Types of sleep disorders affect millions worldwide, disrupting not only individual well-being but also impacting society as a whole. From the common struggles of insomnia to the more complex conditions like sleep apnea, understanding the different types and their underlying causes is crucial for effective management and treatment. This exploration delves into the various sleep disorders, outlining their characteristics, symptoms, and treatment options.
This comprehensive guide will cover everything from the different classifications of insomnia, including acute, chronic, and transient types, to the complexities of sleep apnea, narcolepsy, and hypersomnia. We’ll also examine less common sleep disorders, exploring their unique features and the potential impact they have on daily life. Ultimately, this guide aims to empower readers with knowledge to better understand, manage, and seek appropriate help for sleep-related issues.
Introduction to Sleep Disorders
Sleep disorders are conditions that disrupt the normal sleep-wake cycle, impacting the quality and quantity of sleep. These disorders can range from minor inconveniences to severe medical conditions, significantly affecting an individual’s physical and mental well-being. Their prevalence is substantial, affecting a considerable portion of the population globally, and their impact extends beyond the individual, impacting societal productivity and healthcare costs.Sleep disorders encompass a wide spectrum of conditions, often characterized by difficulty falling asleep, staying asleep, or experiencing unusual sleep behaviors.
These issues can lead to daytime fatigue, reduced alertness, and impaired cognitive function, negatively impacting daily activities and interpersonal relationships. Understanding these disorders is crucial for early diagnosis and effective treatment, leading to improved quality of life for affected individuals and contributing to a healthier society.
Prevalence and Impact
Sleep disorders affect a significant portion of the population worldwide. Studies consistently show that a substantial percentage of adults experience some form of sleep disruption, impacting their overall health and productivity. The consequences extend beyond individual suffering, impacting various aspects of society, including reduced workplace productivity, increased healthcare costs, and an elevated risk of accidents. This impact underscores the importance of recognizing and addressing sleep disorders as a public health concern.
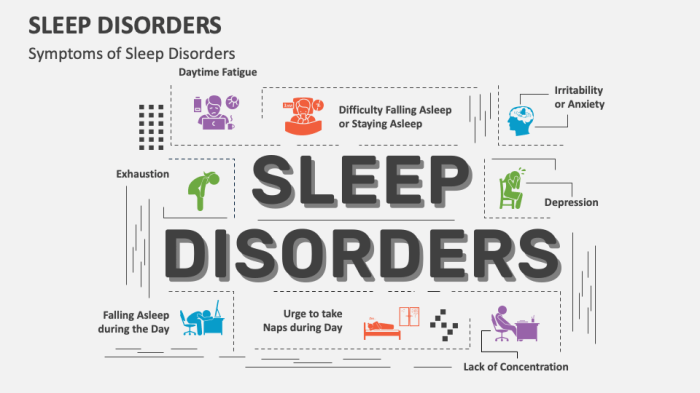
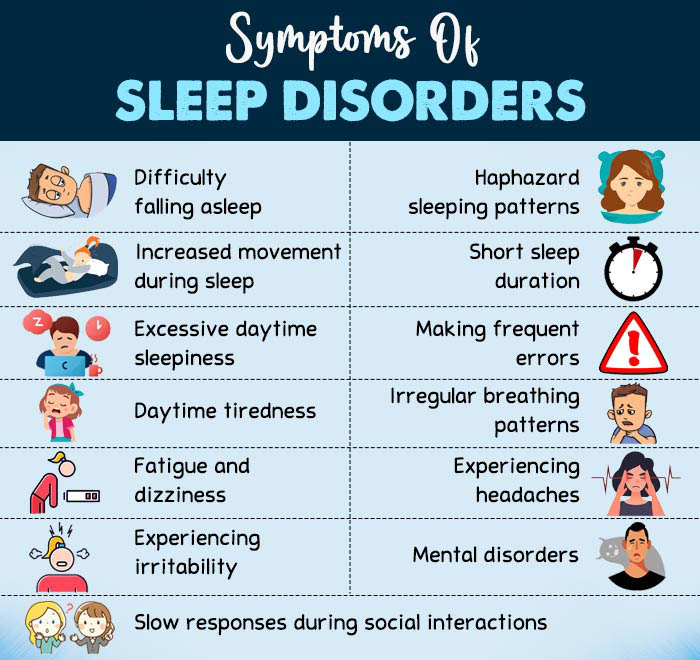
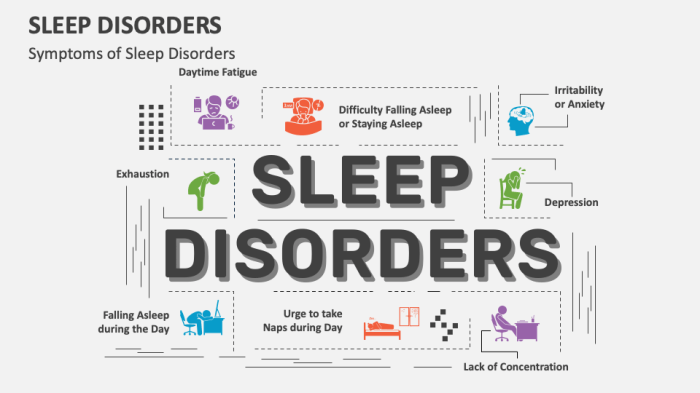
Common Symptoms
Various sleep disorders exhibit a range of symptoms. Common symptoms include difficulty falling asleep, frequent awakenings during the night, prolonged sleepiness during the day, and experiencing unusual sleep behaviors like sleepwalking or sleep paralysis. These symptoms can vary in severity and frequency depending on the specific disorder. Understanding these common symptoms can aid in early identification and appropriate intervention.
Categories of Sleep Disorders
Recognizing the different categories of sleep disorders is essential for appropriate diagnosis and treatment. The following table provides a summary of common sleep disorders, categorized for clarity.
| Category | Description |
|---|---|
| Insomnia | Characterized by persistent difficulty falling asleep, staying asleep, or experiencing restful sleep. This can stem from various factors including stress, anxiety, or underlying medical conditions. |
| Sleep-Related Breathing Disorders | These disorders involve disruptions in breathing during sleep, often leading to reduced oxygen levels. Examples include obstructive sleep apnea, a condition where the airway becomes blocked during sleep. |
| Parasomnias | These disorders involve unusual or undesirable behaviors during sleep, including sleepwalking, night terrors, and restless legs syndrome. These can be triggered by various factors, including stress, fatigue, or underlying medical conditions. |
| Circadian Rhythm Sleep-Wake Disorders | These disorders involve a mismatch between an individual’s natural sleep-wake cycle and their environment. Examples include jet lag and shift work sleep disorder. |
| Hypersomnia | Characterized by excessive daytime sleepiness, even after adequate sleep duration. This can stem from various factors, including underlying medical conditions or sleep disorders. |
| Narcolepsy | A neurological disorder characterized by excessive daytime sleepiness, sudden episodes of muscle weakness (cataplexy), and other sleep-related issues. |
Types of Insomnia
Insomnia isn’t a single entity; it presents in various forms, each with its own set of characteristics. Understanding these different types is crucial for effective diagnosis and treatment. Different types of insomnia require tailored approaches to address the underlying causes and promote healthy sleep.Insomnia can be categorized based on its duration and the contributing factors. This classification helps clinicians determine the appropriate treatment strategy, which might vary significantly depending on the specific type of insomnia experienced.
Acute Insomnia
Acute insomnia, also known as short-term insomnia, is a temporary sleep disturbance lasting for a few days or weeks. It often arises due to a stressful event, such as a major life change, travel, or a significant medical issue.Common causes of acute insomnia include: work-related stress, relationship problems, significant life changes, travel across time zones, or illness. The stress response, in these situations, can trigger a cascade of physiological changes, ultimately disrupting the sleep-wake cycle.
Often, the underlying cause is temporary and resolves with time, allowing sleep to return to normal.
Chronic Insomnia
Chronic insomnia is a more persistent sleep problem, typically defined as difficulty sleeping for at least three nights a week for a minimum of three months. It is often a complex condition with a multitude of potential contributing factors.Chronic insomnia is often linked to underlying medical conditions, such as chronic pain, depression, anxiety, or sleep apnea. Lifestyle factors like irregular sleep schedules, poor sleep hygiene, and substance use can also contribute to chronic insomnia.
Understanding sleep disorders is crucial for overall well-being, but did you know what you eat can significantly impact your sleep? For example, incorporating the ten best foods for IBS, like those listed in this helpful guide the ten best foods for ibs , can actually help regulate your digestive system and improve sleep quality. Different sleep disorders, like insomnia or sleep apnea, can then be approached with a more holistic and balanced approach.
The interplay between physical and mental health conditions makes chronic insomnia more challenging to treat compared to acute insomnia.
Transient Insomnia
Transient insomnia, unlike acute insomnia, is a brief period of sleeplessness that occurs intermittently over time. This type of insomnia can be caused by a variety of factors, such as a change in routine, environmental factors, or stress.Environmental factors, such as a noisy bedroom or an uncomfortable temperature, can lead to transient insomnia. In addition, changes in routine, such as a shift in work schedule, can also trigger transient insomnia.
The duration of this type of insomnia can range from a few nights to a few weeks.
Ever wondered why some nights feel like a restless sea of tossing and turning? Sleep disorders come in various forms, from insomnia to sleep apnea. One interesting area of potential connection is the impact of different types of carbohydrates on sleep quality. For instance, consuming a balanced diet including plenty of complex carbohydrates, like those found in whole grains and vegetables, can contribute to better sleep, while a diet heavy in simple carbohydrates, like those in sugary foods and processed snacks, might lead to disruptions.
Learning more about the relationship between diet and sleep can be really helpful in managing sleep disorders effectively. Understanding the role of simple and complex carbohydrates is a key part of that puzzle. Ultimately, understanding the different types of sleep disorders is crucial for anyone looking to improve their sleep.
Treatment Approaches
Treatment approaches for different types of insomnia vary. For acute insomnia, focusing on stress reduction techniques, such as relaxation exercises or cognitive behavioral therapy (CBT-I), often proves effective. For chronic insomnia, a multi-pronged approach, often including CBT-I, lifestyle modifications, and sometimes medication, may be necessary.CBT-I is a widely used and often effective treatment for all types of insomnia.
It helps individuals identify and modify negative thoughts and behaviors related to sleep. Medication, when prescribed, may be used in conjunction with CBT-I or as an adjunct to lifestyle modifications.
Sleep Hygiene Practices for Insomnia
Consistent sleep hygiene practices are crucial for promoting healthy sleep and can be beneficial in managing insomnia. A consistent sleep schedule, a relaxing bedtime routine, and a comfortable sleep environment contribute to the overall sleep experience.
| Sleep Hygiene Practice | Description |
|---|---|
| Regular Sleep Schedule | Going to bed and waking up around the same time each day, even on weekends, helps regulate the body’s natural sleep-wake cycle. |
| Relaxing Bedtime Routine | Engaging in calming activities before bed, such as reading or taking a warm bath, can signal to the body that it’s time to wind down. |
| Comfortable Sleep Environment | Maintaining a dark, quiet, and cool bedroom environment promotes better sleep quality. |
| Avoidance of Caffeine and Alcohol Before Bed | These substances can interfere with sleep quality and duration. |
| Regular Exercise | Physical activity is beneficial for overall health, including sleep. However, avoid intense exercise close to bedtime. |
| Healthy Diet | Maintaining a balanced diet can contribute to better sleep. |
Other Common Sleep Disorders
Beyond insomnia, a spectrum of other sleep disorders can significantly impact your well-being. Understanding these conditions is crucial for recognizing symptoms and seeking appropriate help. These disorders, while different, often share overlapping symptoms, making accurate diagnosis and effective treatment essential.
Sleep Apnea
Sleep apnea is a common sleep disorder characterized by pauses in breathing during sleep. These pauses can last from a few seconds to a minute or more, and they repeatedly disrupt the sleep cycle, leading to fragmented and poor-quality rest. There are three primary types of sleep apnea:
- Obstructive sleep apnea (OSA): This is the most common type, caused by a blockage of the airway during sleep. The blockage can be due to various factors, including excess throat tissue, a large tongue, or a receding jaw. The muscles in the throat relax, obstructing the flow of air. Symptoms frequently include snoring, gasping, or choking sounds during sleep.
- Central sleep apnea (CSA): In this type, the brain fails to send the proper signals to the muscles controlling breathing, leading to pauses in breathing. CSA can be associated with certain medical conditions like heart failure or stroke. Symptoms may include excessive daytime sleepiness, but may not involve as loud or noticeable snoring as in OSA.
- Mixed sleep apnea: This is a combination of obstructive and central sleep apnea, presenting symptoms from both types. Individuals with mixed sleep apnea may experience both airway blockage and a lack of breathing signals from the brain.
Symptoms of sleep apnea often include excessive daytime sleepiness, morning headaches, and difficulty concentrating. Diagnostic methods typically involve a sleep study (polysomnography), which monitors brain waves, breathing, heart rate, and oxygen levels during sleep. A sleep study is essential for accurately diagnosing the type and severity of sleep apnea.
Risk Factors and Consequences of Untreated Sleep Apnea
Untreated sleep apnea can lead to a range of serious health consequences. Risk factors include obesity, a family history of sleep apnea, and certain medical conditions. The consequences of untreated sleep apnea extend beyond just daytime fatigue. Uncontrolled sleep apnea is linked to increased risks of high blood pressure, heart disease, stroke, type 2 diabetes, and even depression.
The consistent disruption of the sleep cycle due to sleep apnea affects the body’s ability to regulate hormones and other crucial bodily functions.
Treatment Options for Sleep Apnea
Fortunately, sleep apnea is often treatable. Treatment options vary depending on the type and severity of the disorder. Common treatments include:
- Lifestyle changes: Weight loss, avoiding alcohol and sedatives before bed, and practicing good sleep hygiene can significantly improve symptoms in some cases.
- Continuous positive airway pressure (CPAP) therapy: This is a common and effective treatment for obstructive sleep apnea. A CPAP machine delivers a gentle stream of air pressure through a mask, keeping the airway open during sleep.
- Oral appliances: These devices are custom-fitted mouthpieces that reposition the jaw and tongue to keep the airway open. They are a suitable alternative to CPAP for some individuals.
- Surgery: In some cases, surgery may be recommended to address anatomical issues contributing to airway blockage.
Proper diagnosis and individualized treatment plans are crucial for effective management of sleep apnea.
Narcolepsy and Hypersomnia
Narcolepsy and hypersomnia are sleep disorders characterized by excessive daytime sleepiness. However, they differ in their underlying causes and symptoms.
Narcolepsy
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It’s characterized by an irresistible urge to sleep during the day, often with sudden attacks of sleep, along with other symptoms like cataplexy (sudden muscle weakness), hallucinations, and sleep paralysis. While the exact cause of narcolepsy is unknown, genetic predisposition and autoimmune factors are suspected to play a role.
Treatments for narcolepsy typically involve medications to manage symptoms.
Hypersomnia
Hypersomnia is a condition characterized by excessive daytime sleepiness lasting for at least three months, but without the other specific symptoms of narcolepsy. Hypersomnia can be caused by various factors, including underlying medical conditions or certain medications. Treatments for hypersomnia focus on addressing the underlying cause and may include medications to promote wakefulness or therapy to improve sleep habits.
Comparing Sleep Apnea, Narcolepsy, and Hypersomnia
| Characteristic | Sleep Apnea | Narcolepsy | Hypersomnia |
|---|---|---|---|
| Primary Symptom | Pauses in breathing during sleep | Irresistible daytime sleepiness, cataplexy | Excessive daytime sleepiness |
| Cause | Airway obstruction, brain signals | Neurological dysfunction | Underlying medical conditions, medications |
| Treatment | CPAP, lifestyle changes, surgery | Medications | Medications, therapy |
Less Common Sleep Disorders
Beyond the more prevalent sleep disorders like insomnia and sleep apnea, a range of less common conditions can significantly impact sleep quality and overall well-being. These conditions often require specialized diagnostic and treatment approaches. Understanding these less common sleep disorders can help individuals and healthcare professionals identify potential issues and implement effective strategies for improved sleep health.
Specific Sleep Disorders
A variety of less common sleep disorders exist, each with unique characteristics, potential causes, and treatment options. These conditions can affect individuals at any age and may co-occur with other medical or psychological issues. Accurate diagnosis and tailored treatment are crucial for effective management.
Kleine-Levin Syndrome
Kleine-Levin syndrome (KLS) is a rare neurological disorder primarily affecting adolescents and young adults. Characterized by cyclical periods of hypersomnia (excessive sleepiness), behavioral changes, and sometimes hyperphagia (excessive eating), KLS can severely disrupt daily routines and social functioning. These episodes are often unpredictable, lasting from several days to weeks, interspersed with periods of normal activity.
Narcolepsy
Narcolepsy is a chronic neurological disorder characterized by excessive daytime sleepiness. While often associated with cataplexy (sudden loss of muscle tone), other symptoms such as sleep paralysis and hypnagogic hallucinations can also occur. The underlying cause of narcolepsy remains unclear, but genetic factors and immune system dysfunction are suspected.
Restless Legs Syndrome (RLS), Types of sleep disorders
Restless legs syndrome (RLS) is a neurological disorder characterized by unpleasant sensations in the legs, often described as creeping, crawling, or itching. These sensations are typically worse at night and often lead to an irresistible urge to move the legs. RLS can significantly impact sleep quality and lead to fatigue and daytime dysfunction. It is estimated that RLS affects approximately 5-10% of the population.
Periodic Limb Movement Disorder (PLMD)
Periodic limb movement disorder (PLMD) is characterized by repetitive, involuntary movements of the legs and sometimes arms during sleep. These movements, which can include jerking or flexing, often occur in cycles and can be disruptive to sleep. While the specific cause of PLMD isn’t fully understood, factors such as genetics, age, and certain medications have been linked to its occurrence.
Sleepwalking (Somnambulism)
Sleepwalking, or somnambulism, involves walking or performing other complex behaviors while asleep. Episodes typically occur during non-rapid eye movement (NREM) sleep stages and are usually not associated with conscious awareness. While often benign, sleepwalking can be distressing for the individual and those around them, and it is sometimes linked to underlying medical conditions or psychological stress.
Table of Less Common Sleep Disorders
| Disorder | Symptoms | Potential Causes | Treatment Options |
|---|---|---|---|
| Kleine-Levin Syndrome | Hypersomnia, behavioral changes, hyperphagia | Neurological dysfunction, genetic predisposition | Medications (e.g., stimulants), behavioral therapy |
| Narcolepsy | Excessive daytime sleepiness, cataplexy, sleep paralysis, hypnagogic hallucinations | Genetic factors, immune system dysfunction | Medications (e.g., stimulants, antidepressants), lifestyle adjustments |
| Restless Legs Syndrome | Unpleasant sensations in the legs, urge to move | Genetics, neurological factors, iron deficiency, medications | Medications (e.g., dopamine agonists), lifestyle changes, iron supplements |
| Periodic Limb Movement Disorder | Repetitive involuntary movements of the limbs during sleep | Genetics, age, medications | Medications (e.g., benzodiazepines), lifestyle modifications |
| Sleepwalking (Somnambulism) | Walking or performing complex behaviors while asleep | Stress, sleep deprivation, medications, underlying medical conditions | Addressing underlying issues, sleep hygiene improvements, medications (in some cases) |
Diagnosis and Treatment Approaches
Unraveling the mysteries of sleep disorders requires a meticulous approach, combining expert knowledge with the patient’s active participation. Accurate diagnosis is the cornerstone of effective treatment, enabling personalized strategies to restore healthy sleep patterns. A comprehensive understanding of diagnostic methods, treatment options, and the vital role of lifestyle modifications is crucial for managing sleep disorders effectively.
Methods for Diagnosing Sleep Disorders
Sleep disorders often manifest subtly, making accurate diagnosis challenging. Physicians employ a multi-faceted approach, gathering detailed information about the patient’s sleep habits, medical history, and lifestyle factors. This comprehensive evaluation lays the groundwork for identifying the underlying cause of the sleep disturbance.
Diagnostic Tools and Techniques
A variety of tools and techniques are used to assess sleep disorders. Polysomnography (PSG) is a standard procedure, involving overnight monitoring of brain waves, eye movements, muscle activity, and breathing patterns. Actigraphy, a less invasive method, uses a small device worn on the wrist to track sleep-wake cycles over a period of time. These objective measures provide valuable insights into sleep patterns, aiding in the diagnosis of various sleep disorders.
Role of Sleep Specialists and Healthcare Providers
Sleep specialists, with their specialized training and expertise, play a pivotal role in diagnosing and treating sleep disorders. They utilize their knowledge of sleep physiology and disorders to interpret the data collected from diagnostic tools. Collaboration with primary care physicians and other healthcare professionals ensures a holistic approach, integrating medical history and physical examination findings to formulate an accurate diagnosis.
Common and Alternative Therapies for Treating Sleep Disorders
Numerous therapies are available for treating sleep disorders, ranging from conventional approaches to alternative strategies. Cognitive behavioral therapy for insomnia (CBT-I) is a widely recognized method that addresses the psychological factors contributing to insomnia. Pharmacological interventions, such as the use of sleep medications, may be considered in some cases, but should be carefully evaluated in consultation with a healthcare professional.
Ever wondered about those strange sleep disorders? From insomnia to sleep apnea, there’s a whole spectrum of issues. Interestingly, some digestive problems, like the mysterious sulfur burps, can sometimes be linked to sleep disruptions. If you’re curious about what causes sulfur burps, check out this insightful article what causes sulfur burps. Understanding these connections helps paint a broader picture of overall health and wellness, and ultimately, helps us better address the various types of sleep disorders.
Alternative therapies, such as relaxation techniques and mindfulness practices, are often incorporated into treatment plans to promote overall well-being and improve sleep quality.
Comparison of Different Treatment Approaches
Various treatment approaches offer distinct advantages and disadvantages. CBT-I, for example, focuses on modifying thought patterns and behaviors related to sleep, proving effective in the long term without reliance on medication. Pharmacological interventions can provide rapid relief but may carry potential side effects and are generally not a long-term solution. Alternative therapies offer complementary approaches, often improving sleep quality by promoting relaxation and stress reduction.
Choosing the most appropriate treatment depends on the individual’s specific needs and preferences, and is a decision made collaboratively with a healthcare professional.
Importance of Lifestyle Modifications in Managing Sleep Disorders
Adopting healthy lifestyle habits plays a critical role in managing sleep disorders. Regular exercise, maintaining a consistent sleep schedule, and establishing a relaxing bedtime routine can significantly improve sleep quality. Dietary factors, such as avoiding caffeine and alcohol before bed, are also important considerations. Creating a conducive sleep environment, including a dark, quiet, and cool bedroom, can also contribute to better sleep.
Treatment Options Table
| Treatment Option | Description | Effectiveness (Generally) | Suitable for |
|---|---|---|---|
| Cognitive Behavioral Therapy for Insomnia (CBT-I) | Addresses negative thoughts and behaviors related to sleep. | High, long-term | Insomnia, various sleep disorders |
| Pharmacological Interventions (e.g., Sleep Medications) | Medication to induce sleep. | Moderate, short-term | Insomnia, when other methods are ineffective |
| Relaxation Techniques (e.g., Deep Breathing) | Techniques to reduce stress and promote relaxation. | Moderate, complementary | Various sleep disorders, stress-related sleep issues |
| Lifestyle Modifications | Regular exercise, consistent sleep schedule, healthy diet. | High, long-term, preventative | All sleep disorders |
Impact of Sleep Disorders on Daily Life: Types Of Sleep Disorders
Sleep disorders are not just a nuisance; they significantly impact various aspects of daily life, affecting physical and mental well-being, social interactions, and overall productivity. The consequences can range from minor inconveniences to serious health complications, highlighting the importance of recognizing and addressing sleep disturbances.Sleep deprivation, a common consequence of untreated sleep disorders, has profound and far-reaching effects on a person’s daily functioning.
The cumulative impact of poor sleep can lead to decreased performance in various domains, including physical health, mental acuity, and social interactions.
Effects on Physical Health
Sleep is crucial for the body’s restorative processes. Insufficient sleep disrupts the body’s natural rhythm, leading to a multitude of physical health problems. Chronic sleep deprivation can weaken the immune system, increasing susceptibility to infections. It can also contribute to cardiovascular issues, such as high blood pressure and an increased risk of heart disease. Furthermore, sleep disorders have been linked to metabolic disturbances, contributing to weight gain and the development of type 2 diabetes.
Maintaining healthy sleep patterns is essential for overall physical well-being.
Effects on Mental Health
Sleep plays a vital role in regulating mood and emotional responses. Chronic sleep deprivation can significantly impact mental health, increasing the risk of developing mood disorders like depression and anxiety. Sleep deprivation impairs cognitive functions such as concentration, memory, and problem-solving, leading to decreased productivity and overall mental well-being. Individuals with sleep disorders often experience heightened irritability, difficulty managing stress, and diminished emotional regulation.
A healthy sleep cycle is essential for maintaining mental stability and resilience.
Effects on Social Functioning
Sleep disorders can strain interpersonal relationships. Individuals experiencing chronic sleep deprivation may exhibit irritability, mood swings, and difficulty concentrating, which can lead to social conflicts and misunderstandings. These issues can negatively impact relationships with family members, friends, and colleagues, ultimately affecting social interactions. Lack of sleep can also hinder the ability to engage in social activities and maintain social connections, potentially leading to isolation and loneliness.
Consistent sleep allows for more effective and harmonious interactions.
Impact on Academic or Professional Performance
Sufficient sleep is critical for optimal cognitive function. Students and professionals alike rely on alertness, focus, and memory to succeed in their academic or professional pursuits. Sleep disorders can significantly impair these abilities, leading to decreased academic performance, lower productivity, and diminished job satisfaction. Sleep deprivation can impact attention span, problem-solving skills, and decision-making abilities, hindering performance in both academic and professional settings.
Consistent and adequate sleep directly correlates with improved performance in various areas.
Correlation Between Sleep Disorders and Other Health Conditions
| Sleep Disorder | Potential Associated Health Conditions |
|---|---|
| Insomnia | Depression, anxiety, hypertension, obesity, diabetes |
| Sleep Apnea | High blood pressure, heart disease, stroke, type 2 diabetes, obesity |
| Narcolepsy | Weakened immune system, sleep paralysis, cataplexy, depression |
| Restless Legs Syndrome | Anxiety, depression, pain conditions |
This table illustrates potential correlations between common sleep disorders and various health conditions. It highlights the interconnectedness of sleep and overall health, emphasizing the importance of addressing sleep disturbances to prevent and manage potential health complications. Further research is needed to fully understand the intricate relationship between these conditions.
Prevention and Management Strategies
Taking proactive steps to prevent sleep disorders and manage existing ones is crucial for overall well-being. A consistent sleep routine, healthy habits, and stress reduction techniques are powerful tools in maintaining optimal sleep quality. By addressing potential triggers and adopting effective strategies, individuals can significantly improve their sleep and daily functioning.Maintaining a healthy sleep-wake cycle, coupled with sleep hygiene practices, is paramount in preventing sleep disorders and promoting restorative sleep.
Stress management techniques, coupled with regular exercise, can further enhance sleep quality and resilience.
Maintaining a Healthy Sleep Schedule
A regular sleep schedule, including consistent bedtimes and wake-up times, even on weekends, helps regulate the body’s natural sleep-wake cycle. This consistency reinforces the body’s internal clock, leading to improved sleep quality and duration. Establishing a pre-sleep routine can also signal to the body that it’s time to wind down, promoting relaxation and preparing for sleep.
Sleep Hygiene Practices
Sleep hygiene encompasses a set of habits that promote healthy sleep. These include creating a conducive sleep environment—a dark, quiet, and cool bedroom—and avoiding stimulating activities before bed, such as using electronic devices. Avoiding large meals and caffeine or alcohol close to bedtime can also significantly improve sleep quality. A comfortable mattress and pillows are also essential for a good night’s rest.
Stress Management Techniques
Chronic stress can significantly disrupt sleep patterns. Therefore, incorporating stress-reducing techniques into daily life is essential. These techniques include relaxation exercises, mindfulness practices, meditation, or spending time in nature. Finding healthy outlets for stress, such as hobbies or spending time with loved ones, can contribute to better sleep.
Promoting Healthy Sleep Habits
Adopting healthy sleep habits is key to preventing and managing sleep disorders. These habits include avoiding excessive daytime napping, ensuring regular physical activity, and maintaining a healthy diet. Creating a relaxing bedtime routine, such as taking a warm bath or reading a book, can also signal to the body that it’s time to wind down.
Regular Exercise
Regular physical activity plays a vital role in improving sleep quality. Exercise promotes better sleep by reducing stress, improving mood, and regulating body temperature. However, avoiding strenuous exercise too close to bedtime is crucial, as this can have the opposite effect.
Practical Tips for Improving Sleep Quality
| Category | Tip | Explanation |
|---|---|---|
| Sleep Schedule | Maintain a consistent sleep schedule, including weekends. | Consistency reinforces the body’s internal clock, improving sleep quality. |
| Sleep Environment | Create a dark, quiet, and cool bedroom. | A conducive environment promotes relaxation and sleep. |
| Pre-Sleep Routine | Establish a relaxing bedtime routine, such as taking a warm bath. | Signals to the body it’s time to wind down. |
| Diet and Lifestyle | Avoid large meals and caffeine or alcohol before bed. | These substances can interfere with sleep quality. |
| Stress Management | Practice relaxation techniques like meditation. | Reduces stress, a major sleep disruptor. |
| Exercise | Engage in regular physical activity, but avoid strenuous exercise close to bedtime. | Promotes better sleep by reducing stress and improving mood. |
Outcome Summary
In conclusion, navigating the world of sleep disorders requires a multifaceted approach. By understanding the different types, their causes, and the available treatment options, individuals can take proactive steps towards better sleep health. This guide has provided a thorough overview of various sleep disorders, emphasizing the importance of seeking professional help when needed. Ultimately, prioritizing sleep hygiene, adopting healthy lifestyle choices, and seeking support from qualified healthcare professionals are key components of effective sleep management.