Dry eyes after cataract surgery is a common issue, and understanding the reasons behind it, the symptoms, and effective treatments is crucial for a smooth recovery. This guide delves into the various aspects of dry eye syndrome following cataract surgery, from the initial onset to long-term management.
Cataract surgery, while improving vision, can disrupt the delicate balance of tear production and drainage, leading to dry eye symptoms. This article examines the prevalence, typical timeline, and underlying mechanisms of this post-surgical complication.
Dry Eyes After Cataract Surgery
Post-cataract surgery, many patients experience dry eye syndrome. This is a common complication, and understanding its prevalence, timeline, and contributing factors is crucial for proactive management. Proper knowledge empowers both patients and surgeons to address this issue effectively.Dry eye, a significant post-surgical concern, can significantly impact a patient’s quality of life. The discomfort and potential for vision impairment necessitate careful attention to the factors that influence its development and management strategies.
Prevalence of Dry Eye After Cataract Surgery
Dry eye syndrome is a frequent post-cataract surgery complication. Studies indicate that a substantial percentage of patients experience some degree of dry eye symptoms following the procedure. This isn’t a universal experience, but it is a noteworthy consideration for surgical planning and patient expectations.
Timeline of Dry Eye Development
Dry eye symptoms can manifest at various points after cataract surgery. Initial symptoms might be subtle and appear within days of the procedure, while more pronounced symptoms may develop over weeks or even months. It’s important to recognize that the timeline can vary from patient to patient.
Mechanisms Behind Increased Dry Eye Risk
Several factors contribute to the increased risk of dry eye following cataract surgery. The surgical procedure itself can disrupt the delicate tear film mechanism. Additionally, medications used during or after surgery may also influence tear production and quality. Post-surgical inflammation can further exacerbate the problem. Finally, the use of intraocular lenses (IOLs) can also contribute.
Symptom Onset, Duration, and Severity
| Symptom Onset | Duration | Severity |
|---|---|---|
| Days to weeks post-surgery | Variable, from a few days to several months | Mild, moderate, or severe, depending on individual factors |
| Examples | Examples include initial discomfort to prolonged, severe irritation | Examples include slight discomfort to significant pain that interferes with daily activities |
The table above provides a general overview. Individual experiences can vary significantly. This information should not be considered medical advice, and consultation with an ophthalmologist is always recommended.
Symptoms and Diagnosis

Cataract surgery, while a life-changing procedure, can sometimes lead to a range of complications, one of which is dry eye. Understanding the symptoms and diagnostic processes is crucial for timely intervention and effective management. This section will delve into the specific symptoms associated with dry eye after cataract surgery, differentiating them from other causes of dry eye and outlining the diagnostic procedures ophthalmologists use.
Common Symptoms of Dry Eye Post-Surgery
Dry eye after cataract surgery presents a variety of symptoms, often subtle initially. These symptoms can range from mild discomfort to significant visual impairment, impacting the patient’s quality of life. Recognizing these symptoms is vital for prompt diagnosis and treatment.
- Visual Disturbances: Blurred vision, fluctuating vision, glare, and halos around lights are common. These can vary in severity and are often transient, but can also persist, necessitating further investigation.
- Discomfort: A persistent, gritty, or sandy feeling in the eye is frequently reported. This discomfort can range from mild irritation to severe pain, often exacerbated by activities such as reading or using a computer.
- Foreign Body Sensation: Patients may experience a sensation as if a foreign object is lodged in the eye, accompanied by a feeling of dryness or irritation. This sensation can be a significant source of discomfort and is often associated with reduced tear production.
- Other Symptoms: Other symptoms can include redness, itching, and excessive tearing. While tearing might seem counterintuitive in dry eye, it’s a body’s attempt to compensate for insufficient lubrication. This excessive tearing can lead to a further feeling of discomfort.
Differentiating Symptoms from Other Dry Eye Causes
Dry eye is a common condition, and its symptoms can overlap with those of other eye conditions. Understanding the specific characteristics of dry eye symptoms after cataract surgery is key to accurate diagnosis.
- Post-Surgical Dry Eye: Symptoms often present immediately or shortly after the surgery. The reduced tear production is directly related to the surgical procedure and the subsequent changes in the ocular surface.
- Non-Surgical Dry Eye: Symptoms associated with other causes, such as environmental factors (e.g., air conditioning, dry climate), systemic conditions (e.g., autoimmune diseases), or medication side effects, may manifest gradually over time. Symptoms in these cases are not necessarily linked to a specific event like cataract surgery.
Diagnostic Procedures for Post-Surgical Dry Eye
Accurate diagnosis of post-surgical dry eye involves a multi-faceted approach, combining subjective patient reports with objective measurements.
| Diagnostic Procedure | Description |
|---|---|
| Tear Film Evaluation | This involves assessing the quantity, quality, and stability of the tear film. Measurements include tear breakup time (TBUT), which indicates how quickly the tear film evaporates. This is a common and valuable diagnostic tool. |
| Ocular Surface Examinations | Detailed examination of the ocular surface using slit lamp microscopy and other advanced techniques can reveal signs of inflammation, damage, or dryness. Findings from this step aid in understanding the severity and type of dry eye. |
| Slit Lamp Biomicroscopy | A specialized microscope allows the ophthalmologist to examine the cornea and conjunctiva, revealing potential damage or inflammation. |
| Patient History | Thorough questioning about symptoms, medications, and any pre-existing conditions is crucial. A complete medical history helps identify potential contributing factors. |
Risk Factors and Contributing Factors
Post-cataract surgery dry eye is a complex issue, influenced by a multitude of factors. Understanding these factors is crucial for preventative measures and personalized management strategies. This section delves into the various risk factors and contributing elements, aiming to shed light on their relative significance in the development of dry eye after cataract surgery.While cataract surgery itself is a generally safe procedure, certain predispositions and circumstances can increase the likelihood of post-operative dry eye.
This heightened susceptibility stems from a combination of surgical techniques, patient characteristics, and underlying health conditions.
Surgical Techniques
Surgical factors play a significant role in the development of post-operative dry eye. Different surgical approaches and the use of certain instruments can potentially impact the tear film stability and overall ocular surface health. The incision size, the type of lens implanted, and the extent of manipulation of the ocular structures can all influence the risk of dry eye.
For instance, a larger incision or complex lens implantation might increase the likelihood of disrupting the tear film’s natural balance.
Patient Demographics
Patient-related characteristics also contribute to the development of dry eye after cataract surgery. Age, gender, and pre-existing conditions are all factors to consider. Age is often linked to a decrease in tear production, making older individuals more susceptible. Similarly, certain pre-existing medical conditions, such as autoimmune diseases, can exacerbate the risk of dry eye.
Pre-existing Conditions
Pre-existing conditions can significantly influence the development of dry eye post-cataract surgery. These conditions might affect tear production, tear film quality, or the overall health of the ocular surface. Conditions like Sjögren’s syndrome, rheumatoid arthritis, and certain autoimmune diseases are known to increase the risk of dry eye. Furthermore, pre-existing dry eye conditions, even if mild, can be exacerbated by the surgical procedure.
Relative Importance of Risk Factors
It is challenging to definitively quantify the relative importance of each risk factor. The impact of each factor is often interwoven and dependent on individual circumstances. For example, a patient with pre-existing dry eye and a history of autoimmune diseases will likely be at a higher risk compared to someone with no pre-existing conditions undergoing a standard cataract procedure.
Summary Table of Risk Factors
| Risk Factor | Potential Impact |
|---|---|
| Surgical Technique (e.g., incision size, lens implantation) | Disruption of tear film balance, potential for increased surface irritation. |
| Patient Age | Decreased tear production, increased susceptibility to dry eye. |
| Gender | Potential variations in tear production and composition. |
| Pre-existing Dry Eye | Exacerbation of existing condition. |
| Autoimmune Diseases (e.g., Sjögren’s syndrome) | Significant reduction in tear production and overall ocular surface health. |
| Medications | Potential for side effects impacting tear production. |
Management and Treatment Strategies
Managing dry eye after cataract surgery requires a multifaceted approach tailored to the individual’s specific needs and the severity of the condition. Early intervention and proactive management are crucial to alleviate discomfort and prevent potential complications. A combination of different treatments often proves most effective.Effective treatment strategies for dry eye after cataract surgery focus on restoring tear film stability and improving tear production.
This can involve addressing underlying causes, supplementing natural tear production, and promoting tear film health. Various treatment options are available, and choosing the right combination often requires consultation with an ophthalmologist.
Dealing with dry eyes after cataract surgery can be tricky. It’s a common side effect, but did you know that the body’s overall health, including proper digestion, can play a role? For example, understanding what digestive enzymes do can help you better manage post-surgery eye health. What are digestive enzymes are crucial for breaking down food, and a healthy digestive system could indirectly impact your body’s ability to produce moisture for your eyes.
So, while dry eyes are often treated with eye drops, maintaining a balanced digestive system might be another important step in recovery.
Artificial Tears
Artificial tears are a cornerstone of dry eye management. These over-the-counter eye drops provide a lubricating layer on the surface of the eye, mimicking the natural tear film. They come in various formulations, including preservative-free options for increased comfort, especially for long-term use. Frequent application throughout the day is often necessary to maintain a sufficient moisture level.
The immediate relief they offer makes them a valuable first-line treatment for mild to moderate dry eye.
Punctal Plugs
Punctal plugs are small, temporary or permanent devices inserted into the tear drainage channels (puncta). These plugs block the outflow of tears, increasing the amount of moisture on the eye’s surface. This leads to a longer-lasting moisturizing effect compared to artificial tears alone. Temporary plugs are often used initially to assess their effectiveness, while permanent plugs may be considered for more severe or chronic cases.
The procedure is relatively simple, but individual responses to plugs can vary.
Prescription Eye Drops
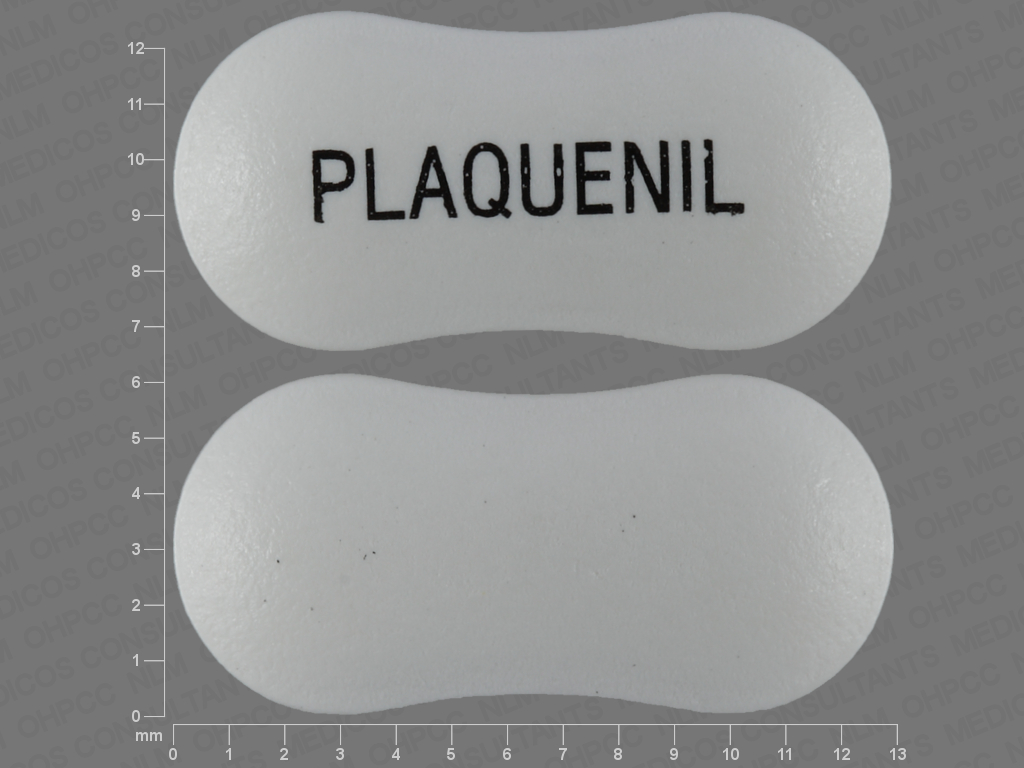
Prescription eye drops can be used to address specific underlying causes of dry eye or to augment the effects of artificial tears. These drops can include cyclosporine, lifitegrast, or other medications designed to improve tear production or reduce inflammation. While these drops often show positive results, they may have side effects such as mild stinging or burning, and careful monitoring by an ophthalmologist is essential.
The efficacy and potential side effects of each prescription medication differ.
Comparison of Treatment Options
| Type | Mechanism of Action | Potential Side Effects |
|---|---|---|
| Artificial Tears | Provide a lubricating layer on the eye surface, mimicking natural tears. | Minimal, some individuals may experience mild stinging or irritation. |
| Punctal Plugs | Block tear drainage, increasing tear retention on the eye surface. | Potential for discomfort during insertion, slight redness, or infrequent tearing. Temporary plugs are generally well-tolerated. |
| Prescription Eye Drops (e.g., Cyclosporine) | Reduce inflammation and promote tear production. | Potential for mild stinging, burning, or other minor discomfort; possible systemic effects (less common). |
Careful consideration of individual needs and responses is paramount in selecting the most suitable treatment plan for dry eye after cataract surgery. Consulting with an ophthalmologist is essential to determine the most effective and appropriate combination of therapies.
Prognosis and Long-Term Outcomes

Post-cataract surgery dry eye can vary significantly in its impact on patients. While many individuals experience temporary discomfort, some face more persistent issues. Understanding the potential long-term outcomes and factors influencing them is crucial for effective management and patient expectations.The prognosis for dry eye after cataract surgery depends on several factors, including the individual’s pre-existing eye health, the surgical technique employed, and the post-operative care followed.
Early detection and prompt intervention are essential in minimizing the risk of long-term complications.
Factors Influencing Long-Term Outcomes
Several factors contribute to the long-term outcomes of dry eye management. Individual responses to treatment, adherence to prescribed regimens, and proactive management of contributing factors play a vital role. For instance, patients who actively participate in eye drops and lifestyle adjustments are more likely to experience positive outcomes compared to those who do not. Consistent follow-up appointments with ophthalmologists are also key to monitoring the condition and adapting treatment plans as needed.
Potential Long-Term Outcomes
The long-term effects of dry eye after cataract surgery can range from mild discomfort to more severe conditions. Persistent dryness, accompanied by symptoms like burning, stinging, and foreign body sensation, can significantly impact quality of life. In some cases, dry eye can lead to corneal damage, such as superficial punctate keratitis, which may manifest as blurred vision or pain.
Vision Impairment
Vision impairment is a potential, though not inevitable, consequence of persistent dry eye. The severity of vision impairment is directly linked to the degree of corneal damage. In mild cases, vision changes might be subtle, causing slight blurring or reduced clarity. In more severe instances, vision impairment can be more pronounced, potentially leading to significant discomfort and difficulty with daily tasks.
For example, a patient with advanced corneal damage might experience difficulty driving or reading. The severity of vision impairment can vary based on individual factors and the response to treatment.
Dealing with dry eyes after cataract surgery can be a real pain, and understanding the medical procedures involved can be helpful. For instance, learning about CPT codes, which are used to report medical procedures like cataract surgery to insurance companies, can give you a better understanding of the billing process. Knowing what these codes mean can help you navigate the paperwork and ensure you’re getting the appropriate care for your dry eye symptoms after cataract surgery.
what are cpt codes It’s all part of the recovery journey.
Persistent Discomfort
Persistent discomfort is another possible long-term outcome. This can involve chronic burning, itching, or foreign body sensation. These symptoms can significantly affect a patient’s daily activities and overall well-being. For example, someone experiencing constant discomfort might find it difficult to concentrate at work or enjoy social activities. Such persistent discomfort highlights the importance of proactive management and close collaboration with an ophthalmologist to address the underlying causes and implement effective treatment strategies.
Severity and Duration of Dry Eye
The severity and duration of dry eye symptoms can significantly influence the long-term outcomes.
| Severity and Duration of Dry Eye | Potential Outcomes |
|---|---|
| Mild, short-term | Generally good prognosis; symptoms often resolve with appropriate treatment. |
| Moderate, short-term | Potential for some residual symptoms; close monitoring and management needed. |
| Mild, long-term | Potential for long-term discomfort, but vision impairment is less likely. |
| Moderate, long-term | Increased risk of vision impairment; requires aggressive management. |
| Severe, long-term | High risk of significant vision impairment and persistent discomfort; may necessitate specialized interventions. |
“Early intervention and consistent management of dry eye symptoms are crucial for achieving positive long-term outcomes and minimizing the risk of vision impairment.”
Prevention Strategies
Preventing dry eye after cataract surgery is crucial for a smooth recovery and optimal visual outcomes. Taking proactive steps both before and after the procedure can significantly reduce the risk of developing this common complication. By understanding the contributing factors and implementing preventative measures, patients can significantly improve their chances of a comfortable and successful post-operative experience.Implementing preventive strategies is key to minimizing the risk of post-operative dry eye.
This proactive approach involves careful consideration of pre-operative factors, diligent adherence to post-operative instructions, and a comprehensive understanding of the condition itself. By equipping themselves with knowledge and taking the necessary precautions, patients can significantly reduce the likelihood of dry eye and ensure a more comfortable recovery.
Pre-Operative Considerations
A thorough pre-operative evaluation plays a critical role in mitigating the risk of dry eye. This evaluation should include an assessment of the patient’s existing eye health, including any pre-existing dry eye conditions or contributing factors. Identifying and addressing these issues before surgery allows for targeted management and proactive strategies to minimize the risk of complications. For example, if a patient has a history of mild dry eye, the ophthalmologist can discuss potential pre-operative eye drops to prepare the eyes for the procedure.
Post-Operative Care, Dry eyes after cataract surgery
Adherence to post-operative instructions is essential for preventing dry eye. This includes consistent use of prescribed eye drops as directed by the ophthalmologist. Regular lubrication of the eyes helps maintain tear film stability, preventing dryness and promoting healing. The frequency and type of eye drops will depend on individual needs and the surgeon’s recommendations. Patients should follow their surgeon’s instructions meticulously, ensuring proper use of the prescribed medications to prevent dry eye and support recovery.
Dealing with dry eyes after cataract surgery can be a real pain. It’s a common side effect, but sometimes other health issues can contribute to the problem, like inflammatory bowel conditions. For example, understanding what indeterminate colitis is can be helpful in identifying potential underlying causes for persistent dry eyes. What is indeterminate colitis is a type of inflammatory bowel disease that can affect the digestive system.
Even though dry eyes seem unrelated, it’s worth considering these potential connections to get a more complete picture of your health. Fortunately, managing dry eyes post-surgery is usually straightforward with eye drops and other treatments.
Patient Education
Patient education is a cornerstone of successful dry eye prevention. Educating patients about the causes, symptoms, and management strategies of dry eye is crucial for proactive management and better outcomes. This education empowers patients to take an active role in their recovery and proactively address any emerging symptoms. For instance, a detailed explanation of the different types of eye drops, their purpose, and potential side effects, will aid the patient in making informed decisions and adhering to their treatment plan.
Preventive Measures
- Regular Eye Lubrication: Maintaining a healthy tear film is paramount. Regular use of artificial tears, as prescribed by the ophthalmologist, helps to replace lost tears and keep the eyes moist. This can include using lubricating eye drops before and after activities that may dry the eyes, such as prolonged computer use, or exposure to wind or air conditioning. This preventative step can significantly reduce the likelihood of dry eye.
- Maintaining Proper Hydration: Adequate hydration is essential for overall health, including eye health. Drinking sufficient amounts of water helps to maintain the proper balance of fluids in the body, which can indirectly affect tear production. Maintaining good hydration can be a simple, yet effective preventative measure.
- Avoiding Irritants: Exposure to environmental irritants, such as smoke, wind, or air conditioning, can exacerbate dry eye symptoms. Minimizing exposure to these irritants can be a crucial preventative step.
- Managing Underlying Conditions: Certain medical conditions, such as autoimmune diseases, can contribute to dry eye. Managing any underlying conditions effectively can help prevent or minimize dry eye symptoms. This involves consulting with primary care physicians and ophthalmologists for comprehensive care.
- Avoiding Overuse of Contact Lenses: Frequent or prolonged use of contact lenses can lead to dryness. If possible, patients should consider temporarily switching to glasses to reduce strain and potential dryness.
Illustrations and Visual Aids: Dry Eyes After Cataract Surgery
Understanding dry eye after cataract surgery requires visualizing the intricate interplay of eye anatomy, tear production, and surgical techniques. Visual aids help clarify the complex mechanisms involved and the impact of surgical interventions on the delicate tear film. This section will provide detailed illustrations and descriptions to aid in comprehension.
Eye Anatomy and Tear Production
The eye’s anatomy is crucial for understanding tear production and drainage. The tear film, a crucial component for eye health, is composed of three layers: an oily layer (lipid layer), an aqueous layer, and a mucous layer. The lacrimal gland produces the aqueous layer, providing lubrication and nutrients. Meibomian glands, located along the eyelids, produce the lipid layer, which prevents tear evaporation.
The conjunctiva, a thin membrane lining the eyelids and eye surface, secretes the mucous layer, promoting tear film stability. The tear drainage system, including the puncta, canaliculi, lacrimal sac, and nasolacrimal duct, removes excess tears. 
Tear Film Evaporation Mechanisms
Tear film evaporation is a natural process, but factors can accelerate it. The lipid layer plays a crucial role in preventing evaporation.
Defects or insufficient production of the lipid layer can lead to increased evaporation. Environmental conditions, such as dry air, wind, and low humidity, also contribute to tear film evaporation. Additionally, blinking frequency and eyelid movements influence tear film stability. Reduced blinking can exacerbate evaporation. 
Impact of Surgical Techniques on Tear Film
Cataract surgery, while improving vision, can sometimes impact the tear film.
Phacoemulsification, a common technique, may disrupt the meibomian glands, potentially affecting lipid layer production. Intraocular lens (IOL) placement and incision size can also influence tear film dynamics. Different types of IOLs may have varying effects on the tear film. 
Dry Eye Symptoms
Dry eye symptoms vary in severity and presentation. Common symptoms include a gritty or sandy feeling in the eyes, burning, stinging, and excessive tearing.
Other symptoms include blurry vision, especially in fluctuating light conditions, and discomfort when wearing contact lenses. The severity of symptoms can vary considerably among individuals. 
Final Wrap-Up
In conclusion, dry eyes after cataract surgery is a treatable condition. Understanding the risk factors, recognizing the symptoms, and implementing appropriate management strategies are key to achieving a successful recovery and maintaining good eye health.
Preventive measures and proactive communication with your ophthalmologist are vital in minimizing the risk and maximizing positive outcomes.