What are coxsackievirus infections? They’re a group of viruses that can cause a range of illnesses, from mild to severe. Understanding these viruses, their different types, how they spread, and the symptoms they cause is key to effective prevention and treatment. This exploration delves into the various aspects of coxsackievirus infections, from their global distribution and prevalence to their impact on public health.
We’ll examine the pathogenesis, clinical manifestations, diagnostic methods, available treatments, and potential complications. Prepare to learn more about these often-overlooked infections!
Coxsackieviruses, a family of enteroviruses, are common culprits behind various ailments. They’re transmitted through close contact and contaminated food or water. Different types can cause a diverse spectrum of symptoms, from the familiar hand, foot, and mouth disease to more serious conditions. Understanding the variations within these viruses is critical for accurate diagnosis and appropriate management.
Introduction to Coxsackievirus Infections

Coxsackieviruses are a group of enteroviruses, meaning they primarily infect the gastrointestinal tract. These viruses are responsible for a wide range of illnesses, ranging from mild, self-limiting infections to more severe conditions. Understanding the different types, transmission routes, and symptoms is crucial for appropriate diagnosis and management.Coxsackieviruses are categorized into two groups: Coxsackie A viruses and Coxsackie B viruses.
These groups are further subdivided into various serotypes, each with its own potential clinical presentation. This complex classification reflects the diversity of the viruses and the range of illnesses they can cause.
Routes of Transmission
Coxsackieviruses are typically spread through the fecal-oral route. This means the virus can be transmitted when contaminated fecal matter comes into contact with the mouth, either directly or indirectly through contaminated surfaces or objects. Respiratory droplets can also play a role in transmission, especially in cases of upper respiratory tract infections. Close contact with infected individuals, such as through shared utensils or personal items, can facilitate the spread.
Types of Coxsackieviruses
The classification of Coxsackieviruses is crucial for understanding their different clinical presentations. A and B groups are distinguished based on their growth characteristics in different cell cultures, as well as the type of illnesses they typically cause. Coxsackie A viruses are more often associated with hand, foot, and mouth disease, herpangina, and other mild illnesses. Coxsackie B viruses, on the other hand, can cause more severe conditions, including myocarditis (inflammation of the heart muscle) and meningitis (inflammation of the membranes surrounding the brain and spinal cord).
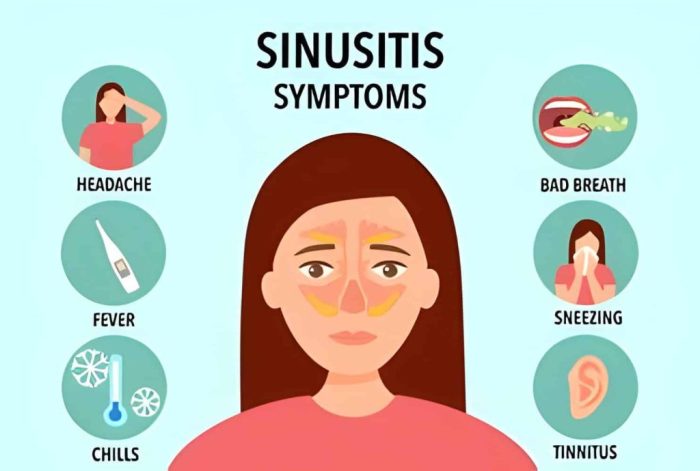
Symptoms of Coxsackievirus Infections
The symptoms of Coxsackievirus infections vary depending on the specific type of virus and the individual’s immune response. Common symptoms include fever, headache, sore throat, and malaise. Some infections, like hand, foot, and mouth disease, are characterized by a distinctive skin rash.
Comparison of Clinical Presentations
| Virus Type | Primary Symptoms | Secondary Symptoms |
|---|---|---|
| Coxsackie A viruses (e.g., types 1-16) | Sore throat, fever, small blisters in the mouth (herpangina), skin rash on hands, feet, and buttocks (hand, foot, and mouth disease) | Occasionally, headache, malaise, vomiting, diarrhea |
| Coxsackie B viruses (e.g., types 1-6) | Fever, malaise, muscle aches, abdominal pain, headache, nausea, and vomiting | Potential for myocarditis (inflammation of the heart muscle), meningitis (inflammation of the membranes surrounding the brain and spinal cord), encephalitis (inflammation of the brain), hepatitis (inflammation of the liver) |
Epidemiology and Prevalence
Coxsackievirus infections, a common cause of mild to severe illnesses, exhibit a global distribution and varying prevalence across different populations. Understanding their epidemiology is crucial for effective prevention and management strategies. This section delves into the geographic spread, infection frequency in various demographics, associated risk factors, and seasonal patterns of these infections.The prevalence of Coxsackievirus infections is influenced by a complex interplay of factors including socioeconomic conditions, hygiene practices, and access to healthcare.
Variations in infection rates across different regions are often tied to these factors, impacting the overall burden of the disease.
Global Distribution
Coxsackieviruses are globally distributed, with infections reported in all continents. Geographic variations in prevalence exist, but a consistent pattern of occurrence is seen. Factors such as population density, sanitation, and access to healthcare play a significant role in shaping these regional differences.
Frequency of Infections in Different Populations
Infants and young children are particularly susceptible to Coxsackievirus infections, experiencing a higher frequency of infections compared to older age groups. This susceptibility is often linked to a less developed immune system and increased exposure to potential viral sources. While all age groups can be affected, the severity of illness tends to be milder in older individuals due to the development of immunity.
Risk Factors
Several risk factors can increase the likelihood of contracting a Coxsackievirus infection. Crowded living conditions and poor sanitation facilitate the spread of the virus, especially in areas with limited access to clean water and hygiene facilities. Close contact with infected individuals, such as in families or childcare settings, can also significantly increase the risk. Pre-existing medical conditions can also influence the severity of infection, particularly in immunocompromised individuals.
Seasonal Variations
Some studies suggest seasonal variations in Coxsackievirus infection rates, although this isn’t a universal phenomenon. Data from different regions show that infection rates may fluctuate depending on factors such as temperature and humidity, which can impact the transmission dynamics of the virus. Further research is needed to fully elucidate these seasonal patterns and understand their underlying mechanisms.
Epidemiological Data Summary
| Region | Infection Rate (estimated) | Risk Factors |
|---|---|---|
| North America | Moderate | Crowded living conditions, lower hygiene standards, limited access to healthcare, contact with infected individuals |
| Sub-Saharan Africa | High | Poor sanitation, lack of access to clean water, malnutrition, limited healthcare resources, overcrowding |
| Southeast Asia | High | Crowded living conditions, lower hygiene standards, poor sanitation, limited access to healthcare, high population density |
| Europe | Moderate | Crowded living conditions, lower hygiene standards, contact with infected individuals, and in some cases, seasonal fluctuations |
| South America | Moderate to High | Crowded living conditions, lower hygiene standards, limited access to healthcare, contact with infected individuals |
Pathogenesis and Mechanisms

Coxsackieviruses, a diverse group of enteroviruses, employ various strategies to establish infection and cause a range of diseases. Understanding their pathogenesis is crucial for developing effective prevention and treatment strategies. This section delves into the mechanisms of Coxsackievirus infection, including viral replication within the host, the immune response, and comparative pathogenesis across different types.
Viral Entry and Replication
Coxsackieviruses gain entry into host cells primarily through receptor-mediated endocytosis. Specific cellular receptors, often involved in nutrient uptake, mediate this process. Once inside the cell, the viral capsid is uncoated, releasing the viral RNA. This RNA then directs the cellular machinery to synthesize viral proteins and replicate the viral genome. This process involves several key steps.
Steps in Viral Replication
- Attachment: The virus binds to specific receptors on the host cell surface. Examples of these receptors include integrins and other cell surface proteins.
- Entry: The virus enters the cell via receptor-mediated endocytosis, forming an endosome. The endosome acidifies, facilitating viral uncoating.
- Uncoating: The viral capsid is degraded, releasing the viral RNA into the cytoplasm.
- Transcription: Viral RNA is transcribed into messenger RNA (mRNA) by the host cell’s machinery. This mRNA directs the synthesis of viral proteins.
- Translation: Viral proteins are translated from the mRNA, with some proteins being structural components of new virions and others playing regulatory roles.
- Replication: The viral RNA genome is replicated using viral enzymes. This process often involves the formation of a replication complex within the cell.
- Assembly: Newly synthesized viral RNA and proteins assemble to form new virions.
- Release: Newly assembled virions are released from the host cell, often causing cell lysis, which can lead to tissue damage and inflammation.
Immune Response to Coxsackievirus Infection
The host mounts a multifaceted immune response to combat Coxsackievirus infection. The innate immune system, including interferons and natural killer cells, plays an initial role in recognizing and combating viral infection. Subsequently, the adaptive immune system, involving B and T cells, further contributes to clearing the infection. Antibody production helps neutralize the virus, while cytotoxic T lymphocytes (CTLs) eliminate infected cells.
Comparison of Coxsackievirus Types
While all Coxsackieviruses share basic mechanisms of infection, variations exist in their tropism and pathogenic potential. Some types preferentially infect specific tissues or organs, contributing to the diversity of clinical presentations. For example, Coxsackievirus B3 is associated with myocarditis, while Coxsackievirus A16 is commonly linked to hand, foot, and mouth disease. The differences in the specific receptors utilized and the immune responses triggered by various types can lead to distinct clinical outcomes.
Detailed studies on the specific molecular mechanisms behind these differences are ongoing.
Clinical Manifestations and Diagnosis
Coxsackievirus infections manifest in a wide array of clinical presentations, ranging from mild, self-limiting illnesses to severe, potentially life-threatening conditions. Accurate diagnosis is crucial for appropriate management and to prevent complications. Identifying the specific Coxsackievirus type involved can be helpful in predicting the course of the infection and guiding treatment strategies.Understanding the diverse clinical presentations and available diagnostic methods is essential for healthcare professionals to effectively manage these infections.
A thorough evaluation of symptoms, coupled with appropriate laboratory tests, allows for accurate diagnosis and timely intervention.
Clinical Presentations
Coxsackievirus infections exhibit a spectrum of symptoms, reflecting the diverse tropism of the virus. Common presentations include:
- Hand, Foot, and Mouth Disease (HFMD): This is a common presentation, especially in young children. Characterized by blisters and sores on the hands, feet, and mouth, along with fever and general malaise. This presentation is frequently associated with Coxsackievirus A16.
- Herpangina: This condition is characterized by fever, sore throat, and painful blisters or ulcers in the back of the throat. It is typically caused by Coxsackievirus A viruses, and can be a significant source of discomfort for the affected individuals.
- Meningitis and Encephalitis: Coxsackieviruses can cause inflammation of the membranes surrounding the brain (meningitis) and the brain itself (encephalitis). These infections can present with symptoms such as fever, headache, stiff neck, and altered mental status. This serious complication can affect people of all ages.
- Myocarditis and Pericarditis: Coxsackieviruses can lead to inflammation of the heart muscle (myocarditis) and the lining of the heart (pericarditis). This can present with chest pain, palpitations, and shortness of breath. This severe presentation can result in potentially life-threatening complications if left untreated.
- Other presentations: Some individuals may experience a nonspecific febrile illness, with symptoms like fever, headache, and muscle aches. These nonspecific presentations are not easily identifiable with the naked eye, requiring laboratory tests for accurate diagnosis.
Diagnostic Methods
Accurate identification of Coxsackievirus infections relies on a combination of clinical evaluation and laboratory testing. Clinical presentation, along with epidemiological context, helps to narrow down potential diagnoses.
- Clinical Evaluation: The physician assesses the patient’s symptoms, medical history, and physical examination findings to determine the possible cause. Factors like age, recent exposure to others with similar symptoms, and specific symptoms like blisters on the hands, feet, or mouth are crucial clues.
- Laboratory Testing: Laboratory tests are essential for confirming the diagnosis. These tests typically include virus isolation, serological testing, and molecular methods.
Laboratory Tests in Diagnosis
Laboratory testing plays a vital role in confirming the diagnosis of Coxsackievirus infections.
Coxsackievirus infections are pretty common, often causing mild illnesses like a sore throat or a rash. Sometimes, though, these infections can lead to more serious liver issues. Understanding how autoimmune hepatitis is diagnosed is key to getting a proper diagnosis, and knowing the symptoms of coxsackievirus infections can help determine if other underlying issues are present. Fortunately, many cases resolve on their own, but seeking medical attention if symptoms persist is crucial.
Knowing how to differentiate between different causes of liver problems, including the role of coxsackievirus infections, is important. how autoimmune hepatitis is diagnosed is a great resource for understanding the diagnostic process. In summary, coxsackievirus infections can sometimes have overlapping symptoms with other conditions, making a precise diagnosis essential.
- Virus Isolation: This method involves culturing the virus from a clinical specimen (e.g., throat swab, stool sample, or cerebrospinal fluid). While this is a definitive method, it requires specialized laboratory facilities and time for results. The process of culturing a virus involves a series of steps, beginning with collecting a sample and ending with observing the virus under a microscope.
The time taken to complete these steps can range from several days to a few weeks.
- Serological Testing: These tests detect antibodies produced by the body in response to the virus. This method can be helpful in determining if the patient has been previously exposed to the virus. The serological tests help in identifying past infections, which is crucial for understanding the individual’s immune response.
- Molecular Methods (PCR): Polymerase chain reaction (PCR) is a sensitive and specific technique that can detect the genetic material of the virus in clinical specimens. This method is often preferred due to its speed and efficiency, and provides quicker turnaround times.
Examples of Symptoms and Viral Types
The following table provides examples of common symptoms and their associated Coxsackievirus types:
| Diagnostic Method | Procedure | Accuracy |
|---|---|---|
| Virus Isolation | Culturing the virus from a clinical sample | High, but time-consuming |
| Serological Testing | Detecting antibodies against the virus | Useful for past infections |
| Molecular Methods (PCR) | Detecting viral genetic material | High sensitivity and specificity |
Treatment and Prevention
Coxsackievirus infections, while often resolving on their own, can cause significant discomfort and, in rare cases, lead to more serious complications. Understanding the available treatment options and preventive measures is crucial for managing these infections effectively. This section will explore supportive care, available treatments, and strategies for preventing the spread of these viruses.Effective management of coxsackievirus infections primarily focuses on alleviating symptoms and supporting the body’s natural defenses.
Different approaches may be necessary depending on the specific manifestation of the infection.
Supportive Care Strategies
Effective management of coxsackievirus infections often involves a multifaceted approach focusing on alleviating symptoms and supporting the body’s natural defenses. This frequently includes providing symptomatic relief and ensuring adequate hydration to combat dehydration, which can be a concern, particularly in young children.
- Rest and Hydration: Encouraging rest and ensuring adequate hydration are paramount. Fluids help prevent dehydration, a common concern, especially in young children. This is particularly important in cases of fever and vomiting.
- Pain and Fever Management: Over-the-counter pain relievers, like acetaminophen (paracetamol) or ibuprofen, can effectively reduce fever and muscle aches. However, aspirin should be avoided in children and adolescents due to the risk of Reye’s syndrome. Always consult a healthcare professional before administering any medication, especially to children.
- Wound Care: For skin manifestations like hand, foot, and mouth disease, gentle cleaning and protecting the affected areas from further irritation are crucial. Avoid harsh soaps or scrubbing to prevent discomfort.
Treatment Options
Currently, there’s no specific antiviral medication available to treat coxsackievirus infections. Management primarily involves supportive care to alleviate symptoms and allow the body to fight off the infection.
- No Specific Antivirals: There are no antiviral medications specifically targeting coxsackieviruses. This highlights the importance of supportive care in managing the infection.
Preventive Measures
Preventing coxsackievirus infections relies heavily on general hygiene practices to limit transmission. These practices are crucial in reducing the spread of the virus.
- Hand Hygiene: Regular and thorough handwashing with soap and water, especially after using the restroom, changing diapers, or touching potentially contaminated surfaces, is essential.
- Hygiene Practices: Maintaining good hygiene practices, such as disinfecting frequently touched surfaces and cleaning shared items, can help prevent the spread of coxsackievirus.
- Avoid Close Contact: Minimizing close contact with infected individuals, especially during periods of illness, is a crucial preventative step.
- Proper Sanitation: Ensuring proper sanitation and waste disposal can help prevent the spread of the virus.
Comparison of Treatment Approaches
Given the absence of specific antiviral drugs, the comparison of treatment approaches primarily revolves around the effectiveness of different supportive care strategies in alleviating symptoms and improving patient outcomes. Strategies focus on managing discomfort and ensuring the body can fight off the infection.
Complications and Long-Term Effects
Coxsackievirus infections, while often mild, can sometimes lead to significant complications and long-term health issues. Understanding these potential consequences is crucial for appropriate monitoring and management. Prompt diagnosis and treatment can significantly reduce the risk of severe outcomes.A variety of complications can arise depending on the specific Coxsackievirus type and the individual’s immune response. Some complications manifest immediately, while others may develop over time, highlighting the importance of ongoing medical attention and follow-up care.
Coxsackievirus infections, often causing mild illnesses like the common cold, can sometimes lead to more serious issues. While managing respiratory symptoms is crucial, understanding the various inhalers like Flovent, Qvar, Pulmicort, Alvesco, or Asmanex is important for those with chronic conditions. These medications, which are frequently prescribed for asthma and other respiratory issues, can be a vital part of treatment plans, as detailed in this helpful guide on flovent qvar pulmicort alvesco or asmanex.
Ultimately, recognizing and addressing coxsackievirus infections promptly is key to preventing complications.
Potential Neurological Complications
Coxsackieviruses, particularly Coxsackievirus B, can potentially cause myocarditis (inflammation of the heart muscle) and meningoencephalitis (inflammation of the brain and spinal cord membranes). These conditions can lead to lasting neurological impairments. The severity of neurological complications varies greatly, ranging from mild symptoms to severe, debilitating conditions. In some cases, permanent neurological damage can occur. For example, some individuals might experience long-term cognitive deficits or motor impairments.
The severity and nature of these complications depend heavily on the individual’s overall health and the specific type of Coxsackievirus involved.
Long-Term Cardiovascular Issues
Myocarditis, inflammation of the heart muscle, is a serious potential complication of some Coxsackievirus infections. This inflammation can lead to various cardiovascular problems, including heart failure and arrhythmias. In some instances, the damage to the heart muscle can be permanent, impacting the heart’s ability to pump blood efficiently. This can lead to long-term cardiovascular issues, potentially requiring ongoing medical management and potentially impacting life expectancy.
One example is a young athlete who developed myocarditis following a Coxsackievirus infection, leading to reduced athletic performance and the need for regular cardiac monitoring.
Other Potential Long-Term Health Effects
Certain Coxsackievirus infections can have lasting effects on various organ systems. The following is a list of potential long-term health effects:
- Neurological damage: This can manifest in various ways, from mild cognitive impairments to more severe conditions like paralysis or epilepsy.
- Cardiovascular issues: Inflammation of the heart muscle (myocarditis) can lead to heart failure, arrhythmias, and other long-term cardiac problems.
- Chronic fatigue syndrome: Some individuals may experience persistent fatigue and other symptoms long after the initial infection has subsided.
- Chronic pain conditions: Certain Coxsackievirus infections have been linked to the development of chronic pain conditions, affecting various parts of the body.
- Developmental delays in children: In some cases, Coxsackievirus infections during childhood can lead to developmental delays in cognitive or motor skills.
- Liver dysfunction: The liver can be affected in some cases, leading to long-term liver problems.
- Kidney problems: In rare instances, kidney dysfunction can be a consequence of a Coxsackievirus infection.
Importance of Monitoring for Complications
Early detection and treatment of potential complications are essential. Regular medical check-ups, especially for individuals with a history of Coxsackievirus infection, are crucial. Monitoring for signs and symptoms of complications, such as persistent fatigue, chest pain, or neurological symptoms, is critical. This proactive approach can lead to early intervention and potentially mitigate long-term health issues. This is particularly important for individuals who have a weakened immune system or pre-existing medical conditions.
Coxsackievirus infections are pretty common, often causing mild symptoms like a fever or sore throat. While they’re usually not serious, understanding the nuances of different kinds of brain injuries, like the difference between concussions and traumatic brain injuries, here , is important. Ultimately, recognizing the symptoms of coxsackievirus infections is key for proper diagnosis and treatment, and hopefully, a quick recovery.
Case Studies and Examples
Coxsackievirus infections, while often mild, can manifest in a wide range of ways. Understanding the diverse clinical presentations, diagnostic processes, and treatment outcomes is crucial for appropriate patient care. Real-world case studies provide valuable insights into the spectrum of these infections and inform best practices.
Diverse Clinical Presentations
Coxsackievirus infections can present with a variety of symptoms, ranging from mild to severe. These infections can affect different organs and systems, leading to varying clinical manifestations. Some patients experience mild, self-limiting symptoms, while others develop more severe conditions requiring intensive medical intervention. Understanding the diversity in clinical presentation is vital for accurate diagnosis and appropriate treatment strategies.
Diagnostic Process in Specific Cases
Accurate diagnosis of Coxsackievirus infections relies on a combination of clinical evaluation, laboratory tests, and sometimes, imaging studies. The diagnostic process often involves considering the patient’s medical history, physical examination findings, and the results of specific tests. The choice of diagnostic tests will vary depending on the suspected site of infection and the clinical presentation. For example, in cases of suspected myocarditis, cardiac enzyme tests and electrocardiography (ECG) may be crucial components of the diagnostic workup.
Successful Treatment Outcomes
The treatment for Coxsackievirus infections is primarily supportive, focusing on managing symptoms and preventing complications. Recovery often involves rest, hydration, and over-the-counter pain relievers. In cases of more severe infections, such as myocarditis, specific therapies like antiviral medications or immunomodulators may be employed. The successful outcomes in many cases demonstrate the effectiveness of supportive care and the importance of prompt diagnosis and management.
Case Study Examples
| Case Study ID | Patient Profile | Symptoms | Diagnosis |
|---|---|---|---|
| CS1 | 10-year-old male, previously healthy | Fever, sore throat, headache, muscle aches, rash | Coxsackievirus A infection (hand, foot, and mouth disease) |
| CS2 | 25-year-old female, with a history of asthma | Sudden onset of chest pain, shortness of breath, fatigue | Coxsackievirus B infection (myocarditis) |
| CS3 | 60-year-old male, with hypertension | Severe abdominal pain, nausea, vomiting | Coxsackievirus infection (acute hemorrhagic conjunctivitis) |
| CS4 | Infant, 3 months old | Fever, irritability, lethargy, decreased appetite, and stiff neck | Coxsackievirus infection (aseptic meningitis) |
These are just a few examples, and the presentation of Coxsackievirus infections can vary significantly. The specific symptoms and the organs affected will influence the diagnostic approach and the course of treatment. Monitoring for potential complications is essential in managing patients with Coxsackievirus infections.
Public Health Implications: What Are Coxsackievirus Infections
Coxsackievirus infections, while often mild, can pose significant public health challenges, especially during outbreaks. Understanding the impact on different populations and implementing appropriate control measures is crucial for minimizing the spread and severity of these infections. The potential for complications and long-term effects further underscores the need for proactive public health strategies.
Impact on Public Health, What are coxsackievirus infections
Coxsackievirus infections can significantly impact public health through various avenues. High rates of infection, especially in vulnerable populations, can strain healthcare resources. The potential for severe complications like myocarditis and meningitis can lead to increased hospitalizations and long-term disabilities. Moreover, the economic burden of lost productivity due to illness and treatment adds to the public health concern.
Importance of Public Health Measures
Effective public health measures are essential to control outbreaks of coxsackievirus infections. These measures aim to reduce transmission, protect vulnerable populations, and limit the overall impact on public health. Strategies like improved sanitation, promoting hand hygiene, and isolation of infected individuals can effectively break the chain of transmission.
Role of Public Health Professionals
Public health professionals play a vital role in managing coxsackievirus outbreaks. Their expertise in epidemiology allows for accurate assessment of outbreaks, identification of high-risk populations, and development of targeted interventions. Public health professionals also work to educate the public about prevention strategies, ensuring that individuals take the necessary precautions to protect themselves and others.
Surveillance Systems
Effective surveillance systems are critical for monitoring coxsackievirus infections and identifying outbreaks early. These systems collect data on the incidence, prevalence, and characteristics of infections, enabling public health officials to track trends, identify emerging patterns, and implement timely interventions. This real-time data is invaluable for adjusting public health strategies and ensuring optimal control of the outbreaks.
Examples of Public Health Campaigns
Public health campaigns play a vital role in educating the community about coxsackievirus infections. These campaigns often emphasize the importance of hand hygiene, promoting vaccination where available, and providing information on recognizing symptoms. Examples could include public service announcements on television, radio, and social media, community workshops, and educational materials distributed in schools and healthcare facilities. The specific focus and content of these campaigns will be tailored to the local context and risk factors.
Concluding Remarks
In conclusion, coxsackievirus infections are a complex group of viral illnesses with varied clinical presentations. From their diverse types and transmission routes to the wide range of symptoms and potential complications, these viruses demand careful consideration. Public health measures and effective treatments are essential for managing these infections and minimizing their impact. This comprehensive overview provides a starting point for understanding coxsackievirus infections and highlights the importance of vigilance in preventing and treating these illnesses.