How could I not know that I had PCOS until adulthood? This journey explores the often-delayed diagnosis of Polycystic Ovary Syndrome (PCOS) in women. We’ll delve into why diagnosis might be delayed, the impact of this delay on health outcomes, and strategies for improving early detection. Many women experience a range of symptoms, some subtle,…
Tag: women’s health
Turmeric Health Benefits for Women A Deep Dive
Turmeric health benefits for women are plentiful and fascinating, offering a natural approach to overall well-being. From hormonal balance to digestive health, bone strength, skin radiance, and immune support, turmeric’s active compound, curcumin, appears to play a key role in various aspects of women’s health. This exploration delves into the science behind turmeric’s effects, highlighting…
Ovarian Pain Causes and Treatment Explained
Ovary pain causes and treatment – Ovarian pain causes and treatment is a complex issue affecting many women. Understanding the intricacies of the female reproductive system, the various potential causes of discomfort, and the available treatment options is crucial for effective management. This exploration delves into the different types of ovarian pain, their potential origins,…
Nkem Osians Uterine Fibroid Story A Personal Account
Nkem osian uterine fibroid story – Nkem Osian’s uterine fibroid story is a powerful account of navigating a health challenge with resilience and grace. This journey delves into the personal experiences, medical treatments, and societal factors surrounding uterine fibroids. From understanding the condition itself to exploring the emotional and practical impacts, this narrative offers a…
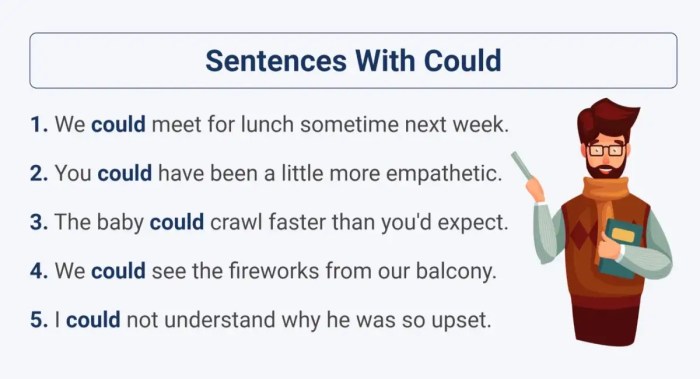
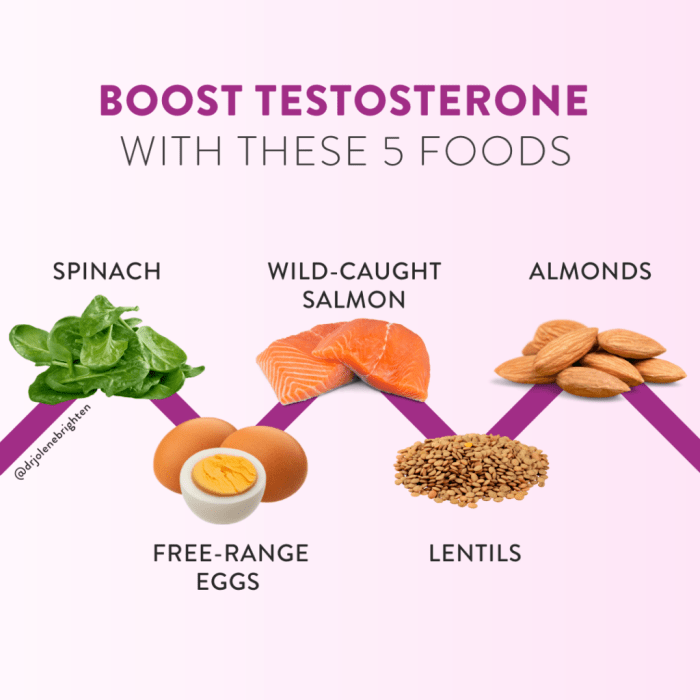
Low Testosterone in Women A Deep Dive
Low testosterone in women sets the stage for this enthralling narrative, offering readers a glimpse into a complex hormonal landscape. We’ll explore the intricacies of low testosterone levels in women, delving into its various definitions, measurement methods, and the diverse factors that influence them. From understanding the typical ranges to identifying potential symptoms and underlying…
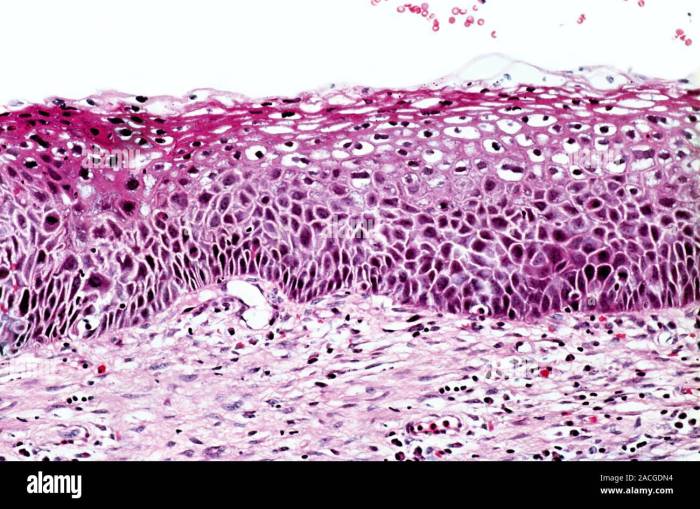
What is Cervical Intraepithelial Neoplasia? A Deep Dive
What is cervical intraepithelial neoplasia (CIN)? This condition, often linked to HPV, represents abnormal cell growth on the cervix. Understanding its various grades, from CIN 1 to CIN 3, is crucial for early detection and effective management. This blog post delves into the specifics of CIN, exploring its causes, diagnosis, treatment options, and preventative strategies….
What to Eat on Your Period A Guide
What to eat on your period? This isn’t just about cravings; it’s about understanding your body’s unique needs during menstruation. From boosting energy levels to easing discomfort, the right foods can make a real difference. This guide dives deep into the nutritional needs of your cycle, offering practical advice and delicious meal ideas. We’ll explore…
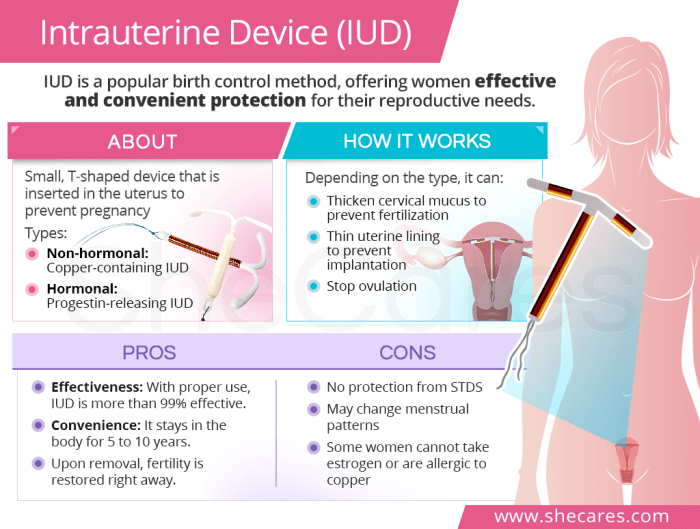
Pros and Cons of IUD A Comprehensive Guide
Pros and cons of IUD: This comprehensive guide dives deep into the world of intrauterine devices (IUDs), exploring their various types, advantages, potential drawbacks, and crucial factors to consider before choosing one. We’ll examine the effectiveness, convenience, and potential side effects, equipping you with the knowledge to make an informed decision about your reproductive health….
Yeast Infection vs UTI Understanding the Differences
Yeast infection vs UTI: This guide delves into the often-confused conditions of yeast infections and urinary tract infections (UTIs). We’ll explore their distinct symptoms, causes, and treatment approaches, helping you understand the key differences and how to approach diagnosis and care. Knowing the specifics is crucial for getting the right treatment. From common symptoms like…
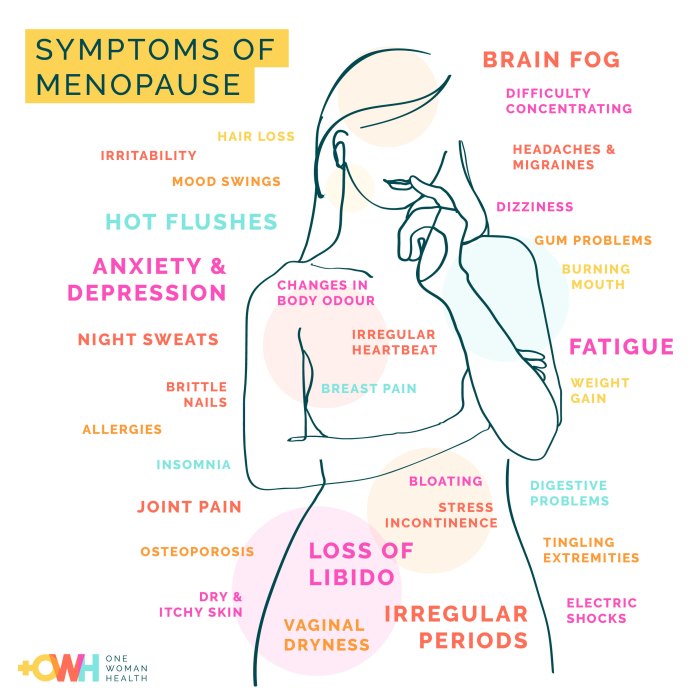
Menopause Fatty Liver Disease Risk A Deep Dive
Menopause fatty liver disease risk is a growing concern for women as they transition through this life stage. Hormonal shifts during menopause can significantly impact liver health, potentially increasing the likelihood of developing fatty liver disease. This comprehensive guide explores the underlying mechanisms, risk factors, diagnostic methods, and management strategies associated with this condition. We’ll…