What is levator ani syndrome? This condition affects the pelvic floor muscles, specifically the levator ani, causing a range of symptoms and impacting daily life. Understanding the anatomy, potential causes, and available treatment options is key to managing this often-overlooked health issue. This comprehensive guide delves into the intricacies of levator ani syndrome, equipping you with essential knowledge to navigate this complex area of pelvic health.
The levator ani muscles are crucial for pelvic floor function, supporting the pelvic organs and facilitating continence. When these muscles are weakened, damaged, or strained, a variety of symptoms can arise, leading to discomfort and impacting overall well-being. Understanding the underlying mechanisms behind levator ani syndrome is vital to effective management and treatment.
Introduction to Levator Ani Syndrome
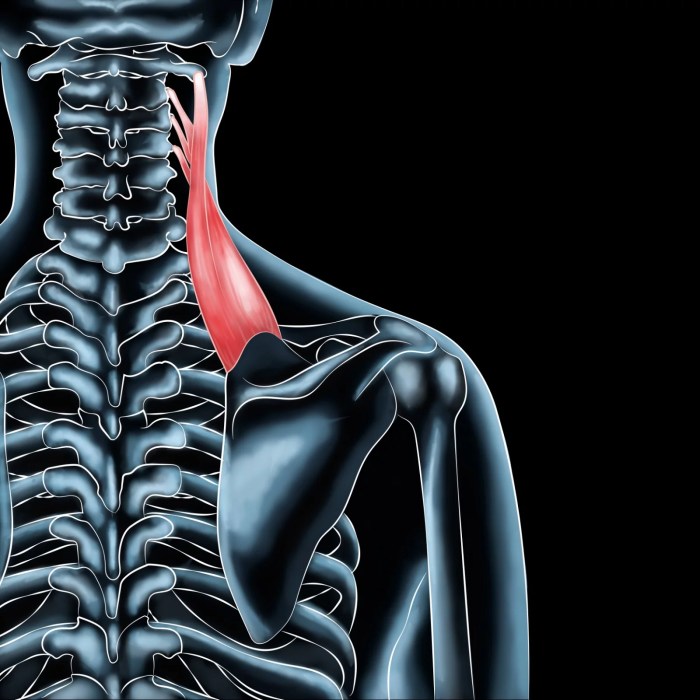
Levator ani syndrome (LAS) is a condition characterized by pain and discomfort in the pelvic region, often stemming from the levator ani muscles. These muscles, a crucial component of the pelvic floor, play a vital role in supporting the pelvic organs and controlling bowel and bladder function. Understanding the anatomy and potential causes of LAS is key to recognizing and addressing this condition effectively.The levator ani muscles are a group of muscles located within the pelvic floor.
They form a sling-like structure that supports the pelvic organs, including the bladder, uterus (in females), and rectum. These muscles are essential for maintaining continence, facilitating bowel and bladder emptying, and supporting the weight of the abdominal organs. Dysfunction or injury to these muscles can lead to various symptoms and discomfort.
Anatomy of the Levator Ani Muscles
The levator ani muscles are comprised of three main parts: the pubococcygeus, iliococcygeus, and puborectalis. These muscles work synergistically to create a dynamic support system for the pelvic organs. The pubococcygeus muscle is responsible for supporting the urethra and vagina, while the iliococcygeus muscle contributes to the support of the rectum. The puborectalis muscle forms a sling around the rectum, aiding in continence.
Proper coordination of these muscles is critical for optimal pelvic floor function.
Symptoms of Levator Ani Syndrome
Common symptoms of Levator Ani Syndrome include chronic pelvic pain, pain during sexual activity, and pain during bowel movements. Other symptoms can range from urinary incontinence or urgency to a sensation of heaviness or pressure in the pelvis. These symptoms can vary in intensity and duration, and their presence can indicate underlying dysfunction of the levator ani muscles.
Levator ani syndrome is a frustrating condition where the muscles supporting your pelvic floor become overly tight or strained, often leading to pain and discomfort. Before you use stool softeners, it’s important to understand if they’re even the right solution for your specific issue. Consider exploring the factors involved in your particular situation by visiting this resource on before you use stool softeners This knowledge can help you make informed decisions about treatment options and, ultimately, better manage levator ani syndrome.
Potential Causes of Levator Ani Syndrome
Understanding the potential causes of Levator Ani Syndrome is essential for appropriate diagnosis and treatment. A multifaceted approach is often required to identify the specific cause and develop a tailored management plan.
So, you’re learning about levator ani syndrome? It’s a condition where the muscles supporting your pelvic floor aren’t functioning correctly. This can lead to a whole host of issues, like incontinence and pain. Sometimes, similar issues can be related to breathing problems, and understanding the differences between CPAP and BiPAP machines can be really helpful in managing these types of conditions.
For a deeper dive into the technicalities of these machines, check out this helpful resource on what is the difference between cpap and bipap. Ultimately, understanding your body and the various options for support is key when dealing with levator ani syndrome.
| Cause | Description | Risk Factors | Symptoms |
|---|---|---|---|
| Trauma (e.g., childbirth, pelvic injury) | Direct or indirect injury to the levator ani muscles, often resulting in inflammation and scarring. | Multiple vaginal deliveries, high-impact pelvic injuries. | Localized pelvic pain, pain during intercourse, pain during bowel movements, or a feeling of heaviness in the pelvic area. |
| Chronic Constipation | Straining during bowel movements can put excessive pressure on the pelvic floor muscles, potentially leading to inflammation and pain. | Lack of fiber in diet, insufficient fluid intake, certain medications. | Pelvic pain, pain with defecation, pain during intercourse. |
| Prolonged Sitting | Sustained pressure on the pelvic floor muscles can lead to fatigue, soreness, and potential inflammation. | Occupations requiring prolonged sitting, individuals with sedentary lifestyles. | Chronic pelvic pain, pain during intercourse, pain with bowel movements. |
| Pelvic Organ Prolapse | Weakening of the pelvic floor tissues can cause pelvic organs to descend, putting pressure on the levator ani muscles. | Age, pregnancy, childbirth, genetic predisposition. | Pelvic pain, pressure or heaviness in the pelvis, urinary incontinence, bowel incontinence. |
| Inadequate Pelvic Floor Exercises | Improper or insufficient pelvic floor exercises can result in weakened or strained muscles. | Incorrect exercise technique, inadequate frequency of exercises. | Pelvic pain, pain during intercourse, urinary or bowel incontinence. |
Prevalence of Levator Ani Syndrome
The precise prevalence of Levator Ani Syndrome is not definitively established. However, given the significant role of the pelvic floor in everyday function, and the potential for various factors to impact these muscles, it is reasonable to anticipate that this condition affects a considerable portion of the population. Further research is needed to establish precise numbers.
Diagnostic Methods
Pinpointing Levator Ani Syndrome (LAS) can be tricky, as symptoms often overlap with other conditions. Accurate diagnosis relies on a comprehensive approach, combining meticulous physical examinations with appropriate imaging techniques. A thorough understanding of the diagnostic process is crucial for effective management and treatment.
Physical Examinations
Physical examinations are the initial cornerstone of diagnosing LAS. These evaluations focus on assessing the pelvic floor muscles’ strength, tone, and range of motion. A skilled practitioner will meticulously evaluate the patient’s posture, pain patterns, and any associated neurological symptoms. This process includes palpating the muscles of the pelvic floor to identify potential tenderness, spasms, or areas of restriction.
The clinician will also note any observable asymmetries or dysfunctions in the region.
Imaging Techniques
Advanced imaging techniques provide valuable insights into the underlying anatomical structures of the pelvic floor, supplementing physical examinations. These methods often reveal structural abnormalities or irregularities that might contribute to the patient’s symptoms. Different imaging modalities offer varying degrees of detail, and the choice depends on the specific clinical question.
Comparison of Diagnostic Methods
| Method | Procedure | Advantages | Disadvantages |
|---|---|---|---|
| Digital Rectal Examination (DRE) | A physician inserts a gloved finger into the rectum to palpate the pelvic floor muscles, assessing tone, tenderness, and any abnormalities. | Non-invasive, relatively inexpensive, provides immediate feedback on the pelvic floor musculature. | Subjectivity in assessment, limited visualization of deeper structures, may not be sufficient for complex cases. |
| Pelvic Floor Ultrasound | Utilizes high-frequency sound waves to visualize the pelvic floor muscles, identifying any structural or functional issues. | Provides real-time visualization of the pelvic floor, allowing for detailed assessment of muscle function and tissue health. Less invasive than MRI or CT. | Limited depth of penetration, may not be optimal for deep-seated issues, requires specialized equipment and expertise. |
| Magnetic Resonance Imaging (MRI) | Uses a powerful magnetic field and radio waves to create detailed images of the pelvic floor structures, including muscles, nerves, and ligaments. | Excellent soft tissue contrast, allows for detailed visualization of the entire pelvic floor and surrounding structures, identifying potential anatomical anomalies or nerve entrapment. | Expensive, time-consuming, may require sedation for some patients, potentially exposes the patient to radiation. |
| CT Scan | Uses X-rays and computer processing to create cross-sectional images of the pelvic floor. | Faster than MRI, may be preferable for patients with claustrophobia or metal implants, potentially provides more detailed anatomical information than ultrasound. | Higher radiation exposure than ultrasound or MRI, limited soft tissue contrast, might not be as detailed as MRI for assessing muscle function. |
Limitations of Current Diagnostic Tools
Currently, no single diagnostic method perfectly diagnoses Levator Ani Syndrome. The diagnostic process often involves a combination of approaches to reach a definitive diagnosis. Subjectivity in physical examinations, limited visualization with some imaging techniques, and the potential for overlapping symptoms with other conditions can lead to diagnostic challenges. Furthermore, the lack of standardized diagnostic criteria for LAS can complicate the process.
Researchers are constantly working to refine diagnostic tools and improve diagnostic accuracy.
Pelvic Floor Examination Procedure
A pelvic floor examination for suspected Levator Ani Syndrome typically involves the following steps:
- Patient History and Review of Symptoms: The examiner gathers detailed information about the patient’s symptoms, medical history, and any relevant risk factors.
- Physical Examination: This includes visual inspection of the perineal region, followed by palpation of the pelvic floor muscles, assessing their tone, strength, and any tenderness or trigger points.
- Neurological Assessment: The examiner evaluates reflexes and sensation in the affected area to rule out neurological involvement.
- Imaging, if necessary: Depending on the specific case, imaging techniques like ultrasound, MRI, or CT scans may be ordered to visualize the pelvic floor structures in greater detail.
- Differential Diagnosis: The examiner considers other possible conditions that could be causing the patient’s symptoms.
Treatment Approaches: What Is Levator Ani Syndrome
Managing Levator Ani Syndrome involves a multifaceted approach tailored to the individual’s specific symptoms and severity. The primary goal is to alleviate pain, restore function, and improve quality of life. Treatment options range from conservative measures to surgical interventions, and the choice often depends on the patient’s response to initial therapies.Effective treatment for Levator Ani Syndrome hinges on accurate diagnosis and a thorough understanding of the underlying causes.
A comprehensive assessment, including physical examination, imaging studies, and potentially electromyography, helps guide the selection of the most appropriate treatment strategy.
Common Treatment Approaches
Conservative therapies are frequently the initial line of defense for Levator Ani Syndrome. These approaches aim to reduce pain, improve muscle function, and promote healing without resorting to surgery. Physical therapy plays a crucial role in this phase, focusing on stretching, strengthening exercises, and manual therapy techniques to address muscle imbalances and restore proper pelvic floor function.
Conservative Treatments
Conservative treatments, such as physical therapy, pelvic floor exercises, and pain management strategies, are often employed initially. These approaches aim to address the underlying muscle imbalances and pain contributing to the syndrome. Pelvic floor physical therapy is particularly important, focusing on exercises that strengthen and stretch the pelvic floor muscles.
Surgical Interventions
Surgical interventions are considered for patients who do not respond adequately to conservative treatments or experience severe symptoms that significantly impact their quality of life. The most common surgical approaches for Levator Ani Syndrome aim to correct anatomical abnormalities, release tension on the levator ani muscles, and restore proper pelvic floor function. Surgery can involve various techniques, including muscle releases, nerve blocks, or procedures to address associated anatomical issues.
Comparison of Treatment Options
| Treatment | Description | Benefits | Drawbacks ||—|—|—|—|| Physical Therapy | Exercises, manual therapy, and education to improve muscle strength, flexibility, and coordination of the pelvic floor muscles. | Non-invasive, often covered by insurance, relatively low risk. Can improve overall pelvic floor health. | May take time to show significant improvement, requires patient commitment to exercises and follow-up appointments.
Effectiveness varies depending on individual factors. || Medications (Pain Management) | Analgesics, muscle relaxants, or anti-inflammatory drugs to reduce pain and muscle spasms. | Can provide immediate pain relief, allowing for better participation in physical therapy. | May have side effects, such as gastrointestinal issues or drowsiness. Does not address the underlying cause of the syndrome.
|| Botox Injections | Injection of botulinum toxin into specific pelvic floor muscles to temporarily relax them and reduce pain. | Can provide temporary relief from pain and spasms, allowing for better function. May be less invasive than surgery. | Temporary relief, requires repeated injections, potential for side effects at the injection site, and may not be effective for all individuals.
|| Surgical Release | Surgical procedures to release tension on the levator ani muscles, address anatomical abnormalities, or correct nerve entrapment. | Potentially provides long-term relief for severe cases, addresses underlying structural issues. | Higher risk of complications, longer recovery time, and potential for recurrence of symptoms. Not suitable for all patients. |
Potential Risks and Complications
Potential risks and complications associated with each treatment approach vary significantly. Physical therapy generally carries minimal risk, but potential complications from medications include adverse drug reactions. Botox injections may cause temporary bruising or discomfort at the injection site. Surgical interventions carry a higher risk of complications, including bleeding, infection, nerve damage, and recurrence of symptoms. The choice of treatment always needs to be made in consultation with a healthcare professional, weighing the benefits and potential risks for each individual case.
Symptoms and Associated Conditions
Understanding the symptoms of Levator Ani Syndrome is crucial for accurate diagnosis and effective treatment. It’s important to recognize that symptoms can vary significantly from person to person, and often overlap with other pelvic floor disorders. This makes accurate diagnosis a challenge, highlighting the need for a comprehensive evaluation by a healthcare professional.
Common Symptoms
Identifying the range of symptoms associated with Levator Ani Syndrome is essential for proper diagnosis. This multifaceted condition can manifest in various ways, impacting both physical comfort and overall well-being. Pain, discomfort, and dysfunction are key elements to consider.
- Pain: This can range from mild ache to sharp, intense pain in the pelvic area, perineum, or lower back. The pain may be constant or intermittent, and may worsen with certain activities like prolonged sitting or standing.
- Discomfort: This can manifest as a feeling of pressure, heaviness, or fullness in the pelvic region. It can also present as a burning sensation, particularly during or after bowel movements or sexual activity.
- Dyspareunia: Painful sexual intercourse is a common symptom, affecting both men and women. This pain can be superficial or deep and is often linked to the tension and dysfunction in the pelvic floor muscles.
- Bowel and Bladder Dysfunction: Symptoms like constipation, diarrhea, incontinence (both urine and stool), urinary urgency, or a feeling of incomplete emptying of the bladder can occur. These are often related to altered muscle function and pressure within the pelvic region.
- Sexual Dysfunction: This can manifest as reduced libido, difficulties with orgasm, or pain during or after sexual activity. This aspect of the condition often goes undiagnosed and untreated due to its sensitive nature.
- Chronic Pelvic Pain: In some cases, Levator Ani Syndrome can contribute to a more general and persistent pain condition in the pelvis and surrounding areas.
Connection to Other Pelvic Floor Disorders, What is levator ani syndrome
Levator Ani Syndrome frequently coexists with or is mistaken for other pelvic floor disorders. Understanding these overlaps is crucial for differentiating the conditions and developing an effective treatment plan.
Conditions like pelvic organ prolapse, endometriosis, interstitial cystitis, and chronic prostatitis can share overlapping symptoms with Levator Ani Syndrome. Therefore, a comprehensive evaluation is essential to pinpoint the exact cause of the patient’s symptoms.
Symptom Comparison Table
| Condition | Symptom 1 | Symptom 2 | Symptom 3 |
|---|---|---|---|
| Levator Ani Syndrome | Pelvic pain, often deep and radiating | Painful bowel movements or urination | Dyspareunia (painful sex) |
| Pelvic Organ Prolapse | Feeling of heaviness or dragging in the pelvis | Urinary or fecal incontinence | Low back pain |
| Endometriosis | Pelvic pain, often cyclical | Painful menstruation | Dyspareunia |
| Interstitial Cystitis | Chronic pelvic pain | Frequent urination | Urgency and pain |
Potential Complications and Long-Term Effects
The potential complications of Levator Ani Syndrome depend largely on the severity and duration of the condition. Left untreated, the chronic pain and dysfunction can negatively impact quality of life. Long-term effects can include chronic pelvic pain, decreased sexual function, and psychological distress. Early diagnosis and appropriate management are essential to mitigate these potential complications.
Prognosis and Management

Levator ani syndrome, while not a life-threatening condition, can significantly impact a person’s quality of life. Understanding the potential outcomes and effective management strategies is crucial for individuals experiencing this condition. This section explores the expected course of the syndrome, symptom management techniques, and the importance of consistent medical follow-up.
Expected Outcomes
The prognosis for levator ani syndrome varies depending on the severity of the condition, the individual’s response to treatment, and the presence of any underlying conditions. In many cases, individuals with mild to moderate levator ani syndrome experience significant improvement with appropriate management. Symptoms may lessen over time, and the individual may achieve a good quality of life.
Levator ani syndrome is a condition that often causes pelvic pain, and while its exact causes aren’t fully understood, some researchers think it might be linked to similar factors impacting hair loss, like those associated with male or female pattern baldness. However, the exact mechanisms are still under investigation, and the connection between these conditions is currently speculative.
Ultimately, levator ani syndrome is a complex issue requiring careful diagnosis and treatment.
However, some individuals may experience persistent or recurring symptoms, potentially requiring ongoing management. A personalized approach, considering the individual’s specific situation, is essential to anticipate and manage the expected outcomes.
Symptom Management Strategies
Effective symptom management is key to improving the quality of life for those with levator ani syndrome. This involves a multifaceted approach tailored to the individual’s needs. Physical therapy plays a crucial role in strengthening pelvic floor muscles and improving flexibility. Pain management strategies may include over-the-counter medications, physical therapy, and, in some cases, prescription medications. Relaxation techniques, such as yoga or meditation, can help manage stress and muscle tension, contributing to symptom relief.
Behavioral modifications, like adjusting bowel habits and avoiding prolonged sitting, can also reduce symptoms.
Importance of Regular Follow-up Appointments
Regular follow-up appointments are essential for monitoring the condition’s progress, adjusting treatment plans, and identifying potential complications. These appointments allow healthcare professionals to assess the effectiveness of current interventions, identify any new symptoms or changes in the condition, and adjust the treatment plan as needed. Follow-up visits provide a valuable opportunity to discuss any concerns, questions, or changes in lifestyle that may impact the condition.
Lifestyle Modifications
Implementing lifestyle changes can significantly contribute to managing levator ani syndrome. These modifications focus on reducing strain on the pelvic floor muscles and promoting overall well-being.
- Maintaining a Healthy Diet: A balanced diet rich in fiber can help prevent constipation, reducing strain on the pelvic floor. Constipation can exacerbate symptoms, so maintaining regular bowel movements is crucial. Fruits, vegetables, and whole grains can contribute to digestive health.
- Regular Exercise: Engaging in regular exercise, especially low-impact activities like walking or swimming, can help strengthen core muscles and improve overall fitness, potentially reducing the severity of symptoms. Avoid activities that put excessive stress on the pelvic floor.
- Stress Management Techniques: Chronic stress can contribute to muscle tension and worsen levator ani syndrome symptoms. Practicing relaxation techniques, such as deep breathing exercises, meditation, or yoga, can help manage stress and promote overall well-being.
- Posture Awareness: Maintaining good posture, especially when sitting or standing for extended periods, can help reduce strain on the pelvic floor muscles. Using ergonomic furniture and proper body mechanics can make a difference.
- Avoiding Prolonged Sitting: Sitting for extended periods can put pressure on the pelvic floor. Taking breaks, standing up regularly, and using a supportive cushion when sitting can help reduce the impact on the muscles.
Research and Future Directions
Unraveling the complexities of levator ani syndrome requires ongoing research. Current understanding, while substantial, still leaves gaps in our knowledge regarding the precise mechanisms driving the condition, the best diagnostic tools, and the optimal treatment strategies. This section will explore key areas needing further investigation and highlight potential implications of recent findings.
Areas Requiring Further Research
A deeper understanding of the pathophysiology of levator ani syndrome is paramount. Researchers need to investigate the interplay of factors, including genetics, hormonal influences, and lifestyle habits, to identify specific risk factors and potential triggers. The development of more sophisticated imaging techniques, such as advanced MRI protocols and novel ultrasound methods, can offer a clearer picture of the pelvic floor musculature and potential structural anomalies.
Additionally, longitudinal studies tracking the progression of the syndrome over time are essential to understand its natural course and predict individual outcomes.
Potential Implications of Recent Research Findings
Recent research on pelvic floor disorders has yielded valuable insights into the role of neuromuscular dysfunction in levator ani syndrome. This knowledge can lead to the development of more targeted diagnostic tests and the creation of personalized treatment plans. For instance, studies exploring the use of electromyography (EMG) to assess muscle activity in the pelvic floor may offer a more objective measure of muscle weakness or dysfunction.
This could be used to guide rehabilitation exercises and tailor treatment protocols for each patient.
Emerging Trends in Pelvic Floor Disorders
The field of pelvic floor disorders is experiencing a surge in innovative approaches. Biofeedback therapy, combined with digital technologies, is gaining traction. Real-time feedback allows patients to visualize and control their pelvic floor muscles, leading to improved muscle activation and potentially faster recovery. Furthermore, the development of minimally invasive surgical techniques is transforming the treatment landscape. Robotic surgery, for example, offers enhanced precision and control during procedures, minimizing invasiveness and potentially improving patient outcomes.
Illustrative Case Study
A 35-year-old female presented with progressive pelvic pain and dyspareunia. She reported increasing difficulty with bowel and bladder control, accompanied by a sense of pelvic heaviness. Physical examination revealed decreased tone and reduced sensation in the levator ani muscles. Pelvic floor MRI demonstrated subtle but consistent structural abnormalities in the levator ani muscles, suggestive of chronic inflammation.
Biofeedback therapy and targeted pelvic floor exercises were implemented. A combination of manual therapy and targeted exercises aimed at restoring muscle function and reducing inflammation proved successful in alleviating symptoms. The patient experienced a significant reduction in pain and improvement in bowel and bladder control within three months. This case exemplifies the potential for a multidisciplinary approach to treating levator ani syndrome.
Closing Summary
In conclusion, levator ani syndrome presents a multifaceted challenge to pelvic health. The condition, characterized by a range of symptoms and potential causes, necessitates a personalized approach to diagnosis and treatment. From physical examinations to imaging techniques and diverse treatment options, managing levator ani syndrome requires careful consideration of individual needs and circumstances. Ultimately, a proactive approach to managing this condition, coupled with ongoing research and advancements in pelvic floor care, holds the key to improving the quality of life for those affected.

