Sore throat and cough – a common ailment affecting people of all ages. This comprehensive guide delves into the intricacies of these symptoms, exploring everything from their various characteristics to potential causes and effective treatment options. We’ll examine how symptoms differ between adults and children, uncover common triggers, and compare them to similar conditions like allergies and the flu.
Understanding the nuances of sore throats and coughs is crucial for effective self-care and prompt medical intervention when necessary. This article aims to equip you with the knowledge to navigate these often-disruptive symptoms with confidence.
Understanding the Symptoms
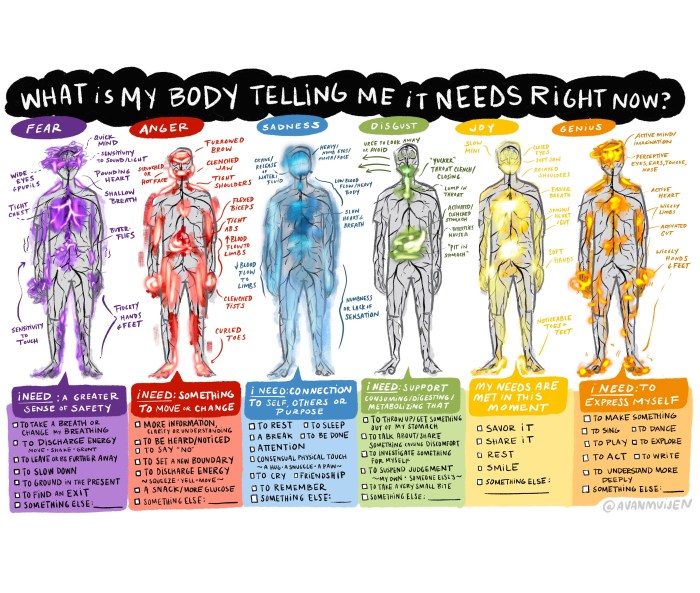
Sore throats and coughs are common ailments that can significantly impact daily life. Understanding the various characteristics, potential causes, and differences in symptoms between adults and children is crucial for effective self-care and seeking appropriate medical attention. This section delves into the specifics of these symptoms, allowing you to better recognize and manage them.Sore throats can manifest in several ways, from a mild scratchiness to a sharp, burning pain.
The discomfort can vary in intensity and location, sometimes radiating to the ears or jaw. The feeling can be described as a constant irritation or a throbbing sensation, exacerbated by swallowing or talking.
Sore Throat Characteristics
Sore throats often accompany a range of sensations, including scratchiness, pain, and a burning feeling. The severity of these symptoms can fluctuate, and they can be localized to a specific area of the throat or more widespread. Factors such as the specific infection or irritation involved influence the exact characteristics experienced.
Cough Types and Causes
Coughs vary significantly in their presentation and cause. A dry cough, often characterized by a persistent, hacking sound, may not produce phlegm. Conversely, a productive cough produces mucus, which can vary in color and consistency. Barking coughs, often associated with croup in children, produce a distinctive, harsh sound.
Differences in Symptoms Between Adults and Children
The presentation of symptoms can differ between adults and children. Children may exhibit a higher fever, irritability, and difficulty swallowing compared to adults. The symptoms of coughs and sore throats can also manifest differently, impacting the overall well-being and daily activities of the child.
Triggers and Associated Illnesses
Sore throats and coughs can be triggered by various factors, including environmental irritants, such as dry air or smoke, and infections. Common illnesses associated with these symptoms include the common cold, influenza (flu), and strep throat. Other triggers can include allergies, exposure to pollutants, or even certain foods.
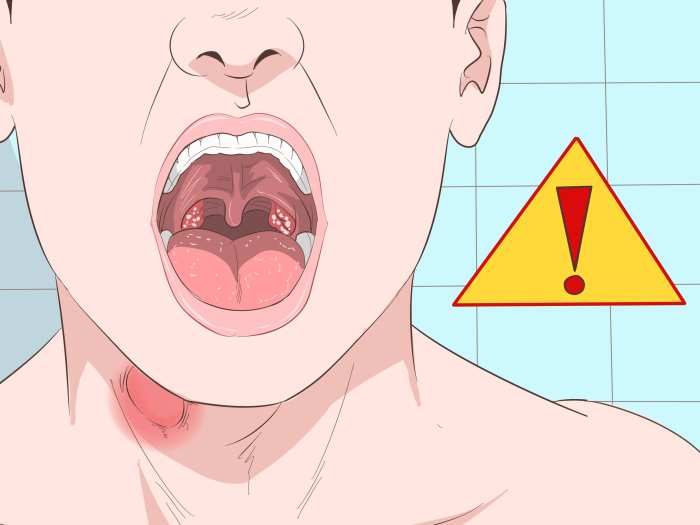
Ugh, a sore throat and cough are never fun. Sometimes, those pesky symptoms can be a sign of something more serious, like an abscess. Understanding abscess causes and treatment is crucial if you’re experiencing persistent discomfort. Fortunately, there are effective ways to manage the condition, and a proper diagnosis is key. abscess causes and treatment can help you understand the various factors involved.
No matter what the cause, it’s essential to seek medical attention for a sore throat and cough that doesn’t improve quickly.
Comparison with Similar Conditions
Sore throats and coughs can overlap with symptoms of other conditions, such as allergies or the flu. Distinguishing between these conditions can be challenging, but observing other symptoms, such as sneezing, runny nose, or body aches, can help in differentiating them. For instance, allergic reactions typically present with nasal congestion and itchy eyes alongside the cough and sore throat, while the flu often involves fever, body aches, and fatigue.
A persistent sore throat and cough can sometimes be a symptom of various things, including a simple cold or flu. However, it’s crucial to consider more serious possibilities, like the potential connection to lymph node positive breast cancer. While less common, these symptoms can sometimes indicate a more significant underlying health issue. Even if you’re not experiencing other breast cancer symptoms, it’s best to consult a doctor if your sore throat and cough persist for an extended period.
Table: Sore Throats and Coughs
| Symptom Type | Possible Causes | Treatment |
|---|---|---|
| Dry Cough | Viral infections, irritants (e.g., smoke, dry air), postnasal drip | Rest, hydration, humidifiers, cough suppressants (consult a doctor) |
| Productive Cough | Bacterial infections, bronchitis, pneumonia | Rest, hydration, expectorants (consult a doctor) |
| Sore Throat (mild) | Viral infections, dry air, allergies | Rest, fluids, throat lozenges |
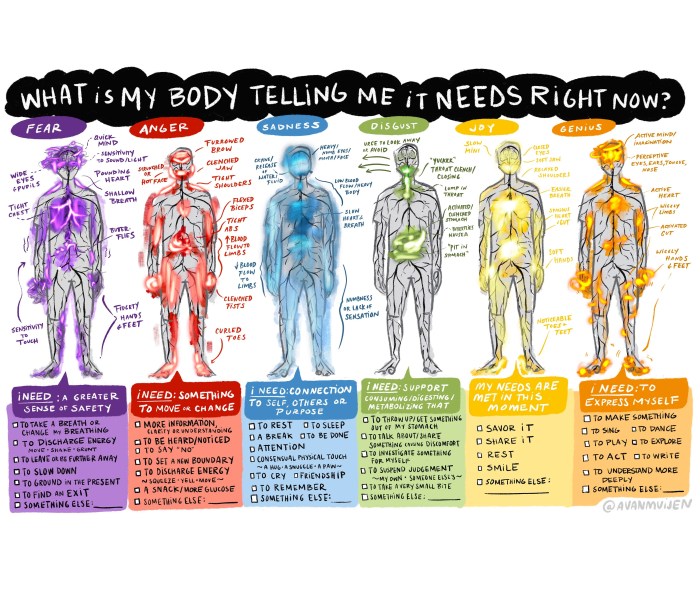
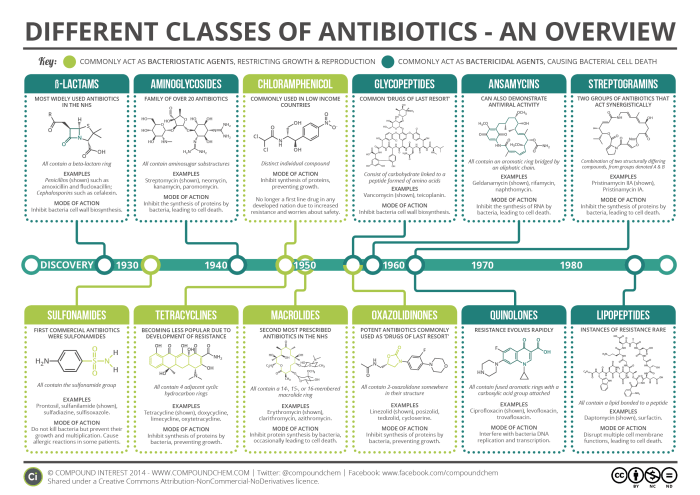
| Sore Throat (severe) | Strep throat, tonsillitis, other bacterial infections | Antibiotics (prescribed by a doctor) |
Potential Causes

Sore throats and coughs are common ailments, often signaling an underlying issue. Understanding the potential causes can help you determine the best course of action and when professional medical advice is necessary. This section delves into the various factors contributing to these symptoms, from viral infections to environmental irritants and lifestyle choices.Viral infections are a frequent culprit behind sore throats and coughs.
Bacterial infections, while less common, can also lead to these symptoms. Other factors, such as environmental irritants and allergies, can also contribute to discomfort. Finally, lifestyle choices can influence the likelihood of developing these conditions. A thorough understanding of these causes is key to effective self-care and prompt medical intervention when appropriate.
Viral Infections
Viral infections are a leading cause of sore throats and coughs, often associated with the common cold and influenza. These infections are spread through respiratory droplets and can affect individuals of all ages. The body’s immune response to these infections often manifests as a sore throat, cough, and other symptoms.
- Common Cold: Viruses like rhinoviruses, coronaviruses, and others are responsible for the common cold. Symptoms typically include a runny nose, sneezing, and a mild cough, alongside a scratchy or sore throat. The duration of a common cold is usually around 7-10 days, though some symptoms may linger for a few weeks.
- Influenza (Flu): Influenza viruses cause the flu. Characterized by a sudden onset of symptoms, including fever, body aches, a severe cough, and a sore throat. Flu symptoms tend to be more severe and debilitating than a common cold, often lasting 1-2 weeks. Severe cases can lead to complications requiring medical attention.
- Other Respiratory Viruses: Various other viruses can cause respiratory illnesses, leading to sore throats and coughs. Examples include parainfluenza virus, RSV (respiratory syncytial virus), and adenoviruses. Symptoms and duration can vary depending on the specific virus.
Bacterial Infections
Bacterial infections, while less frequent than viral infections, can also result in sore throats and coughs. Bacterial infections are often associated with more severe symptoms and a greater risk of complications. Prompt medical attention is crucial when suspecting a bacterial infection.
Ugh, a sore throat and cough are seriously bumming me out lately. I’ve been trying various remedies, but nothing seems to be working perfectly. I even looked into using Questran Cholestyramine bile acid resin, which is sometimes used to help with other digestive issues. Questran cholestyramine bile acid resin is apparently a pretty common treatment for those kinds of issues, but it seems a bit of a stretch for a sore throat and cough.
Hopefully, something will finally work soon to get me back on my feet!
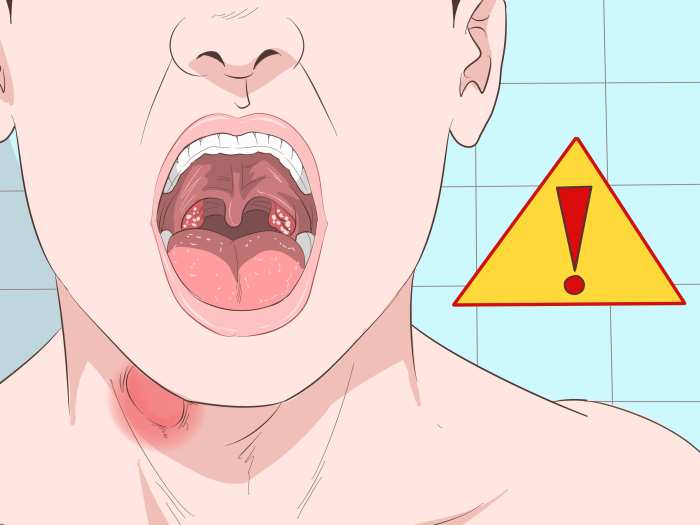
- Strep Throat (Streptococcal Pharyngitis): Streptococcal bacteria cause strep throat. This infection is characterized by a sudden onset of a sore throat, often accompanied by fever, headache, and body aches. The throat may appear red and inflamed. Prompt treatment is essential to prevent potential complications.
- Whooping Cough (Pertussis): Pertussis bacteria cause whooping cough, a highly contagious respiratory illness. Early symptoms can resemble a common cold, but later stages are characterized by severe coughing fits, often followed by a whooping sound. Vaccination is crucial for prevention.
- Other Bacterial Infections: Other bacteria, such as Haemophilus influenzae, can also cause respiratory infections with sore throats and coughs. These infections can vary in severity.
Other Potential Causes
Environmental irritants and allergies can trigger sore throats and coughs. Exposure to pollutants, smoke, or dry air can irritate the respiratory system, leading to these symptoms. Allergies to pollen, dust mites, or other substances can also cause inflammation and irritation. Lifestyle factors, such as smoking, excessive alcohol consumption, and poor sleep hygiene, can also increase the risk of developing these conditions.
- Environmental Irritants: Exposure to smoke, dust, pollutants, or dry air can irritate the throat and airways, causing a sore throat and cough. The severity of symptoms depends on the duration and intensity of exposure.
- Allergies: Seasonal allergies or allergies to indoor triggers can lead to a sore throat, cough, and runny nose. Symptoms can be similar to a cold or the flu.
- Lifestyle Factors: Smoking, excessive alcohol consumption, and poor sleep hygiene can weaken the immune system and increase susceptibility to respiratory illnesses. These factors can also irritate the throat and airways, leading to coughs and sore throats.
Potential Causes Table, Sore throat and cough
| Potential Cause | Symptoms | Typical Duration |
|---|---|---|
| Common Cold | Runny nose, sneezing, mild cough, sore throat | 7-10 days |
| Influenza (Flu) | Fever, body aches, severe cough, sore throat | 1-2 weeks |
| Strep Throat | Sudden sore throat, fever, headache, body aches | 7-10 days with treatment |
| Whooping Cough | Initial cold-like symptoms, progressing to severe coughing fits | 1-6 weeks |
| Environmental Irritants | Sore throat, cough, dry throat | Variable, depending on exposure |
| Allergies | Sore throat, runny nose, cough, itchy eyes | Variable, depending on allergen exposure |
Distinguishing Viral and Bacterial Infections
Distinguishing between viral and bacterial infections is crucial for appropriate treatment. Viral infections typically resolve on their own within a few weeks, while bacterial infections may require antibiotics. A healthcare professional can help determine the cause and recommend the most effective treatment plan.
Common Cold vs. Flu
Differentiating between a common cold and the flu can be challenging based on symptoms alone. The flu generally presents with more severe symptoms, including fever, body aches, and a more pronounced cough. The duration of flu symptoms is also typically longer than a common cold. Consulting a healthcare professional can confirm the diagnosis and guide appropriate treatment.
Diagnosis and Assessment
Navigating a sore throat and cough can be unsettling. Understanding the diagnostic process empowers you to seek appropriate care and manage your symptoms effectively. This section details the steps involved in determining the cause of your discomfort and how healthcare professionals assess the severity of your condition.
Diagnostic Steps for Sore Throat and Cough
A thorough evaluation involves a systematic approach to pinpoint the underlying cause. This process is crucial for determining the best course of treatment.
| Step | Description |
|---|---|
| Patient History | Gathering information about the patient’s medical history, including previous illnesses, allergies, medications, and lifestyle factors. |
| Physical Examination | A physical assessment of the throat, including observation for redness, swelling, or discharge, and listening to the lungs for signs of infection. |
| Symptom Evaluation | Detailed questioning about the duration, severity, and characteristics of the sore throat and cough. |
| Diagnostic Tests | Ordering tests like rapid strep tests, cultures, or imaging studies to confirm or rule out specific diagnoses. |
| Differential Diagnosis | Considering various potential causes of the symptoms based on the collected information and tests. |
| Treatment Plan | Developing a personalized treatment plan based on the confirmed diagnosis. |
Questions for Assessing Severity and Duration
Healthcare professionals use specific questioning techniques to gain a comprehensive understanding of the patient’s condition. These questions help gauge the severity and duration of symptoms, crucial for determining the appropriate course of action. Examples include:
- When did the symptoms begin? This helps establish the timeline and potential triggers.
- How severe is the pain on a scale of 1 to 10? This quantifies the discomfort and helps prioritize treatment.
- Are there any accompanying symptoms, such as fever, body aches, or difficulty swallowing? These additional symptoms can provide clues about the potential cause.
- Have you had similar episodes in the past? Recurring patterns can indicate chronic conditions or specific triggers.
- What have you done to alleviate the symptoms? Self-care measures provide insight into the patient’s approach to managing the problem.
Diagnostic Tests
Various tests may be conducted to confirm or rule out specific diagnoses. The choice of test depends on the suspected cause.
- Rapid Strep Test: A quick test that detects the presence of Streptococcus bacteria, a common cause of strep throat. A positive result suggests the need for antibiotics.
- Throat Cultures: A more definitive method for identifying bacterial or viral infections. A swab of the throat is sent to a laboratory for analysis.
- Blood Tests: These may be conducted to assess for specific infections or underlying conditions, such as mononucleosis.
- Imaging Tests (e.g., X-rays): These tests are used to evaluate the lungs and other areas for signs of infection or complications, particularly when the cough is persistent or severe.
Importance of Medical History
A thorough medical history is essential in the diagnostic process. Past illnesses, allergies, and current medications provide context for understanding the current symptoms.
- Previous Infections: Knowing if the patient has had similar infections in the past can help determine if the current episode is a recurrence.
- Allergies: Allergies to certain medications or substances can influence the choice of treatment.
- Medications: Understanding any medications the patient is currently taking is crucial for avoiding drug interactions and determining the most appropriate course of action.
Determining Severity
The severity of a sore throat and cough is assessed based on the intensity of symptoms, duration, and presence of other complications.
- Mild Symptoms: A sore throat with a mild cough, lasting a few days, may be managed with over-the-counter remedies.
- Moderate Symptoms: More intense pain, a persistent cough, and accompanying symptoms like fever may warrant a visit to a healthcare professional.
- Severe Symptoms: High fever, difficulty swallowing, or breathing difficulties require immediate medical attention.
Self-Assessment Flowchart
This flowchart guides individuals through a self-assessment process for sore throat and cough.[Flowchart Image Description: A simple flowchart would visually guide a user through questions regarding the duration, severity, and presence of other symptoms. Branches would lead to recommendations for self-care, over-the-counter medication, or seeking professional medical attention based on the answers to these questions. The flowchart would be designed with clear decision points and arrows connecting them, culminating in appropriate action.]
Treatment and Management: Sore Throat And Cough

Dealing with a sore throat and cough can be uncomfortable and disruptive. Fortunately, many effective remedies can help alleviate symptoms and promote recovery. This section details common treatments, emphasizing the importance of self-care and when to seek professional medical attention.Effective management of sore throats and coughs involves a multifaceted approach, combining over-the-counter medications, lifestyle adjustments, and potentially, home remedies.
A crucial aspect is understanding when to seek medical intervention, as some cases may require specific treatments or further evaluation.
Over-the-Counter Medications
Common over-the-counter medications offer relief from sore throat and cough symptoms. Analgesics like ibuprofen or acetaminophen can help reduce pain and fever. Lozenges or sprays containing local anesthetics can numb the throat, providing temporary relief from discomfort. Cough suppressants can help manage persistent coughing, while expectorants can aid in clearing mucus. Always follow the recommended dosage instructions on the product label.
Rest, Hydration, and Nutrition
Rest is paramount in allowing your body to fight off infection. Adequate hydration is equally crucial for maintaining overall health and promoting the thinning and removal of mucus. Drinking plenty of fluids, such as water, herbal tea, or clear broths, is essential. A balanced diet rich in fruits, vegetables, and protein supports your immune system’s function.
Home Remedies
Several home remedies can offer soothing relief for sore throats and coughs. Warm salt water gargles can help soothe a sore throat by reducing inflammation. Honey, a natural cough suppressant, can be consumed directly or added to warm drinks. Steam inhalation, using hot water and essential oils (like eucalyptus), can help loosen congestion and soothe respiratory irritation.
However, be mindful of potential allergies or sensitivities to certain ingredients.
Home Care Measures
Implementing certain home care measures can significantly contribute to symptom management. Maintaining a humid environment through a humidifier can help soothe dry throats and coughs. Avoiding irritants like smoke or strong odors can further reduce discomfort. Keeping your environment clean and well-ventilated can help prevent further spread of infections. Elevating your head while sleeping can help reduce nighttime coughing.
When to Seek Medical Attention
While many sore throats and coughs resolve with home remedies, certain situations warrant medical intervention. Persistent or severe pain, high fever, difficulty swallowing or breathing, or a persistent cough that lasts longer than a week should prompt a consultation with a healthcare professional. Also, if you have underlying health conditions, or are pregnant or breastfeeding, it’s always prudent to seek advice from a doctor before starting any treatment.
Treatment Options Table
| Treatment Option | Effectiveness | Potential Side Effects |
|---|---|---|
| Over-the-counter pain relievers (e.g., ibuprofen, acetaminophen) | Generally effective in reducing pain and fever | May cause stomach upset, allergic reactions in some individuals |
| Throat lozenges/sprays | Provide temporary numbing and soothing | May cause mild local irritation |
| Cough suppressants | Can reduce coughing frequency | May cause drowsiness, or other side effects depending on the medicine |
| Expectorants | Aid in mucus removal | May cause nausea or vomiting in some individuals |
| Warm salt water gargles | Soothes sore throat | Generally safe |
| Honey | Natural cough suppressant | Not recommended for infants |
| Steam inhalation | Can help loosen congestion | May cause discomfort if the steam is too hot |
Preventative Measures
“Maintaining good hygiene practices, such as frequent handwashing, avoiding close contact with sick individuals, and getting enough rest, significantly reduces the risk of developing sore throats and coughs.”
Prevention
Sore throats and coughs, while often frustrating, are frequently preventable. Understanding the factors contributing to their development allows us to implement proactive measures to minimize the risk of infection and discomfort. By focusing on hand hygiene, vaccinations, immune system health, environmental controls, and preventative measures against spreading infection, we can significantly reduce the likelihood of experiencing these ailments.Effective prevention relies on a multi-faceted approach, incorporating both personal habits and environmental considerations.
This section delves into strategies for mitigating risk and promoting overall respiratory health.
Importance of Hand Hygiene
Proper handwashing is a cornerstone of infection prevention. Washing hands frequently and thoroughly with soap and water, especially after coughing, sneezing, or touching shared surfaces, significantly reduces the transmission of viruses and bacteria. Germs can easily spread through direct contact, highlighting the crucial role of hand hygiene in preventing the spread of respiratory infections.
Role of Vaccinations
Vaccinations play a critical role in preventing certain infections that lead to sore throats and coughs. Specific vaccines may target influenza viruses, which are a common cause of these symptoms. Receiving recommended vaccinations can dramatically lower the risk of contracting these infections, thereby mitigating the need for treatment and recovery time. The benefits of vaccination extend beyond individual protection; they contribute to community immunity, safeguarding those who cannot be vaccinated.
Strategies for Maintaining a Healthy Immune System
A robust immune system is the body’s first line of defense against infections. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients to support immune function. Adequate sleep, stress management techniques, and regular exercise further contribute to a strong immune response. Prioritizing these lifestyle factors strengthens the body’s natural defenses, making it less susceptible to infections that cause sore throats and coughs.
Avoiding Environmental Irritants
Environmental factors can trigger or exacerbate sore throats and coughs. Exposure to smoke, pollutants, and allergens can irritate the respiratory tract, increasing the risk of infection. Minimizing exposure to these irritants by staying indoors during periods of high pollution, using air purifiers, and avoiding known allergens can reduce discomfort and the likelihood of developing these conditions.
Preventative Measures Against Spreading Infection
Coughing and sneezing etiquette is essential in preventing the spread of infections. Covering the mouth and nose with a tissue or the elbow when coughing or sneezing helps contain the spread of respiratory droplets. Proper disposal of used tissues and frequent handwashing are vital to minimizing the risk of contagion. Individuals with infections should consider isolating themselves to reduce the risk of transmission.
Improving Air Quality for Respiratory Health
Maintaining good air quality is vital for respiratory health. Indoor air quality can be significantly improved by using air purifiers that filter out dust, pollen, and other irritants. Ensuring adequate ventilation by opening windows regularly can also help reduce the concentration of pollutants. These measures can contribute to a healthier environment, reducing the likelihood of respiratory issues, such as sore throats and coughs.
Final Wrap-Up
In conclusion, recognizing the symptoms, potential causes, and appropriate treatment strategies for sore throat and cough is vital for managing these conditions effectively. By understanding the differences between viral and bacterial infections, and when to seek medical attention, you can navigate these common ailments with greater ease and potentially prevent further complications. Remember, proactive self-assessment and appropriate medical guidance are key to a swift recovery.