Oral thrush home remedies offer a range of potential solutions for managing this common oral infection. Understanding the causes, symptoms, and various treatment approaches is key to effectively addressing oral thrush at home. This guide explores a variety of natural and practical methods, from dietary changes to oral hygiene practices, to help alleviate symptoms and prevent recurrence.
This comprehensive resource delves into the different facets of oral thrush, covering everything from its underlying causes to the effectiveness of diverse home remedies. It also examines the importance of proper diagnosis and when professional medical attention is necessary.
Understanding Oral Thrush
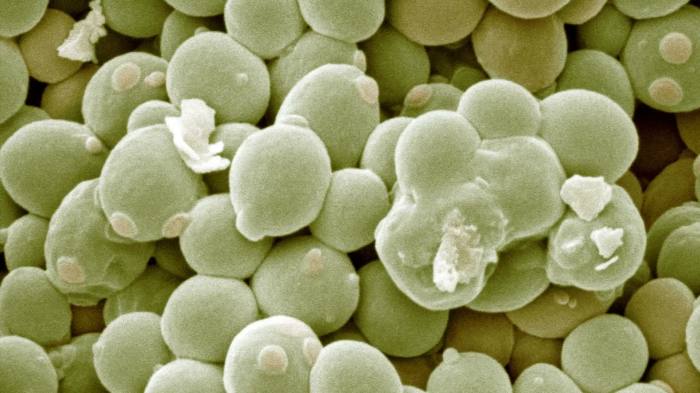
Oral thrush, a common fungal infection, affects the mouth and throat. It’s characterized by the growth of the yeast-like fungus Candida albicans, which typically resides in the mouth but can overgrow under certain circumstances. Understanding its causes, symptoms, and risk factors is crucial for early detection and treatment.Oral thrush often presents as white or yellowish patches on the tongue, inner cheeks, and gums.
These patches may appear thick and slightly raised, and can sometimes be scraped off, revealing red, inflamed underlying tissue. Symptoms can range from mild discomfort to severe pain, making eating and drinking challenging. Early recognition is essential for prompt intervention and relief.
Causes of Oral Thrush
Oral thrush is frequently linked to weakened immune systems. This can be due to a variety of factors, including certain medical conditions, medications, or lifestyle choices. A compromised immune system allows the Candida fungus to proliferate more easily. Weakened immune responses can be seen in individuals with HIV/AIDS, those undergoing chemotherapy, or patients taking broad-spectrum antibiotics. These conditions disrupt the delicate balance of the oral microbiome, creating an environment conducive to the overgrowth of Candida.
Finding home remedies for oral thrush can be tricky, but sometimes the culprit might surprise you. It’s amazing how often seemingly unrelated things, like laundry detergent allergies, can actually impact our health. Understanding the signs and symptoms of these allergies is key, as they can often mimic other conditions. Learning more about this can help you pinpoint the cause of your oral thrush, and you can find more information about laundry detergent allergies, signs, symptoms, and treatment here: laundry detergent allergies signs symptoms and treatment.
Back to oral thrush, though, try incorporating foods rich in probiotics to support your body’s natural defenses.
Symptoms of Oral Thrush
The typical presentation of oral thrush includes white or yellowish plaques on the mucous membranes of the mouth, particularly on the tongue, inner cheeks, and gums. These patches are often described as creamy or cottage cheese-like in appearance and can be easily scraped off, leaving an inflamed, red area underneath. Patients may experience mild discomfort or significant pain, making eating and drinking difficult.
Additional symptoms can include a burning sensation, soreness, and a feeling of dryness in the mouth.
Risk Factors for Oral Thrush
Several factors increase the susceptibility to oral thrush. A weakened immune system, as mentioned earlier, is a significant risk factor. Individuals undergoing treatment with corticosteroids, such as those used in asthma or other inflammatory conditions, are also at a higher risk. Long-term use of antibiotics disrupts the normal oral flora, creating an environment where Candida can thrive.
Babies, especially those who are breastfed, can be susceptible, especially if there are issues with latching or feeding techniques. Diabetic patients with poorly controlled blood sugar levels may also be more prone to developing oral thrush.
Trying to soothe that pesky oral thrush? While natural remedies like coconut oil can help, a balanced approach might be key. For instance, a high protein, high-fat breakfast, like the ones discussed in this article on how high protein fat breakfast can reduce a1c , could potentially contribute to overall health, indirectly benefiting your body’s ability to fight off infections.
So, keep those soothing remedies handy, but also prioritize a healthy lifestyle, and you might find relief faster.
Differentiating Oral Thrush from Other Oral Conditions
Oral thrush can be mistaken for other oral conditions. While similar-looking white patches might appear in other mouth sores or infections, the presence of red, inflamed tissue beneath the patches is a key indicator of thrush. A proper diagnosis is crucial to ensure the appropriate treatment is administered. A healthcare professional can distinguish between oral thrush and other conditions like leukoplakia, which presents as thick white patches that are not easily scraped off, or oral lichen planus, which can exhibit various symptoms, including white or lacy patterns.
Importance of Proper Diagnosis and When to Seek Professional Help
Accurate diagnosis of oral thrush is essential for effective treatment. Self-treating can delay appropriate care and potentially worsen the condition. If you suspect you have oral thrush, it’s crucial to seek professional medical attention. A healthcare provider can confirm the diagnosis through visual examination and potentially a swab sample for laboratory analysis. Seeking professional help is particularly important for individuals with underlying health conditions, as oral thrush can be a symptom of a more significant issue.
Prompt diagnosis and treatment are crucial for preventing complications and ensuring a faster recovery.
Comparison of Oral Thrush Types
| Type of Oral Thrush | Cause | Severity |
|---|---|---|
| Common Oral Thrush | Weakened immune system, antibiotics, corticosteroids, diabetes | Mild to moderate |
| Oral Thrush in Infants | Immature immune system, breastfeeding issues | Mild to moderate |
| Recurrent Oral Thrush | Underlying health conditions, compromised immune system, poor oral hygiene | Moderate to severe |
This table provides a general overview of different oral thrush types. The severity can vary significantly based on the underlying causes and the individual’s overall health. It’s important to consult with a healthcare professional for proper diagnosis and personalized treatment recommendations.
Home Remedies for Oral Thrush
Oral thrush, a fungal infection in the mouth, can be uncomfortable and sometimes painful. While medical treatment is often necessary for severe cases, several home remedies are sometimes used to alleviate symptoms. It’s crucial to remember that these remedies are not a substitute for professional medical care, especially if the thrush is persistent or worsening. Always consult a healthcare provider for proper diagnosis and treatment.Home remedies for oral thrush often focus on soothing the affected area and potentially supporting the body’s natural defenses.
However, the effectiveness and safety of these remedies vary, and it’s essential to approach them with caution and awareness of potential limitations. A doctor can advise on whether or not a home remedy is appropriate in your specific situation.
Commonly Used Home Remedies
Many individuals try various home remedies to manage the discomfort of oral thrush. These approaches often focus on reducing inflammation and promoting healing. However, the scientific evidence supporting their effectiveness is often limited or inconclusive.
- Saltwater Rinses: A simple yet potentially effective home remedy involves rinsing the mouth with warm saltwater. Saltwater can help to soothe the irritated tissues and may reduce inflammation. The antimicrobial properties of salt may also help to inhibit the growth of the fungus. However, this remedy should not be used excessively, as it can potentially dry out the mouth.
It’s best used as a supplementary measure alongside other treatments.
- Coconut Oil Pulling: This involves swishing coconut oil in the mouth for a short period. Proponents suggest that coconut oil has antimicrobial properties that may help combat the fungal infection. While some anecdotal evidence exists, more rigorous scientific studies are needed to confirm its efficacy against oral thrush.
- Honey: Honey has a long history of use as a natural remedy for various ailments, including oral infections. Some believe its antibacterial and antioxidant properties may contribute to the healing process. While anecdotal evidence suggests potential benefits, rigorous studies are needed to establish its effectiveness for oral thrush.
- Yogurt (Probiotics): Probiotic-rich yogurt may offer some support for the body’s natural defenses. The presence of beneficial bacteria might contribute to a healthier oral environment. However, the effectiveness of yogurt in combating oral thrush needs further investigation.
- Tea Tree Oil: Some people use tea tree oil as a topical remedy. Tea tree oil possesses antimicrobial properties, but it’s crucial to use it with extreme caution. Undiluted tea tree oil can cause significant irritation and should never be applied directly to the affected area without proper dilution and consultation with a healthcare professional.
Effectiveness and Safety Comparison
The table below provides a preliminary comparison of the effectiveness and safety profiles of various home remedies. It’s important to remember that this is not an exhaustive list, and further research is needed to fully understand the efficacy of each remedy.
| Home Remedy | Potential Benefits | Potential Limitations | Scientific Evidence | Safety Profile |
|---|---|---|---|---|
| Saltwater Rinses | Soothes irritated tissues, may reduce inflammation | May dry out the mouth | Limited, anecdotal evidence | Generally safe when used appropriately |
| Coconut Oil Pulling | Potentially antimicrobial | Requires further investigation for efficacy | Limited, anecdotal evidence | Potentially safe when used appropriately |
| Honey | Potential antibacterial and antioxidant properties | Requires further investigation for efficacy | Limited, anecdotal evidence | Generally safe when used appropriately |
| Yogurt (Probiotics) | May support a healthier oral environment | Requires further investigation for efficacy | Limited, anecdotal evidence | Generally safe when used appropriately |
| Tea Tree Oil | Potentially antimicrobial | Highly irritating when undiluted; should not be used without dilution and professional consultation | Limited, anecdotal evidence | Potentially unsafe if used inappropriately |
Importance of Professional Consultation
It’s essential to understand that home remedies are not a replacement for professional medical care. Oral thrush can have various underlying causes, and self-treating without proper diagnosis can delay appropriate treatment. Consulting a healthcare provider is crucial for accurate diagnosis and personalized treatment plans. If symptoms persist or worsen, seek immediate medical attention.
Dietary Recommendations for Oral Thrush: Oral Thrush Home Remedies
Dietary choices play a crucial role in managing oral thrush. Certain foods can either exacerbate the symptoms or contribute to healing. Understanding these dietary interactions can significantly improve comfort and promote a faster recovery. This section delves into specific dietary recommendations for managing oral thrush effectively.The oral environment is a complex ecosystem. The presence of excess yeast,Candida albicans*, can thrive in an environment with specific dietary factors.
A balanced diet can help restore the oral environment, supporting the natural defenses and reducing the growth of yeast.
Foods Potentially Aggravating Oral Thrush
Dietary choices can influence the severity of oral thrush symptoms. Certain foods can create an environment more conducive to yeast growth. It’s crucial to identify these triggers to support healing.
- Sugary foods and drinks are a major concern. High sugar content provides an ideal breeding ground for yeast. Examples include sugary cereals, candies, sodas, and processed foods high in added sugars.
- Foods high in refined carbohydrates like white bread, pastries, and pasta can also exacerbate symptoms. These simple carbohydrates are quickly broken down into sugars, which fuel yeast growth.
- Certain acidic foods and drinks can irritate the already inflamed oral tissues. Examples include citrus fruits, juices, and highly acidic beverages. Their high acidity can disrupt the delicate balance of the oral environment, potentially worsening the condition.
Foods Potentially Alleviating Oral Thrush
While certain foods may exacerbate symptoms, others can contribute to healing and support the body’s natural defenses. A balanced diet rich in beneficial nutrients can aid in restoring oral health.
- Foods rich in probiotics, such as yogurt (with live and active cultures), kefir, and sauerkraut, can help restore the natural balance of oral bacteria, potentially inhibiting yeast overgrowth.
- Foods rich in antioxidants, like berries, dark leafy greens, and colorful fruits, may help reduce inflammation and support overall oral health.
- Foods rich in Vitamin C, like citrus fruits and berries, are known for their immune-boosting properties. A strong immune system can help fight off infections and potentially prevent future episodes.
- Foods rich in zinc, such as oysters, beef, and pumpkin seeds, play a role in immune function and may aid in restoring oral health.
Dietary Impact on Oral Environment and Yeast Growth
The diet directly influences the oral environment. A diet rich in sugars and refined carbohydrates creates an ideal environment for yeast to flourish, leading to increased symptoms. Conversely, a balanced diet with adequate nutrients, probiotics, and antioxidants can support the body’s natural defenses, inhibiting yeast overgrowth.
Dietary Approaches for Managing Oral Thrush
The following table Artikels specific dietary approaches to managing oral thrush. This table highlights potential aggravators and potential remedies for each category.
| Category | Foods to Avoid | Foods to Include |
|---|---|---|
| Sugary Foods | Candy, sugary cereals, sodas, fruit juices, processed foods high in sugar | Fruits (in moderation), vegetables, whole grains |
| Refined Carbohydrates | White bread, pasta, pastries, white rice | Whole grains, brown rice, quinoa, oats |
| Acidic Foods | Citrus fruits (in excess), highly acidic beverages | Milk products, vegetables (in moderation) |
| Probiotic-Rich Foods | Foods lacking in live and active cultures | Yogurt (with live and active cultures), kefir, sauerkraut |
| Nutrient-Rich Foods | Processed foods, junk foods | Fruits, vegetables, whole grains, lean proteins |
Foods to Avoid
To effectively manage oral thrush, it’s essential to avoid foods that exacerbate symptoms.
- Sugary Foods: Candy, sugary cereals, sodas, fruit juices, and processed foods high in sugar.
- Refined Carbohydrates: White bread, pasta, pastries, and white rice.
- Acidic Foods: Citrus fruits (in excess), and highly acidic beverages.
- Highly Processed Foods: Foods high in preservatives and artificial additives, including packaged snacks and fast foods.
Oral Hygiene Practices for Oral Thrush
Oral thrush, a yeast infection in the mouth, can be uncomfortable and even painful. Proper oral hygiene plays a crucial role in preventing and managing this condition. Maintaining a clean mouth is vital to minimizing yeast buildup and reducing the risk of recurrence. Effective oral hygiene practices should be tailored to the individual’s needs and circumstances.
So, you’ve got oral thrush and are looking for some home remedies? While there are many natural ways to treat this common yeast infection, remember that a healthy diet is crucial for overall well-being, including managing your immune system. Finding ways to gain weight with a fast metabolism can also be challenging, but luckily there are strategies to help! how to gain weight with a fast metabolism can be a key part of a balanced approach to oral thrush treatment.
Focus on nutrient-rich foods and consider incorporating foods high in protein and healthy fats. Remember, consistency is key for both weight gain and oral thrush relief.
Effective Oral Hygiene Techniques
Maintaining good oral hygiene is fundamental in preventing and managing oral thrush. A thorough cleaning routine helps eliminate yeast buildup and promotes a healthy oral environment. This includes cleaning the teeth, tongue, and any removable oral appliances.
- Gentle Brushing: Brushing your teeth twice a day with a soft-bristled toothbrush is essential for removing food particles and plaque. Use fluoride toothpaste to strengthen enamel and support overall oral health. Avoid vigorous brushing, which can irritate the affected areas and potentially worsen thrush symptoms.
- Thorough Tongue Cleaning: The tongue often harbors bacteria and yeast. Using a tongue scraper or a soft-bristled toothbrush to gently clean the tongue can help remove these microorganisms. This practice is especially important for individuals prone to oral thrush.
- Regular Mouth Rinsing: Rinsing your mouth with warm salt water or a prescribed mouthwash can help remove excess food particles and reduce inflammation. Follow your doctor’s instructions regarding the frequency and type of mouthwash to use.
Cleaning Removable Appliances
Proper cleaning of removable dental appliances, such as dentures or retainers, is critical to prevent thrush. These appliances can easily harbor yeast, increasing the risk of reinfection.
- Soaking in Solution: Soaking removable appliances in a denture cleaner solution or a mild, soapy water solution is recommended. Follow the manufacturer’s instructions for the denture cleaner. Ensure thorough rinsing before placing the appliance back in the mouth.
- Manual Cleaning: Supplement soaking with manual cleaning using a soft-bristled toothbrush and a mild, soapy solution. Pay close attention to crevices and hard-to-reach areas where plaque and food particles may accumulate.
- Proper Storage: Store removable appliances in a designated, clean container when not in use to prevent bacterial and yeast growth.
Oral Hygiene Practices Summary Table
| Oral Hygiene Practice | Description | Frequency |
|---|---|---|
| Brushing Teeth | Gentle brushing with a soft-bristled toothbrush and fluoride toothpaste | Twice daily |
| Tongue Cleaning | Use a tongue scraper or soft-bristled toothbrush to clean the tongue | Daily |
| Mouth Rinsing | Rinse with warm salt water or prescribed mouthwash | After meals or as directed by a healthcare professional |
| Denture Cleaning | Soak in denture cleaner or mild soapy solution; manually clean | Daily or as directed by a dentist |
Additional Considerations
Maintaining meticulous oral hygiene is paramount to preventing and managing oral thrush. Consider these factors:
- Maintaining good overall health: A healthy immune system plays a crucial role in preventing and managing infections. This includes proper nutrition, adequate sleep, and stress management.
- Consulting a Healthcare Professional: If oral thrush persists despite home remedies, consult a dentist or doctor for appropriate medical care. This is particularly important if thrush symptoms are severe or accompanied by other health concerns.
Natural Remedies and Their Use in Treating Oral Thrush
Oral thrush, a common fungal infection, can be uncomfortable and irritating. While many over-the-counter and prescription treatments are available, some individuals explore natural remedies as potential options. This section explores several natural remedies, their purported benefits, potential risks, and mechanisms of action. However, it’s crucial to remember that these remedies are not always scientifically proven to treat oral thrush, and consulting a healthcare professional is essential for proper diagnosis and treatment.Understanding the potential benefits and risks associated with these remedies is vital before considering them as alternatives to conventional medical care.
It’s important to be aware that many natural remedies haven’t been rigorously tested and may not be effective for everyone.
Potential Natural Remedies for Oral Thrush
Natural remedies for oral thrush, often promoted online, encompass a wide range of substances. However, the scientific evidence supporting their efficacy remains limited. It’s essential to approach these options with caution and under the guidance of a healthcare provider.
- Honey: Honey has demonstrated antimicrobial properties in some studies. Its high sugar content can create an environment less favorable for the growth of Candida albicans, the fungus causing oral thrush. Potential benefits include soothing sore mouth tissues. However, honey is not a cure-all, and its efficacy in treating oral thrush needs further investigation. It should not be given to infants under one year old due to the risk of botulism.
- Coconut Oil: Coconut oil is frequently touted for its purported antimicrobial properties. It is believed to inhibit the growth of Candida, potentially providing relief from oral thrush symptoms. Potential benefits include its moisturizing effects on the oral mucosa. However, more rigorous research is needed to determine its effectiveness in treating oral thrush. It’s also important to note that the amount of lauric acid in coconut oil that might be responsible for its antimicrobial properties might be diluted when applied topically.
- Tea Tree Oil: Tea tree oil has shown some antibacterial and antifungal properties in laboratory settings. Topical application might provide temporary relief from symptoms. However, it’s crucial to dilute tea tree oil significantly before applying it to the mouth due to its potential for causing oral irritation. Direct application of undiluted tea tree oil can cause significant harm.
- Probiotics: Probiotics, beneficial bacteria, are believed to restore the balance of oral flora. Maintaining a healthy oral microbiome might help prevent fungal overgrowth. Potential benefits include supporting overall oral health. However, more research is necessary to determine the effectiveness of specific probiotic strains in combating oral thrush. Probiotics are not a substitute for conventional medical care for thrush.
Mechanism of Action and Reported Effectiveness, Oral thrush home remedies
The mechanisms by which these remedies purportedly combat oral thrush are diverse. Some are thought to create an environment less conducive to fungal growth, while others directly target the fungus. The reported effectiveness of these remedies is often anecdotal, and scientific validation is still needed.
| Remedy | Ingredients | Method of Application | Reported Effectiveness |
|---|---|---|---|
| Honey | Honey | Swallowing small amounts of honey or applying it topically to the affected area | Potentially soothing and may create an environment less favorable for fungal growth, but not proven as a sole treatment |
| Coconut Oil | Coconut oil | Applying a small amount of coconut oil to the affected area | Potentially helpful due to its purported antimicrobial properties, but more research is required |
| Tea Tree Oil | Tea tree oil | Applying a diluted solution of tea tree oil to the affected area | Some anecdotal evidence suggests it might provide temporary relief, but significant dilution is needed to prevent oral irritation |
| Probiotics | Beneficial bacteria | Consuming probiotic supplements or foods containing probiotics | Potentially supportive for oral health, but not a proven treatment for oral thrush |
Caution Regarding Unproven Treatments
It’s crucial to exercise caution when considering unproven or experimental treatments for oral thrush. Self-treating with natural remedies might delay or prevent appropriate medical care, potentially worsening the condition. Always consult a healthcare professional for proper diagnosis and treatment of oral thrush. Seeking professional guidance is crucial to ensure the best possible outcome.
Prevention Strategies for Oral Thrush
Oral thrush, a common yeast infection, can recur if not managed properly. Understanding the contributing factors and implementing preventive measures are crucial for long-term oral health and well-being. This section explores effective strategies to minimize the risk of thrush recurrence and maintain a healthy oral environment.Preventing oral thrush involves a multifaceted approach encompassing good oral hygiene, dietary considerations, and immune system support.
By addressing potential risk factors and adopting proactive measures, individuals can significantly reduce the likelihood of experiencing this uncomfortable condition.
Maintaining Oral Hygiene Practices
Proper oral hygiene plays a pivotal role in preventing oral thrush. Consistent and thorough cleaning helps remove food particles and plaque, reducing the environment conducive to yeast overgrowth.
- Regular brushing and flossing are essential to remove food debris and bacteria. This helps maintain a clean oral cavity, minimizing the ideal environment for yeast to thrive.
- Using a soft-bristled toothbrush and gentle brushing technique is crucial to avoid damaging the delicate tissues of the mouth, especially in individuals prone to thrush.
- Regularly rinsing the mouth with water or a mouthwash can help dislodge food particles and bacteria. Rinsing can provide a refreshing and hygienic oral environment.
Dietary Considerations for Prevention
A balanced diet rich in nutrients supports overall health, including a robust immune system. This, in turn, can help combat yeast infections like thrush.
- A diet rich in fruits, vegetables, and whole grains provides essential vitamins and minerals that bolster the immune system.
- Maintaining a healthy weight through balanced nutrition is also important for optimal immune function. Obesity can weaken the immune system, making individuals more susceptible to yeast infections.
- Reducing or eliminating sugary foods and drinks is crucial, as these provide an ideal environment for yeast growth. Sugary foods and drinks can exacerbate yeast overgrowth.
Strengthening the Immune System
A strong immune system is a vital defense against various infections, including oral thrush. Several strategies can help bolster immune function.
- Getting sufficient sleep is essential for immune system function. Adequate sleep allows the body to repair and regenerate, contributing to a healthy immune response.
- Regular exercise contributes to overall health and can strengthen the immune system. Physical activity plays a significant role in maintaining a healthy immune response.
- Stress management techniques, such as meditation or deep breathing exercises, can help reduce stress hormones that can negatively impact the immune system.
Risk Mitigation During Medical Treatments
Certain medical treatments can increase the risk of oral thrush. Proactive measures can help reduce this risk.
- Individuals undergoing antibiotic therapy are more susceptible to thrush due to the disruption of the oral microbiome. Taking probiotics during antibiotic use can help restore the balance of oral bacteria and reduce the risk.
- Patients using corticosteroids, particularly those taken orally, can experience a suppressed immune response, making them more vulnerable to yeast infections. Following the prescribed dosage and duration of corticosteroid use is important to minimize the risk.
- Individuals with weakened immune systems, such as those with HIV/AIDS, are at a higher risk of oral thrush. Maintaining close communication with healthcare providers and promptly reporting any signs or symptoms of infection is essential for appropriate management.
Identifying and Mitigating Risk Factors
Certain situations can increase the risk of oral thrush. Recognizing and mitigating these factors can help prevent recurrence.
- Individuals with diabetes, due to the elevated blood sugar levels, are more prone to oral thrush. Proper blood sugar management can help reduce the risk.
- People who wear dentures or have ill-fitting dental appliances can experience increased risk. Maintaining good oral hygiene and proper care for dental appliances can reduce the risk.
- Frequent use of mouthwashes containing alcohol can disrupt the natural oral flora, increasing the risk of yeast overgrowth. Choosing alcohol-free mouthwashes can help maintain a healthy oral environment.
Illustrations of Oral Thrush and Related Conditions
Understanding the visual presentation of oral thrush and related conditions is crucial for early diagnosis and effective treatment. Accurate identification allows for timely intervention and prevents the spread of infection. Visual aids play a vital role in this process.Visual cues are often the first indicators of a potential issue. Recognizing the symptoms allows for early intervention, which can significantly improve the overall outcome.
Differentiating between healthy and affected oral tissues is important, and these illustrations will help in that process.
Appearance of Oral Thrush in Different Stages
Oral thrush typically progresses through stages, with each characterized by distinct visual patterns. Initial stages often show subtle changes, making early detection challenging.
- Early Stage: Small, white or yellowish patches appear on the tongue, inner cheeks, or the roof of the mouth. These patches may be slightly raised and have a creamy or slightly granular texture. They are often described as resembling cottage cheese. The affected areas may be tender to the touch, but pain is often not significant in this stage.
- Moderate Stage: The white patches expand, possibly merging to form larger, more pronounced areas. The patches may become thicker and more adherent to the underlying tissues, making them difficult to remove. Oral discomfort, including mild pain and soreness, may become more noticeable. At this stage, there might be some redness or inflammation around the patches.
- Advanced Stage: Extensive areas of the mouth are covered with thick white patches. The affected tissues may exhibit significant inflammation and redness, particularly around the patches. The affected areas may be quite painful, and the individual may experience difficulty swallowing or eating.
Visual Difference Between Healthy and Affected Oral Tissues
Healthy oral tissues are typically a light pink or a slightly reddish color. The surface appears smooth and even, without any visible lesions or discolorations. In contrast, oral thrush presents as white or yellowish patches on the affected tissues. The affected areas often appear raised or thickened compared to the surrounding healthy tissues.
Illustrations of Oral Hygiene Tools and Techniques
Proper oral hygiene is critical in preventing and managing oral thrush. Using the correct tools and techniques can significantly reduce the risk of infection.
- Soft-bristled Toothbrush: A soft-bristled toothbrush is essential for gentle cleaning. Illustrations should depict correct brushing techniques, focusing on brushing the affected areas without causing further irritation. It should also show proper brushing techniques around the gum line and tongue.
- Anti-Thrush Mouthwash: Illustrations should depict the correct usage of anti-thrush mouthwash, including how to swish and hold it in the mouth. Proper rinsing techniques should be emphasized to ensure the mouthwash reaches all affected areas.
- Tongue Scraper: A tongue scraper can help remove any accumulated debris or bacteria that may contribute to thrush. Illustrations should demonstrate how to use a tongue scraper effectively and gently to prevent further irritation.
Visual Aids for Understanding Causes, Symptoms, and Remedies
A comprehensive set of visual aids can significantly enhance understanding of oral thrush.
| Category | Visual Aid Description |
|---|---|
| Causes | Illustrations depicting common factors that increase the risk of oral thrush, such as weakened immune systems, antibiotic use, and poor oral hygiene. Infographics showcasing the relationship between these factors and thrush development. |
| Symptoms | Detailed diagrams showing different stages of oral thrush, highlighting the visual characteristics and severity of each stage. Illustrations of other conditions that can mimic oral thrush, such as oral lichen planus or leukoplakia. |
| Remedies | Illustrations depicting different types of antifungal medications, both topical and systemic, with detailed explanations of their usage. Visuals demonstrating the proper application of topical treatments. |
Final Thoughts

In conclusion, oral thrush home remedies provide a range of potential solutions for managing the discomfort and managing the infection. Remember, while these remedies can be helpful, consulting a healthcare professional is crucial for proper diagnosis and to ensure these remedies are safe and effective for your specific situation. Maintaining good oral hygiene and a balanced diet plays a significant role in preventing future outbreaks.