factors can influence how iron intake affects bowel movements, and understanding these nuances is key to managing both conditions effectively. This section delves into the interplay between individual differences, dietary choices, medications, and the symptoms associated with constipation in relation to iron intake.Individual variations in age, gender, and underlying health conditions significantly impact the iron-constipation relationship.
For instance, pregnancy often leads to iron supplementation, but this can also increase the risk of constipation due to the increased iron absorption and hormonal changes. Similarly, certain gastrointestinal conditions can exacerbate constipation symptoms, irrespective of iron intake.
Age-Related Variations
Children and adolescents may experience constipation due to various factors, including dietary habits and growth spurts. Iron supplementation in children might contribute to constipation, particularly if not accompanied by adequate fiber intake. In the elderly, constipation is more prevalent due to decreased muscle tone and motility in the digestive tract, and iron supplements can further complicate this issue.
Furthermore, chronic health conditions like irritable bowel syndrome (IBS) can affect both iron absorption and bowel movements.
Gender-Related Differences
Hormonal fluctuations throughout a woman’s life cycle can influence bowel habits. The menstrual cycle, pregnancy, and menopause are examples where hormonal shifts can affect both iron levels and digestive processes. Similarly, men might experience constipation related to iron intake, but the specific interplay of factors may differ.
Impact of Underlying Health Conditions
Chronic conditions such as diabetes, hypothyroidism, and certain neurological disorders can lead to changes in gut motility, potentially resulting in constipation. These conditions can also impact iron absorption and utilization, further complicating the iron-constipation relationship. It is essential to consider any underlying health issues when addressing iron supplementation and bowel regularity.
Dietary Factors Impacting Iron Absorption and Bowel Health
Dietary choices play a pivotal role in both iron absorption and bowel regularity. Fiber is essential for maintaining healthy bowel movements. Insufficient fiber intake can lead to hard stools and constipation, while adequate fiber intake can soften stools and promote regular bowel movements.
Hey everyone! So, I’ve been doing some digging into whether iron supplements cause constipation, and it’s definitely a common complaint. While iron is essential for our health, it can sometimes lead to digestive issues. Fortunately, a deeper understanding of the complexities of iron and its potential effects on digestion can be found in resources like RU486 the Abortion Pill A Comprehensive Guide.
This comprehensive guide delves into the specifics of iron-related digestive problems and how to manage them. Ultimately, the answer to whether iron causes constipation depends on individual factors and potential interactions with other medications or health conditions.
Dietary Factors and Their Influence on Iron Absorption and Gut Health
| Dietary Factor | Influence on Iron Absorption | Influence on Gut Health |
|---|---|---|
| High Fiber Intake | Can slightly reduce iron absorption, but not significantly | Promotes healthy bowel movements, softens stools |
| Vitamin C | Enhances iron absorption | May not directly affect gut health, but supports overall health |
| Phytates (in whole grains, legumes) | Reduce iron absorption | Can contribute to a healthy gut microbiome if consumed in moderation |
| Calcium | Reduces iron absorption | May not directly affect gut health, but plays a role in overall health |
| Red Meat | Enhances iron absorption | Can contribute to gut health depending on preparation methods |
Medications and Their Potential Impact
Certain medications can impact iron absorption and bowel habits. Antacids, for instance, can reduce iron absorption by binding to iron. Similarly, some antibiotics can disrupt the gut microbiome, potentially affecting bowel regularity. It’s crucial to discuss any medications with a healthcare professional before starting iron supplements.
Iron Deficiency and Constipation: Does Iron Cause Constipation
Iron and constipation can sometimes be intertwined, but they are distinct conditions. Understanding the differences between iron deficiency and constipation is crucial for accurate diagnosis and effective treatment. Confusion between the two can lead to misdiagnosis and potentially ineffective interventions. This section will differentiate between iron deficiency and constipation, explaining how each affects bowel movements and the symptoms associated with each condition.
Distinguishing Iron Deficiency from Constipation
Iron deficiency and constipation, while sometimes presenting overlapping symptoms, are fundamentally different conditions. Iron deficiency arises from a lack of iron in the body, hindering the production of hemoglobin, a crucial component of red blood cells. Constipation, on the other hand, is characterized by infrequent bowel movements or difficulty passing stools. Understanding the underlying causes of each condition is vital for appropriate treatment.
Iron Deficiency Anemia Symptoms
Iron deficiency anemia, a condition resulting from insufficient iron, manifests with a range of symptoms. These symptoms can vary in severity and are often subtle in the early stages. Recognizing these symptoms is crucial for timely diagnosis and treatment. Symptoms often include fatigue, weakness, shortness of breath, pale skin, and headaches. In more severe cases, individuals may experience dizziness, chest pain, or palpitations.
These symptoms are related to the reduced oxygen-carrying capacity of the blood due to insufficient hemoglobin.
Constipation Symptoms
Constipation, a common digestive issue, presents with several telltale signs. These signs can be quite varied and depend on the severity and underlying cause of the condition. Symptoms frequently include infrequent bowel movements, hard or lumpy stools, straining during bowel movements, a feeling of incomplete evacuation, and abdominal discomfort.
Comparison of Iron Deficiency and Constipation Symptoms
| Characteristic | Iron Deficiency | Constipation |
|---|---|---|
| Frequency of Bowel Movements | Typically not directly affected. Bowel movements might be normal or slightly altered in some cases. | Infrequent bowel movements, less than three times a week. |
| Stool Consistency | Not typically directly affected. | Hard, dry, and difficult to pass stools. |
| Other Symptoms | Fatigue, weakness, shortness of breath, pale skin, headaches, dizziness, chest pain, palpitations. | Straining during bowel movements, abdominal discomfort, feeling of incomplete evacuation. |
| Underlying Cause | Insufficient iron intake, malabsorption, blood loss. | Inadequate fiber intake, dehydration, certain medications, lack of physical activity, underlying medical conditions. |
Managing Iron Intake and Bowel Health
Iron is crucial for many bodily functions, but its absorption and impact on digestion can sometimes lead to constipation. A balanced approach to iron intake, combined with strategies to promote healthy bowel movements, is key to avoiding this issue. This section will explore practical ways to manage iron intake while supporting optimal digestive health.A healthy digestive system is essential for efficient iron absorption.
By understanding the relationship between iron and bowel movements, we can develop personalized strategies to maintain both iron levels and digestive regularity.
Dietary Strategies for Iron Absorption and Bowel Health
Proper diet plays a vital role in ensuring both adequate iron intake and healthy bowel movements. Consuming iron-rich foods alongside foods that promote digestion can significantly improve overall health.
- Prioritize Iron-Rich Foods with Fiber: Pairing iron-rich foods with high-fiber options enhances iron absorption and promotes regular bowel movements. Leafy greens, beans, lentils, and whole grains are excellent examples. The fiber adds bulk to stool, facilitating smoother passage through the digestive tract.
- Include Iron-Rich Foods with Vitamin C: Vitamin C significantly improves iron absorption. Consume iron-rich foods alongside citrus fruits, berries, or other vitamin C-rich foods. This combination boosts iron uptake, making the iron more readily available to the body.
- Choose Iron-Rich Foods in Combination with Other Nutrients: Certain foods can inhibit iron absorption. For example, calcium-rich foods, when consumed alongside iron-rich foods, can reduce iron absorption. Careful consideration of food pairings can optimize iron intake while maintaining a balanced diet.
Dietary Strategies for Improved Bowel Health
A diet rich in fiber is crucial for maintaining bowel regularity. Fiber adds bulk to stool, which helps prevent constipation and promotes regular bowel movements.
- High-Fiber Foods for Digestive Support: Incorporate a variety of high-fiber foods into your diet. Examples include fruits (apples, pears, berries), vegetables (broccoli, carrots, spinach), whole grains (brown rice, quinoa, oats), and legumes (beans, lentils). These foods provide the necessary bulk and nutrients for a healthy digestive system.
- Hydration for Bowel Regularity: Adequate hydration is essential for maintaining bowel regularity. Water helps soften stool and facilitates its passage through the digestive tract. Aim for at least 8 glasses of water per day, and adjust based on activity levels and climate.
Exercise and Bowel Health
Regular physical activity can significantly impact bowel health. Exercise promotes healthy digestion and can prevent constipation.
- Importance of Regular Exercise: Incorporate regular exercise into your daily routine. Even moderate-intensity exercise, such as brisk walking, can stimulate bowel movements and promote overall digestive health. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Summary of Dietary Recommendations
| Dietary Recommendation | Description |
|---|---|
| Iron-Rich Foods with Fiber | Combine iron-rich foods (e.g., lentils, leafy greens) with high-fiber foods (e.g., whole grains, fruits) to enhance iron absorption and promote regularity. |
| Iron-Rich Foods with Vitamin C | Consume iron-rich foods alongside vitamin C-rich foods (e.g., citrus fruits) to improve iron absorption. |
| Hydration | Maintain adequate hydration by drinking plenty of water throughout the day to soften stool and aid in digestion. |
| High-Fiber Diet | Include a variety of high-fiber foods (e.g., fruits, vegetables, whole grains) in your diet to promote regularity. |
| Regular Exercise | Engage in regular physical activity to stimulate bowel movements and support overall digestive health. |
Iron Supplements and Constipation: Considerations
Iron supplements are a common way to address iron deficiency, but they can sometimes lead to digestive issues, particularly constipation. Understanding the potential side effects and how to choose a less constipating formulation is crucial for managing your iron intake effectively. This section dives into the specifics of iron supplements and constipation, providing actionable insights to help you navigate this potential complication.Iron supplements, while beneficial for iron deficiency, can interact with your digestive system, sometimes resulting in constipation.
This interaction is a common side effect and is often dose-dependent. Understanding the different formulations and potential risks associated with each type can help you make informed choices and minimize discomfort.
Potential Side Effects of Iron Supplements
Iron supplements, although crucial for iron replenishment, can come with a range of potential side effects. These often manifest as digestive issues, with constipation being a prominent concern. Other common side effects include nausea, vomiting, abdominal cramps, and heartburn. The severity of these side effects can vary significantly depending on the individual, dosage, and specific formulation.
Specific Iron Supplement Formulations and Constipation
Different iron supplement formulations can have varying effects on the digestive system. Ferrous sulfate, a common type, is often associated with constipation due to its tendency to bind water in the intestines. This binding effect can slow down bowel movements and contribute to digestive discomfort. Other forms, such as ferrous fumarate and ferrous gluconate, might be slightly less constipating, but individual responses can differ.
Selecting Less Constipating Iron Supplements
Several strategies can help minimize the likelihood of constipation when taking iron supplements. Choosing a formulation with a lower elemental iron content can be beneficial, as higher doses are more likely to lead to digestive issues. Taking the supplement with food can also help mitigate potential stomach upset. Furthermore, staying adequately hydrated and including fiber-rich foods in your diet can contribute to better bowel health overall.
Spreading the intake throughout the day may also help manage the amount of iron absorbed at once.
Importance of Consulting a Healthcare Professional
Before starting any iron supplementation regimen, consulting a healthcare professional is paramount. A healthcare provider can assess your individual needs, determine the appropriate dosage and formulation, and provide guidance on managing potential side effects, including constipation. They can also help rule out other underlying health conditions that may be contributing to iron deficiency. This proactive approach is vital for ensuring safe and effective iron supplementation.
Table of Iron Supplement Types and Potential Constipation Effects
| Iron Supplement Type | Potential Constipation Effects |
|---|---|
| Ferrous Sulfate | Generally higher risk of constipation due to water binding. |
| Ferrous Fumarate | Potentially less constipating than ferrous sulfate, but individual responses vary. |
| Ferrous Gluconate | Often considered less constipating than ferrous sulfate, but still possible. |
| Iron Bisglycinate | Potentially better absorbed, and may have a lower risk of gastrointestinal side effects, including constipation. |
Illustrative Examples
Iron, a crucial mineral for numerous bodily functions, plays a vital role in oxygen transport and red blood cell production. However, the relationship between iron intake and bowel health is complex, and its impact can vary significantly from person to person. Understanding this relationship requires careful consideration of various factors.The effects of iron-rich diets on bowel health can range from mild discomfort to more significant issues like constipation.
Dietary changes, particularly those involving significant increases in iron intake, should always be approached cautiously and in consultation with a healthcare professional. This is essential to ensure the changes are safe and beneficial, preventing potential adverse health consequences.
While we’re on the topic of digestive health, I wanted to touch on whether iron supplements can lead to constipation. It’s a common concern, and often overlooked. Luckily, there’s a wealth of information available online about managing skin issues, like learning about different skin tag removal methods and various skin tag patches, which can be helpful for understanding the importance of digestive health.
For example, check out What are Skin Tag Patches? A Comprehensive Guide for a deeper dive into skin care. Ultimately, though, iron supplements can sometimes cause constipation, so be mindful of your body’s signals and adjust your diet accordingly.
Potential Iron-Rich Diets and Bowel Health
Different iron-rich foods can have varying effects on bowel health. For instance, red meat, a good source of heme iron, is often associated with a lower incidence of constipation, but this depends on the overall diet and individual factors. Conversely, plant-based iron sources like spinach, while beneficial, may lead to digestive discomfort in some individuals if not consumed in moderation and balanced with sufficient fiber.
- A diet rich in red meat, poultry, and fish, along with adequate fiber, can often support healthy bowel movements. The heme iron in these foods is well-absorbed, contributing to healthy red blood cell production, but it is essential to maintain a balanced diet, including plenty of fruits and vegetables to ensure sufficient fiber intake. These foods can aid in maintaining healthy digestion.
- Diets rich in iron-fortified cereals and legumes can provide sufficient iron but may also require a careful balance with other foods to ensure adequate fiber. Iron fortification can contribute to preventing iron deficiency, but it’s crucial to be mindful of the fiber content and overall dietary composition to support healthy digestion.
- A diet heavily reliant on iron-rich vegetables, such as spinach and kale, may lead to digestive issues for some individuals if not accompanied by sufficient fiber intake. The high iron content, combined with low fiber, can make bowel movements harder, potentially leading to constipation.
Importance of Consulting a Doctor
Dietary changes, particularly those involving a significant increase or decrease in iron intake, should always be discussed with a healthcare professional. Individual needs and sensitivities vary, and a doctor can assess an individual’s specific circumstances to determine the appropriate dietary approach and monitor for potential side effects. This is crucial for maintaining overall health and preventing complications.
Dietary Interactions with Iron Supplements
Iron supplements can interact with certain foods, affecting their absorption. For example, calcium-rich foods can hinder the absorption of non-heme iron. Conversely, vitamin C can enhance the absorption of iron. A doctor can advise on optimizing dietary choices to maximize the effectiveness of iron supplements while minimizing potential side effects.
High-Iron Foods vs. Low-Fiber Foods
| High-Iron Foods | Low-Fiber Foods |
|---|---|
| Red meat | Processed meats |
| Spinach | White bread |
| Legumes | Refined cereals |
| Fortified cereals | Sugary snacks |
| Dried fruits | Highly processed foods |
Case Study: A Potential Link
A 35-year-old female patient, previously diagnosed with mild iron deficiency anemia, began taking iron supplements. She also significantly increased her consumption of iron-rich leafy greens like spinach. Despite taking the supplements, she experienced worsening constipation. She reported consuming minimal fiber-rich foods. This case highlights the potential link between high iron intake, low fiber, and constipation.
The patient’s doctor recommended increasing her fiber intake through fruits, vegetables, and whole grains. The doctor also adjusted the iron supplement dosage to a lower amount, considering the patient’s specific needs and digestive sensitivities.
Further Research Considerations
Unraveling the intricate connection between iron and constipation requires a deeper dive into the underlying mechanisms. While current research provides valuable insights, gaps remain in our understanding of this complex interplay. Further investigation is crucial to refine our knowledge and develop more effective strategies for managing both iron deficiency and related digestive issues.
Interplay of Iron Absorption and Gut Motility
Understanding the precise mechanisms by which iron absorption affects gut motility is a critical area for future research. Studies should explore the specific receptors and signaling pathways involved in the iron-induced changes in gut muscle contractions. This knowledge will allow for a more targeted approach to managing iron-related constipation, possibly identifying specific factors contributing to impaired motility in certain individuals.
Furthermore, investigating the role of intestinal microbiota in this process is important, given the microbiota’s influence on digestion and overall gut health.
Individual Variability in Response to Iron, Does iron cause constipation
Significant individual variability exists in how individuals respond to iron supplementation. Factors such as genetic predisposition, dietary habits, and overall health status likely influence the impact of iron on bowel function. Future research should focus on identifying specific genetic markers or biomarkers that predict an individual’s susceptibility to iron-induced constipation. This personalized approach will allow for tailored recommendations regarding iron intake and potential preventative measures.
Long-Term Effects of Iron Intake on Bowel Health
The long-term effects of iron intake on bowel health require further investigation. Studies should evaluate the cumulative impact of iron consumption, both from dietary sources and supplements, on the structural and functional integrity of the gastrointestinal tract over time. Understanding potential long-term consequences will help refine dietary guidelines and supplement recommendations, especially for individuals with pre-existing digestive conditions or those at risk of developing them.
Potential interactions with other nutrients and medications also deserve careful examination.
Role of Specific Iron Forms
Different forms of iron (e.g., ferrous sulfate, ferrous fumarate) have varying degrees of absorption and bioavailability. Future research should compare the effects of different iron formulations on gut motility and bowel function. This will provide more specific guidance on choosing the most suitable iron supplement for individuals experiencing constipation. For example, if one form is consistently associated with fewer digestive issues, it would significantly improve treatment strategies.
Impact of Iron Deficiency on Gut Microbiome
The relationship between iron deficiency, gut microbiome composition, and constipation needs further exploration. Studies should investigate whether iron deficiency alters the balance of beneficial and harmful bacteria in the gut, potentially impacting bowel regularity. This will help understand if restoring optimal gut microbial balance could help manage iron-related constipation. Detailed analyses of stool samples could reveal specific changes in microbial populations.
Last Word
In conclusion, the relationship between iron and constipation is multifaceted. While iron is essential, certain forms and intake levels can potentially contribute to digestive issues. Individual factors, diet, and medications play a crucial role. Prioritizing a balanced diet rich in fiber, staying hydrated, and consulting a healthcare professional before starting iron supplements are key steps in maintaining both iron levels and digestive health.
Further research continues to shed light on this intricate connection, allowing us to better understand and manage these interactions.