Too much vitamin D, while crucial for bone health, can be detrimental if not managed properly. This comprehensive guide delves into the dangers of excessive vitamin D intake, exploring the defining factors, potential sources, and the serious implications for various demographics. We’ll uncover the symptoms, risk factors, and crucial strategies for prevention and management.
Understanding the recommended daily intake, different units of measurement, and how various sources contribute to overall vitamin D levels is key. We’ll also examine the specific risks to different populations, providing practical advice for maintaining healthy vitamin D levels.
Defining “Too Much” Vitamin D
Vitamin D is crucial for maintaining healthy bones and immune function, but like any nutrient, excessive intake can lead to adverse health effects. Understanding what constitutes “too much” vitamin D is essential for maintaining optimal health. This involves not only knowing the recommended daily intake but also recognizing the different units of measurement and the potential risks associated with exceeding those guidelines.Excessive vitamin D intake, also known as hypervitaminosis D, occurs when the body absorbs and retains more vitamin D than it needs.
This surplus can accumulate in the body, leading to a buildup of the vitamin, resulting in a range of potential health problems.
Defining Excessive Vitamin D Intake
Excessive vitamin D intake is characterized by blood levels of vitamin D exceeding the healthy range. This typically manifests as elevated serum 25-hydroxyvitamin D levels. Different medical organizations and guidelines use various thresholds to define what constitutes a high level, but generally, levels above a certain range, as defined by laboratory testing, are considered excessive.
Units of Measurement
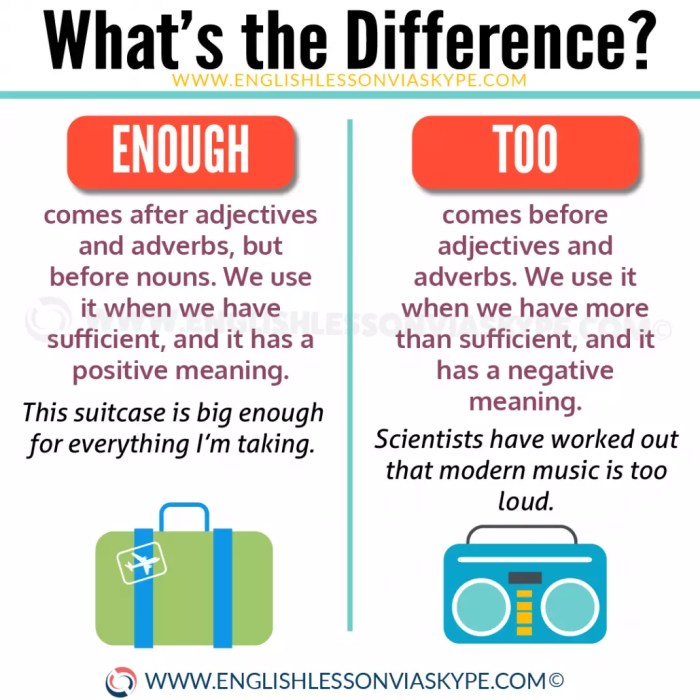
Vitamin D is measured in two primary units: micrograms (mcg) and International Units (IU). While both units represent the same substance, they differ in their relative values. 1 mcg of vitamin D is equivalent to approximately 40 IU. Conversion between these units is crucial for accurate interpretation of dietary supplements and blood test results.
Recommended Daily Intake (RDI), Too much vitamin d
The recommended daily intake (RDI) of vitamin D varies significantly across different age groups and populations due to factors like sun exposure, dietary habits, and overall health. The RDI serves as a guideline to ensure adequate vitamin D levels without risking hypervitaminosis D.
RDI and Potential Risks
The following table provides a comparison of the RDI for different age groups and Artikels potential risks associated with exceeding the recommended intake. It is important to note that these are general guidelines, and individual needs may vary. Consulting with a healthcare professional is crucial for personalized recommendations.
| Age Group | RDI (mcg) | Potential Risks (brief description) |
|---|---|---|
| Infants (0-12 months) | 10 | Elevated calcium levels, kidney stones, nausea, vomiting, constipation. |
| Children (1-13 years) | 15 | Similar to infants, but potential for impaired growth and development if chronic. |
| Adults (19-70 years) | 15 | Similar to children, but with an increased risk of kidney damage and impaired kidney function. |
| Adults (71+ years) | 20 | Similar to other groups, but with an increased susceptibility to kidney problems and impaired bone health due to aging. |
Sources of Excessive Vitamin D Intake

Vitamin D, crucial for bone health and immune function, can be easily obtained through various dietary sources and sun exposure. However, excessive intake, especially from supplements, can lead to hypervitaminosis D, a potentially serious condition. Understanding the different avenues of vitamin D acquisition is key to maintaining optimal levels and avoiding toxicity.Dietary sources and supplement dosages can significantly impact vitamin D levels.
Overconsumption from these sources can surpass the body’s capacity to utilize or excrete the vitamin, resulting in elevated blood levels. The interplay between dietary intake, supplementation, and sun exposure needs careful consideration to prevent potential harm.
Dietary Sources of Vitamin D
A balanced diet plays a vital role in maintaining optimal vitamin D levels. While many foods contain vitamin D in varying amounts, some are naturally richer sources than others. Fatty fish, like salmon, tuna, and mackerel, are excellent dietary sources. Egg yolks and fortified foods like milk and cereals also contribute to daily vitamin D intake. However, the amounts provided by these sources are generally not sufficient to cause overconsumption on their own, unless consumed in extremely large quantities.
Vitamin D Supplements and Dosage
Vitamin D supplements are readily available in various forms and dosages. The dosage on these supplements is crucial, as excessive intake can lead to hypervitaminosis D. People with specific medical conditions, such as kidney problems, may require lower doses or more frequent monitoring. Carefully following recommended dosages is essential to avoid overconsumption. High doses of vitamin D supplements can quickly lead to excessive levels, even if taken for a short period.
While too much vitamin D is generally a less common concern than a deficiency, it can still lead to some unwanted side effects. One surprising effect is its potential impact on oral health. High levels can sometimes contribute to issues like gum inflammation, which can make getting rid of gingivitis more challenging. Fortunately, there are many effective ways to combat this inflammation.
Check out this guide for more detailed information on how to get rid of gingivitis: how to get rid of gingivitis. Ultimately, maintaining a healthy balance of vitamin D is key for overall well-being, including keeping your smile bright and gums healthy.
Sun Exposure and Vitamin D Production
Sunlight is a significant source of vitamin D. The body can synthesize vitamin D when exposed to ultraviolet B (UVB) rays. However, excessive sun exposure can pose risks, including skin damage and an increased risk of skin cancer. Factors like skin pigmentation, time of day, and geographic location influence vitamin D production from sun exposure. Balancing the benefits of vitamin D synthesis with the risks of sun exposure is critical.
Different Vitamin D Supplement Forms
Various forms of vitamin D supplements exist, each with its absorption characteristics. Cholecalciferol (vitamin D3) is the most common form, often considered the body’s preferred form. Ergocalciferol (vitamin D2) is another form, but its absorption and metabolism may differ from vitamin D3. The different forms of vitamin D supplements can have varying effects on the body, so it’s essential to be aware of the form and potential impact on individual vitamin D levels.
Symptoms and Effects of Vitamin D Toxicity
Vitamin D is crucial for bone health and overall well-being, but excessive intake can lead to a range of adverse effects. Understanding the potential symptoms and long-term consequences of vitamin D toxicity is vital for maintaining optimal health and preventing complications. It’s important to note that these effects are often dose-dependent and vary significantly from person to person.High levels of vitamin D in the body can disrupt various bodily functions, leading to a spectrum of symptoms, some of which can be subtle or easily overlooked.
Early detection and prompt intervention are key to mitigating potential harm.
Early Signs of Vitamin D Toxicity
Excessive vitamin D intake, typically from supplements, can manifest in various early symptoms. These symptoms often resemble those of other conditions, making diagnosis challenging.Common early symptoms include nausea, vomiting, and loss of appetite. These gastrointestinal issues can significantly impact daily life and overall well-being. Other early indicators may include increased thirst, frequent urination, and constipation. These symptoms, if persistent, warrant medical attention to determine the underlying cause.
Potential Long-Term Effects of Vitamin D Toxicity
Prolonged exposure to high levels of vitamin D can result in significant long-term complications. These complications can impact various bodily systems and have far-reaching consequences for overall health.One potential long-term effect is kidney damage. High vitamin D levels can lead to calcium deposits in the kidneys, potentially impairing their function and causing long-term complications like kidney stones or even kidney failure.
Furthermore, excessive vitamin D can disrupt the balance of calcium in the body, potentially causing calcification in soft tissues like blood vessels, heart valves, and lungs. This can lead to significant issues such as heart problems or lung disease. The impact of excessive vitamin D on these systems can be substantial and require careful monitoring and management.
Correlation Between Vitamin D Levels and Potential Symptoms
The following table illustrates the potential correlation between vitamin D levels (in ng/mL) and associated symptoms. It’s important to remember that this table provides a general guideline and individual responses may vary.
| Vitamin D Level (ng/mL) | Symptoms |
|---|---|
| >150 | Nausea, vomiting, loss of appetite, increased thirst, frequent urination, constipation, weakness, headache, confusion, and potentially kidney problems. |
| >100 | Nausea, vomiting, loss of appetite, increased thirst, and frequent urination. |
| >80 | Mild symptoms may appear, such as nausea and fatigue. |
| 60-80 | Normal range; no toxicity symptoms are expected. |
Risk Factors for Vitamin D Toxicity: Too Much Vitamin D
Vitamin D, crucial for bone health and immune function, can become detrimental if consumed in excessive amounts. Understanding the individuals and factors predisposed to vitamin D toxicity is vital for preventative measures. Recognizing these risk factors empowers proactive management of vitamin D levels and minimizes the chances of developing this condition.Identifying those at higher risk of vitamin D toxicity is important for preventative measures.
Factors such as dietary habits, certain medical conditions, and genetic predispositions play significant roles. By understanding these influences, individuals can make informed choices about their vitamin D intake and seek appropriate medical advice when needed.
Individuals More Susceptible
Certain groups are inherently more vulnerable to vitamin D toxicity. These include individuals with underlying health conditions that can impact vitamin D metabolism, as well as those who consume high doses of vitamin D supplements without proper medical guidance. Additionally, infants and young children, if given excessive doses, are particularly susceptible to the harmful effects of vitamin D toxicity.
Pre-existing Medical Conditions
Certain medical conditions can interact negatively with vitamin D, increasing the risk of toxicity. For instance, kidney disease can impair the body’s ability to process vitamin D, leading to elevated blood levels. Similarly, some liver diseases can disrupt the metabolism of vitamin D, potentially resulting in excessive accumulation. Furthermore, individuals with hyperparathyroidism, a condition characterized by elevated parathyroid hormone levels, may be more prone to vitamin D toxicity due to increased calcium absorption.
While too much vitamin D is generally less common than a deficiency, it can still cause some serious issues. High levels can disrupt various bodily functions, including potentially impacting the delicate balance of your ophthalmic nerve anatomy function and significance. Understanding how these nerves work is key, as outlined in this excellent resource: ophthalmic nerve anatomy function and significance.
This underscores the importance of maintaining a healthy vitamin D level for overall well-being, preventing potential problems like nerve dysfunction.
Role of Genetics in Vitamin D Metabolism
Genetic variations can significantly influence how the body metabolizes and absorbs vitamin D. Some individuals may possess genetic predispositions that affect the activity of enzymes involved in vitamin D metabolism, making them more susceptible to toxicity. This highlights the importance of personalized approaches to vitamin D supplementation, tailoring recommendations to individual genetic profiles. For example, variations in the CYP2R1 gene, which plays a crucial role in vitamin D metabolism, have been linked to altered vitamin D processing.
Importance of Regular Blood Tests
Regular blood tests to monitor vitamin D levels are essential for proactive health management. These tests provide valuable insights into the body’s vitamin D status, enabling timely interventions if levels become excessively high. The frequency of these tests is determined by individual factors, including medical history, dietary habits, and the use of vitamin D supplements. This proactive approach ensures that individuals receive personalized guidance on their vitamin D intake and prevent the development of toxicity.
Furthermore, a blood test can detect potential issues with vitamin D metabolism before they manifest as symptoms.
Diagnosis and Management of Vitamin D Toxicity
Vitamin D toxicity, while less common than deficiency, can still pose health risks. Understanding how to diagnose and manage elevated vitamin D levels is crucial for preventing complications and ensuring optimal health. Early detection and appropriate intervention are vital in mitigating the negative effects of excessive vitamin D.
So, you’ve been taking extra vitamin D, thinking it’s a super boost for your health. But did you know that too much of a good thing can be problematic? This excess can actually impact your foot health, affecting the complex structure and function of your bones and muscles, which is why understanding foot anatomy and physiology here is crucial.
High vitamin D levels can lead to calcification issues, potentially impacting the delicate balance of your foot’s support system. It’s important to monitor your intake and consult with a doctor to avoid any unwanted side effects from too much vitamin D.
Diagnostic Methods for Vitamin D Toxicity
Identifying vitamin D toxicity involves a multi-step process. Blood tests are the cornerstone of diagnosis. Measuring serum 25-hydroxyvitamin D levels is essential. Elevated levels, often exceeding 150 ng/mL, can indicate toxicity. However, a single test may not be conclusive, as individual variations exist.
Additional tests might include parathyroid hormone (PTH) levels, which could provide insight into the body’s response to high vitamin D. Furthermore, a thorough medical history and physical examination are essential to evaluate any symptoms and potential underlying conditions that might contribute to the elevated levels. A comprehensive assessment considers factors like diet, supplements, and overall health.
Treatment Strategies for Managing Excessive Vitamin D Levels
Managing vitamin D toxicity involves reducing vitamin D intake and addressing symptoms. The primary approach is to discontinue all vitamin D supplements immediately. Dietary modifications that limit vitamin D-rich foods are also important. In severe cases, medical professionals might recommend medications to help the body eliminate excess vitamin D. This could involve using medications that can bind and excrete vitamin D from the body.
Monitoring the levels of vitamin D through regular blood tests is essential to track the effectiveness of the treatment. Symptoms will be addressed through supportive care, tailored to the specific manifestation of the toxicity.
Role of Medical Professionals in Assessing and Managing Vitamin D Toxicity
Medical professionals play a critical role in assessing and managing vitamin D toxicity. Physicians must conduct a thorough evaluation, including a review of medical history, physical examination, and blood tests. They need to assess the patient’s individual risk factors and the severity of the toxicity. The treatment plan should be individualized, considering the specific needs of the patient.
Regular follow-up appointments are necessary to monitor the patient’s progress and adjust the treatment plan as needed. Healthcare professionals should emphasize the importance of appropriate vitamin D intake and the potential risks associated with excessive supplementation. They can educate patients about the importance of maintaining healthy vitamin D levels through a balanced diet and appropriate supplementation guidance.
Reducing Vitamin D Intake
Reducing vitamin D intake when levels are too high requires careful consideration. Stopping all vitamin D supplements is the first step. Modifying the diet to limit vitamin D-rich foods, such as fatty fish and fortified foods, is also essential. It’s crucial to remember that sunlight exposure contributes to vitamin D synthesis. Limiting sun exposure is not a practical solution for reducing vitamin D intake in cases of toxicity, as the amount of vitamin D produced through sun exposure is typically insignificant compared to supplementation.
However, it can be a helpful part of overall healthy lifestyle recommendations. Consult with a healthcare professional to discuss specific dietary changes and adjust vitamin D intake based on the patient’s individual circumstances.
Prevention of Vitamin D Toxicity
Vitamin D toxicity, while rare, is a serious concern. Proactively preventing it is crucial for maintaining overall health. This involves understanding the recommended intake levels, supplement use, and the importance of regular monitoring. By taking proactive steps, individuals can significantly reduce the risk of experiencing this potentially harmful condition.
Importance of Following Recommended Dietary Guidelines
A balanced diet is the cornerstone of optimal vitamin D intake. Consuming foods rich in vitamin D, such as fatty fish (salmon, tuna), egg yolks, and fortified dairy products, contributes to meeting daily needs without the risk of exceeding safe limits. Moderation is key. Avoiding excessive consumption of these foods, especially those high in fat, is vital to preventing potential toxicity.
For example, consuming multiple servings of fatty fish daily could lead to vitamin D accumulation.
Need for Appropriate Supplement Usage
Vitamin D supplements can be beneficial for those with insufficient dietary intake, but careful attention to dosage is paramount. Individuals considering supplements should consult with their healthcare provider to determine the appropriate dosage and frequency. The recommended daily allowance (RDA) should be strictly adhered to. Overdosing through supplements is a common cause of vitamin D toxicity. For instance, taking high-dose vitamin D supplements without medical supervision could lead to hypervitaminosis D.
Necessity of Regular Monitoring of Vitamin D Levels
Regular blood tests to monitor vitamin D levels are crucial for individuals who supplement or have underlying health conditions that affect vitamin D metabolism. These tests help identify potential imbalances and allow for prompt adjustments to prevent toxicity. This proactive approach ensures that vitamin D levels remain within the safe range. For example, individuals with kidney disease may need more frequent monitoring as their bodies process vitamin D differently.
Following recommended dietary guidelines, using supplements appropriately, and regularly monitoring vitamin D levels are crucial preventative measures to avoid vitamin D toxicity. Understanding these preventive measures empowers individuals to maintain healthy vitamin D status without the risk of adverse effects.
Illustrative Cases of Vitamin D Toxicity
Vitamin D, crucial for bone health and immune function, can become detrimental when taken in excessive amounts. Understanding real-world scenarios of vitamin D toxicity is vital for preventative measures and effective treatment. This section delves into illustrative cases, highlighting the symptoms, diagnoses, and management strategies, emphasizing the importance of responsible supplementation and regular monitoring.
Real-World Examples of Vitamin D Toxicity
Excessive vitamin D intake, often stemming from high-dose supplements, can lead to a range of health problems. These cases underscore the importance of adhering to recommended dietary allowances and consulting healthcare professionals before initiating any supplementation regimen.
| Case Study | Symptoms | Diagnosis | Treatment |
|---|---|---|---|
| A 50-year-old male, with a history of osteoporosis, took high-dose vitamin D supplements (over 10,000 IU daily) for several months to boost bone density. He experienced severe nausea, vomiting, and persistent thirst. He also reported weakness and frequent urination. | Nausea, vomiting, persistent thirst, weakness, frequent urination, and anorexia. | Elevated serum vitamin D levels (significantly above the normal range) and calcium levels (hypercalcemia). Blood tests revealed kidney dysfunction. | Immediate cessation of vitamin D supplements. Intravenous fluids to manage dehydration and electrolyte imbalances. Medications to lower blood calcium levels (e.g., bisphosphonates or calcitonin) and to support kidney function. Close monitoring of serum vitamin D and calcium levels. |
| A 20-year-old female, avidly taking vitamin D supplements (10,000 IU daily) with no medical consultation, experienced severe abdominal pain, and was diagnosed with kidney stones. She also reported muscle weakness and confusion. | Severe abdominal pain, kidney stones, muscle weakness, confusion, and fatigue. | Elevated serum vitamin D and calcium levels. Imaging studies (e.g., X-rays, CT scans) confirmed the presence of kidney stones. | Discontinuation of vitamin D supplements. Hydration therapy to aid in kidney stone passage. Medications to manage calcium levels and prevent further stone formation. Dietary changes to minimize calcium intake and encourage hydration. |
| A 65-year-old woman, taking vitamin D supplements for several years as part of a holistic wellness regimen, experienced bone pain, severe itching, and frequent falls. She was also diagnosed with kidney disease. | Bone pain, severe itching, frequent falls, kidney disease, and mental confusion. | Elevated serum vitamin D and calcium levels, along with laboratory evidence of kidney impairment. | Immediate cessation of vitamin D supplements. Fluid therapy, along with medications (e.g., calcitonin or bisphosphonates) to lower calcium levels. Dialysis or other renal support as needed. Careful monitoring of vitamin D and calcium levels, and management of underlying kidney issues. |
Importance of Careful Monitoring and Dosage
Regular monitoring of vitamin D levels, particularly when taking supplements, is crucial. Blood tests can assess the level of vitamin D in the body. This ensures that supplementation remains within the recommended range and avoids potential toxicity. The dosage should always be determined by a healthcare professional, considering individual needs and health conditions. A healthcare provider can advise on the appropriate dosage and frequency, tailored to the individual’s circumstances.
Impact on Different Populations
Vitamin D, crucial for bone health and immune function, is essential for all age groups. However, the body’s ability to process and utilize vitamin D, and the susceptibility to its toxic effects, varies significantly across populations. Understanding these differences is vital for appropriate supplementation and preventative measures. This section delves into the specific needs and risks associated with various demographics, such as children, the elderly, and pregnant women.The requirements for vitamin D and the potential for toxicity vary considerably between populations due to factors like metabolism, body composition, and overall health status.
These variations demand tailored approaches to vitamin D supplementation and monitoring, ensuring optimal health benefits without the adverse effects of toxicity.
Vitamin D Needs and Toxicity Risks in Children
Children are a vulnerable population, as their growing bones and developing immune systems rely heavily on adequate vitamin D levels. However, excessive vitamin D intake can disrupt bone growth and mineralization. Infants and young children are particularly susceptible to vitamin D toxicity due to their rapid bone development. Over-supplementation can lead to hypercalcemia, a condition characterized by abnormally high calcium levels in the blood.
This can result in a range of health problems, including kidney stones, digestive issues, and even cardiac complications. Regular monitoring of vitamin D levels in children, especially those receiving supplements, is crucial to prevent toxicity.
Vitamin D Needs and Toxicity Risks in the Elderly
Older adults often experience a decline in vitamin D production and absorption, making them more susceptible to vitamin D deficiency. This deficiency can lead to bone loss, increasing the risk of fractures. However, the elderly are also more prone to the negative effects of excessive vitamin D intake. Their kidneys might not process vitamin D efficiently, increasing the risk of hypercalcemia and its associated complications.
This highlights the importance of careful monitoring and appropriate supplementation strategies in older adults.
Vitamin D Needs and Toxicity Risks in Pregnant Women
During pregnancy, the mother’s body needs increased vitamin D to support fetal bone development and overall health. While adequate vitamin D is crucial for both the mother and the developing fetus, excessive intake can pose risks to both. Hypercalcemia in pregnant women can lead to various complications, including premature birth, preeclampsia, and potential long-term health issues for the child.
Maintaining optimal vitamin D levels is paramount during pregnancy, but it should always be under the guidance of a healthcare professional.
Comparison Table
| Population | Vitamin D Needs | Toxicity Risk |
|---|---|---|
| Children (infants and young children) | Lower than adults, varies with growth stage | High; rapid bone development makes them more vulnerable to hypercalcemia. |
| Elderly | Potentially higher due to decreased vitamin D production and absorption | High; impaired kidney function can hinder vitamin D metabolism, increasing the risk of hypercalcemia. |
| Pregnant Women | Increased needs for fetal development | Moderate; potential for complications for both mother and fetus. |
Final Summary
In conclusion, navigating the complexities of vitamin D levels requires careful attention to recommended intakes, supplement usage, and regular monitoring. This in-depth exploration highlights the importance of understanding the risks associated with too much vitamin D and provides practical steps to prevent and manage potential toxicity. Remember, consulting with a healthcare professional is essential for personalized guidance.