Papilledema symptoms causes diagnosis treatment – Papilledema symptoms, causes, diagnosis, and treatment are crucial for understanding this potentially serious condition. This comprehensive guide delves into the various visual and non-visual symptoms, exploring the underlying causes from intracranial pressure to tumors. We’ll examine diagnostic methods, from ophthalmoscopy to imaging, and discuss the diverse treatment approaches, from medication to surgery. Understanding the progression of visual field deficits and the complications of untreated papilledema is vital for proactive management.
We’ll analyze the nuances of symptoms, differentiating between early and advanced stages, and provide a detailed comparison of potential causes. The diagnostic process, including the critical role of ancillary tests, will be explored, with a clear explanation of the diagnostic criteria. The treatment section covers a wide spectrum of options, highlighting the importance of addressing the root cause for optimal results.
We’ll even look at illustrative case studies to solidify understanding and offer real-world insights.
Symptoms of Papilledema
Papilledema, a swelling of the optic disc, often signals an underlying neurological issue. Recognizing its symptoms is crucial for prompt diagnosis and treatment. Understanding these symptoms, from subtle visual changes to more pronounced systemic discomfort, allows for early intervention and better management of the condition.
Visual Symptoms
Visual symptoms are often the first indicators of papilledema, though they can vary significantly. Early changes may be subtle and easily overlooked, which highlights the importance of regular eye examinations. The pressure from the swelling on the optic nerve can cause a range of vision problems.
- Visual field deficits: These encompass a variety of potential losses in the field of vision. Patients might notice a reduced ability to see objects in specific parts of their visual field, potentially leading to tunnel vision or the inability to see peripheral objects. These deficits can range from slight impairments to significant loss of vision, depending on the severity of the swelling and its impact on the optic nerve.
- Blurred vision: Blurred vision, a common symptom, can be intermittent or persistent. It can affect both near and far vision and is often described as haziness or a loss of clarity. This symptom often accompanies other visual disturbances and can worsen over time as the condition progresses.
- Double vision (diplopia): While less common, double vision can occur. This phenomenon happens when the brain receives two images from the eyes, creating a sense of duplication. It may be a transient symptom or more persistent depending on the underlying cause and the progression of the papilledema.
Non-Visual Symptoms
Beyond the visual disturbances, papilledema often presents with other systemic symptoms. These symptoms can vary significantly and might be the first noticeable signs of the condition in some individuals.
- Headache: Headaches are a frequent companion to papilledema, often described as throbbing or persistent. The location of the headache may vary, and its intensity can range from mild to severe. The presence and characteristics of the headache can be helpful in assessing the severity of the condition.
- Nausea and vomiting: These gastrointestinal symptoms are frequently associated with increased intracranial pressure. The nausea and vomiting can be mild or severe and may occur in conjunction with headaches. These symptoms are typically indicative of a more advanced stage of the condition.
Symptom Progression
The severity and progression of papilledema symptoms are closely tied to the underlying cause and the rate at which the intracranial pressure increases. Early symptoms might be subtle and easily dismissed, but as the condition advances, symptoms become more pronounced.
| Symptom | Initial Symptoms | Advanced Symptoms |
|---|---|---|
| Visual Symptoms | Mild blurring, slight visual field changes | Significant visual field deficits, double vision, profound vision loss |
| Non-Visual Symptoms | Occasional mild headaches, infrequent nausea | Severe, persistent headaches, frequent nausea and vomiting, significant cognitive impairment |
Causes of Papilledema
Papilledema, the swelling of the optic disc, is a serious condition requiring prompt diagnosis and treatment. Understanding the underlying causes is crucial for effective management. Identifying the root cause helps direct appropriate therapies and prevent potential complications.The optic nerve, a vital pathway for transmitting visual information to the brain, can become inflamed due to a variety of factors.
These factors often involve increased intracranial pressure (ICP) or conditions that damage or obstruct the flow of cerebrospinal fluid (CSF). The resulting pressure buildup can lead to the swelling of the optic nerve head, characterized by papilledema. This swelling, while often a symptom, can also be a sign of a more serious underlying health problem.
Intracranial Pressure Elevation
Increased intracranial pressure (ICP) is a leading cause of papilledema. This pressure increase can arise from various conditions, all affecting the delicate balance within the skull. The pathophysiology involves the compression of the optic nerve, causing swelling and edema in the optic disc. This compression restricts blood flow and impairs the function of the optic nerve.Several factors contribute to elevated ICP.
Hydrocephalus, a condition characterized by excessive cerebrospinal fluid (CSF) in the brain’s ventricles, is a prime example. The increased fluid volume puts pressure on the brain and surrounding structures. Similarly, brain tumors can exert pressure on the surrounding tissues, leading to increased ICP and subsequent papilledema. Head trauma, though less frequent, can also cause a rise in ICP.
The resulting swelling and bleeding within the brain and surrounding tissues can impede the normal flow of CSF and cause intracranial pressure to increase.
Tumors and Masses
Brain tumors and other intracranial masses, such as cysts or abscesses, exert direct pressure on the optic nerve. This pressure interferes with blood flow and nutrient delivery to the nerve, leading to inflammation and swelling of the optic disc. The location of the mass relative to the optic nerve significantly influences the severity of papilledema.The frequency of papilledema stemming from tumors varies based on the type of tumor and its growth rate.
Benign tumors tend to cause a slower increase in ICP, whereas malignant tumors can exhibit rapid growth, potentially leading to a more acute presentation of papilledema. This difference in growth rates can affect the diagnostic timeline and management strategies.
Infections and Inflammatory Conditions
Infections within the brain or meninges (the membranes surrounding the brain and spinal cord) can trigger inflammation and swelling, leading to increased ICP and papilledema. Meningitis, an infection of the meninges, is a prime example. The inflammatory response caused by the infection can exert pressure on the optic nerve, leading to its swelling. Similarly, encephalitis, an inflammation of the brain, can lead to similar consequences.The prevalence of papilledema associated with infections depends on the specific infectious agent and the overall health of the individual.
Viral infections are more common than bacterial ones, and the severity of the infection significantly impacts the likelihood of papilledema development. Early diagnosis and prompt treatment are crucial to prevent further complications.
Other Potential Causes
Certain other medical conditions can also contribute to papilledema, although less frequently than the causes mentioned above. These include:
- Aneurysms: Weakened areas in the blood vessels in the brain can bulge, causing pressure on the optic nerve. This pressure buildup can cause papilledema.
- Venous sinus thrombosis: Blood clots in the venous sinuses of the brain can obstruct blood flow, leading to increased intracranial pressure and papilledema.
- Trauma: Head injuries can cause swelling and bleeding within the brain, increasing ICP and potentially causing papilledema.
- Medications: Certain medications, including steroids and some antibiotics, can increase ICP as a side effect, leading to papilledema in susceptible individuals.
Table of Potential Causes of Papilledema
| Underlying Medical Condition | Specific Cause |
|---|---|
| Increased Intracranial Pressure | Hydrocephalus, Brain Tumors, Head Trauma |
| Tumors and Masses | Brain Tumors, Cysts, Abscesses |
| Infections | Meningitis, Encephalitis |
| Other Conditions | Aneurysms, Venous Sinus Thrombosis, Trauma, Medications |
Diagnosis of Papilledema
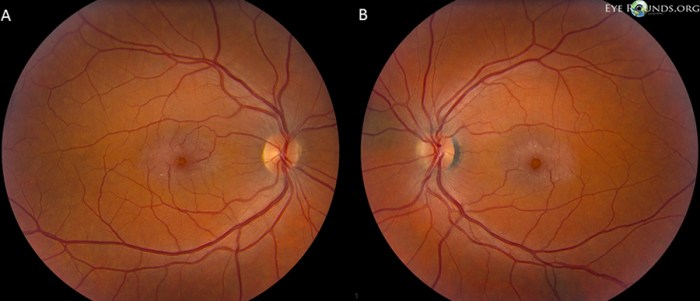
Diagnosing papilledema involves a meticulous approach combining ophthalmological examination with neurological and ancillary imaging studies. Accurate identification is crucial for timely intervention and management of the underlying cause. The process begins with a comprehensive evaluation, focusing on the optic disc and visual function.Ophthalmologists employ various diagnostic methods to identify the presence and severity of papilledema. These methods are designed to detect the characteristic swelling of the optic nerve head, and often necessitate a thorough understanding of the patient’s medical history and presenting symptoms.
Ophthalmoscopy
Ophthalmoscopy is a fundamental diagnostic tool for evaluating the optic nerve. It allows visualization of the optic disc, enabling detection of characteristic changes associated with papilledema. A thorough ophthalmoscopic examination is essential for confirming the diagnosis.A step-by-step procedure for performing an ophthalmoscopic examination to detect papilledema typically involves the following:
- Patient positioning: The patient is positioned comfortably, usually seated, with appropriate lighting and the necessary instruments.
- Pupil dilation: Pupil dilation may be necessary to obtain a clear view of the optic disc.
- Slit lamp examination: The ophthalmoscope is used to carefully examine the optic nerve head, focusing on the optic disc for signs of swelling, blurring of margins, and other indicative features.
- Documentation: Detailed documentation of the findings, including the degree of swelling, the presence of hemorrhages or exudates, and the appearance of the optic disc, is crucial for diagnosis and monitoring.
Visual Field Testing
Visual field testing is an essential adjunct to ophthalmoscopy. It assesses the extent of visual loss associated with papilledema. This is vital to understand the impact of the optic nerve swelling on the patient’s vision. Changes in visual field are often a significant indicator of the severity of the condition. Testing assesses the patient’s ability to perceive light or objects in different parts of their visual field.
Ancillary Tests
While ophthalmoscopy and visual field testing are crucial, ancillary tests such as CT scans and MRIs play a significant role in evaluating the underlying cause of papilledema. These imaging modalities provide detailed information about the brain and its structures, aiding in identifying possible lesions or conditions that might be responsible for the optic nerve swelling. These tests can also help exclude other neurological conditions with similar symptoms.
- CT Scan: A computed tomography (CT) scan is often used to evaluate for acute intracranial events such as hemorrhages or structural abnormalities.
- MRI: Magnetic resonance imaging (MRI) provides detailed visualization of the brain and its structures, allowing for identification of masses, lesions, and other abnormalities that might be responsible for the papilledema.
Diagnostic Criteria and Procedures
The following table summarizes the diagnostic criteria and procedures used to confirm papilledema. It is crucial to remember that this table provides a general overview and the exact criteria may vary depending on the clinical setting and the individual patient’s presentation.
| Diagnostic Criterion | Procedure |
|---|---|
| Swollen optic disc | Ophthalmoscopic examination |
| Blurred disc margins | Ophthalmoscopic examination |
| Visual field defects | Visual field testing |
| Elevated intracranial pressure | Clinical assessment, potential lumbar puncture |
| Underlying cause identified | Neurological examination, imaging studies (CT/MRI) |
Treatment of Papilledema
Papilledema, characterized by swelling of the optic disc, necessitates prompt and effective treatment. The cornerstone of management is identifying and addressing the underlying cause. The severity of papilledema and its impact on vision dictate the urgency and intensity of treatment. Failure to address the root cause can lead to irreversible vision loss.Effective treatment strategies for papilledema focus on reducing intracranial pressure (ICP), managing the underlying medical condition, and preventing further complications.
This involves a multi-faceted approach combining medical interventions, such as medications, and surgical procedures when necessary. The choice of treatment is tailored to the specific cause of the papilledema.
Understanding papilledema symptoms, causes, diagnosis, and treatment is crucial. Often, underlying conditions like increased intracranial pressure are the culprits. A related, though different, respiratory condition is bronchiectasis, which is thoroughly covered in this excellent guide: complete guide to bronchiectasis. Ultimately, recognizing the signs of papilledema is vital for timely intervention and effective management.
Treatment Approaches Based on Underlying Cause
Treatment for papilledema hinges on identifying and addressing the root cause. A thorough evaluation, including medical history, neurological examination, and diagnostic imaging, is crucial to pinpoint the etiology. Common underlying causes include intracranial masses, hydrocephalus, infections, and inflammatory conditions. Once the cause is established, appropriate treatment strategies can be initiated.
Medications for Managing Papilledema
Various medications are used to manage papilledema, primarily focusing on reducing intracranial pressure. Diuretics, such as acetazolamide and furosemide, are frequently prescribed to promote fluid excretion. Corticosteroids, such as dexamethasone, may be employed to reduce inflammation, particularly in cases of inflammatory conditions contributing to increased ICP. The dosage and duration of these medications are tailored to the individual patient’s response and the underlying condition.
Surgical Interventions for Papilledema
Surgical interventions are reserved for cases where medical management proves insufficient or when the underlying cause necessitates direct intervention. Surgical procedures for papilledema aim to alleviate pressure on the optic nerve and surrounding structures. Examples include craniotomy for the removal of tumors or shunting procedures for hydrocephalus. Specific surgical techniques are determined by the nature and location of the causative lesion.
Summary of Treatment Options
| Underlying Cause | Treatment Options |
|---|---|
| Intracranial masses (e.g., tumors) | Surgical resection of the mass, radiation therapy, chemotherapy (depending on the tumor type) |
| Hydrocephalus | Shunting procedures (e.g., ventriculoperitoneal shunt) |
| Infections (e.g., meningitis) | Antimicrobial therapy, supportive care |
| Inflammatory conditions (e.g., idiopathic intracranial hypertension) | Medications (diuretics, corticosteroids), weight loss (if obesity is a factor), optic nerve sheath fenestration (a surgical procedure) |
| Trauma | Management of the underlying trauma, medications to reduce ICP |
Visual Field Deficits in Papilledema
Papilledema, the swelling of the optic nerve head, can significantly impact vision. A key aspect of this impact is the development of visual field deficits. These deficits represent a loss of the visual field’s ability to perceive light, and understanding their progression is critical for timely diagnosis and effective management. The nature and extent of these deficits vary, depending on the severity and location of the underlying cause.Visual field deficits in papilledema typically manifest as a gradual loss of peripheral vision.
The initial stages often go unnoticed, as the loss is subtle. As the condition progresses, the deficits become more pronounced, potentially affecting central vision as well. These changes in vision can have profound effects on daily activities and require careful monitoring and management.
Types of Visual Field Deficits
Visual field deficits in papilledema can encompass various patterns, reflecting the pressure and compression exerted on the optic nerve. These include:
- Peripheral Visual Field Loss: This is the most common initial finding. Patients may report difficulty seeing objects in their peripheral vision, such as things on the side of their field of view. This loss can be subtle at first, but it gradually progresses as the papilledema worsens. Examples include difficulty spotting a car approaching from the side while driving or difficulty recognizing someone approaching from the periphery while walking.
- Bitemporal Hemianopia: In some cases, the pressure on the optic nerve can lead to a loss of vision in the outer portions of both visual fields. This is referred to as bitemporal hemianopia, and it may progress to involve more of the visual field if the condition isn’t managed.
- Central Scotoma: A central scotoma is a dark spot or blind area in the center of the visual field. While less common in the early stages of papilledema, a central scotoma can occur as the condition progresses and the optic nerve is severely affected. This can cause difficulties in reading, recognizing faces, or performing tasks that require precise visual acuity.
Understanding papilledema symptoms, causes, diagnosis, and treatment is crucial. The swelling of the optic nerve, often a symptom of underlying conditions, can be a serious concern. Fortunately, advancements in surgical techniques, like those detailed in the history of surgery timeline , have significantly improved our ability to treat this condition. Further research and refined procedures continue to improve outcomes for those affected by papilledema.
- Homonymous Hemianopia: This type of visual field deficit involves the loss of the same half of the visual field in both eyes. It’s less frequently associated with early-stage papilledema but can be a sign of more severe optic nerve involvement and possible compression. This can significantly impact daily tasks such as driving or navigating environments.
Progression of Visual Field Deficits
The progression of visual field deficits in papilledema is closely correlated with the underlying cause and the severity of the condition. In the early stages, the loss is often subtle and may only be noticeable during specific tasks or in low-light conditions. As papilledema worsens, the visual field loss extends, progressing from the periphery towards the center.
Optic Nerve Compression and Visual Field
The diagram would show the optic nerve, the retinal fibers, and the visual field. It would illustrate how compression of the optic nerve at various points leads to specific visual field defects. The affected retinal fibers and the resulting visual field loss would be highlighted in the diagram.
Implications of Visual Field Deficits on Daily Life
Visual field deficits significantly impact daily activities. Examples of how these deficits might affect a patient include:
- Driving: Difficulty seeing cars or pedestrians approaching from the sides, leading to increased risk of accidents.
- Walking: Difficulty navigating or detecting obstacles in the periphery, increasing the risk of falls or collisions.
- Reading: A central scotoma can impair reading comprehension and increase the effort required for reading tasks.
- Social Interactions: Difficulties recognizing faces or understanding social cues due to peripheral vision loss can impact social interactions.
- Work and Employment: Certain professions requiring visual acuity and peripheral vision may be impacted by the deficits, leading to work-related challenges or job changes.
Complications of Untreated Papilledema: Papilledema Symptoms Causes Diagnosis Treatment

Papilledema, the swelling of the optic nerve at the back of the eye, is a serious condition that requires prompt medical attention. Untreated papilledema can lead to a cascade of complications, most significantly impacting vision and overall health. Understanding these potential consequences is crucial for proactive management and ensuring the best possible outcome.Untreated papilledema allows increased intracranial pressure to persist, damaging the delicate optic nerve.
Understanding papilledema symptoms, causes, diagnosis, and treatment is crucial for early intervention. High intracranial pressure often leads to this condition, causing vision changes and headaches. Fortunately, a knowledgeable nurse practitioner like rachael zimlich rn bsn can provide expert guidance throughout the diagnostic and treatment process. This involves a thorough evaluation of symptoms and medical history, ultimately leading to the best possible outcome for patients.
This damage can progress rapidly, leading to irreversible vision loss and other severe consequences. The longer the condition remains untreated, the higher the risk of permanent damage and the more significant the impact on quality of life.
Potential Vision Loss
The optic nerve is vulnerable to pressure and inflammation caused by elevated intracranial pressure. Progressive damage to the nerve fibers can result in visual field deficits, starting with peripheral vision loss and potentially progressing to central vision loss. In severe cases, complete blindness can occur. This loss of vision can significantly impair a patient’s ability to perform daily tasks, impacting their independence and quality of life.
For instance, a patient might struggle with driving, reading, or recognizing faces.
Long-Term Effects on Vision
The long-term effects of untreated papilledema on vision are often irreversible. The damage to the optic nerve can lead to permanent visual field defects, blurring, or even complete blindness. These deficits can dramatically alter a patient’s ability to navigate their environment and participate in activities they once enjoyed. For example, a person who loved hiking might find it difficult to navigate trails or recognize landmarks.
Long-Term Effects on Overall Health
Untreated papilledema is not just a visual concern; it can have significant implications for overall health. Persistent high intracranial pressure can put strain on other brain structures, leading to headaches, nausea, and vomiting. In some cases, the pressure can affect other parts of the nervous system, leading to cognitive difficulties or other neurological problems. The underlying cause of the papilledema, such as a brain tumor or bleeding, also needs to be addressed.
The consequences of untreated underlying conditions can be catastrophic.
Sudden Vision Loss: Immediate Action
Sudden vision loss is a medical emergency, particularly if it is associated with papilledema. If you experience sudden vision loss, immediately seek emergency medical attention. Time is crucial in these situations, as prompt treatment can potentially prevent further damage. Early intervention can significantly improve the chances of preserving vision and mitigating long-term complications.
Steps to Take When Experiencing Sudden Vision Loss, Papilledema symptoms causes diagnosis treatment
If you experience sudden vision loss, follow these steps:
- Immediately call emergency services: Prompt medical attention is essential to determine the cause of the vision loss and initiate appropriate treatment.
- Describe the symptoms: Clearly communicate the nature and extent of the vision loss to the emergency responders.
- Follow the instructions of medical professionals: Comply with the instructions provided by the emergency medical services and hospital personnel.
Illustrative Case Studies
Papilledema, a swelling of the optic nerve at the back of the eye, can manifest in various ways, making accurate diagnosis and timely intervention crucial. Understanding how the condition presents itself in different individuals through case studies provides valuable insights into its complexities. These case studies illustrate the spectrum of symptoms, causes, and treatment approaches associated with papilledema.These case studies highlight the importance of recognizing the subtle signs of papilledema, which often mimic other conditions.
Early diagnosis is essential to prevent potential complications, and these examples demonstrate how early intervention can positively impact patient outcomes.
Case Study 1: A Young Adult with Gradual Onset
A 25-year-old female presented with progressively worsening headaches, along with blurry vision and intermittent double vision. She reported a recent history of a viral infection. On examination, the ophthalmologist noted bilateral papilledema, with elevation of the optic disc. Further investigations revealed a cerebrospinal fluid (CSF) pressure elevation, consistent with a diagnosis of idiopathic intracranial hypertension (IIH). Treatment focused on reducing CSF pressure through medication (diuretics) and lifestyle modifications (weight management).
The patient’s symptoms gradually subsided with appropriate management, and visual acuity returned to normal. This case emphasizes the importance of considering IIH in patients with papilledema, particularly in those with a history of weight gain or a recent viral infection.
Case Study 2: A Child with a Rapidly Progressive Course
A 10-year-old boy presented with severe headaches, vomiting, and visual disturbances. The symptoms developed acutely over a few days, accompanied by a noticeable decrease in his level of consciousness. The ophthalmologist found significant papilledema, and a CT scan revealed a brain tumor compressing the brain stem. This case illustrates the importance of prompt diagnosis and treatment in cases of rapidly progressive papilledema, particularly when accompanied by neurological symptoms like altered mental status.
The rapid progression of the symptoms and the life-threatening nature of the underlying cause underscored the urgency of the situation. Aggressive treatment, including surgical intervention to remove the tumor, was necessary to alleviate the pressure and save the child’s life. The case highlights the crucial role of imaging in evaluating the cause of papilledema and the importance of a multidisciplinary approach in managing such complex cases.
Case Study 3: A Patient with a History of Hypertension
A 60-year-old male with a history of hypertension presented with persistent headaches and blurred vision. He had been experiencing increasing difficulty with concentration and coordination. The ophthalmologist noted bilateral papilledema and visual field deficits. Investigations revealed uncontrolled hypertension, which had been contributing to increased intracranial pressure. Treatment focused on aggressively controlling blood pressure and managing the elevated intracranial pressure.
This case emphasizes the potential for secondary causes of papilledema, such as hypertension, and the critical need for thorough evaluation to identify the underlying cause. The patient’s improvement was directly related to stabilizing his blood pressure and addressing the underlying condition.
Closure

In conclusion, papilledema is a complex condition requiring a thorough understanding of its multifaceted aspects. By grasping the symptoms, causes, diagnosis, and treatment, we equip ourselves with the knowledge to recognize and address this potentially vision-threatening issue. This comprehensive guide provides a valuable resource for healthcare professionals and individuals seeking to understand papilledema better. Early intervention and appropriate management are paramount to mitigating long-term complications and improving patient outcomes.