Moderna covid 19 vaccine – The Moderna COVID-19 vaccine, a crucial tool in the global fight against the pandemic, offers a compelling story of scientific innovation and global health impact. This vaccine, developed at an unprecedented pace, quickly became a vital component of many countries’ vaccination campaigns. Its efficacy, safety profile, and global distribution all deserve careful examination. We will explore the intricacies of its development, production, administration, and its impact on public perception.
From its initial research to widespread deployment, the Moderna COVID-19 vaccine journey is a testament to human ingenuity and collaborative effort. We’ll dissect the science behind its mechanism of action, the clinical trial data, and the safety measures implemented. Furthermore, we’ll analyze public acceptance, distribution challenges, and the evolving response to COVID-19 variants.
Vaccine Efficacy and Safety
The Moderna COVID-19 vaccine has emerged as a crucial tool in the fight against the pandemic. Understanding its mechanism of action, efficacy, safety profile, and long-term effects is essential for informed decision-making. This analysis delves into the key aspects of the Moderna vaccine, comparing it to other COVID-19 vaccines.The Moderna vaccine utilizes messenger RNA (mRNA) technology. This innovative approach involves introducing a piece of genetic code (mRNA) into the body.
This mRNA instructs cells to produce a harmless piece of the virus’s “spike protein.” The immune system recognizes this protein as foreign and mounts an immune response, producing antibodies and T-cells that can neutralize the virus in the future. This mRNA is encased in a lipid nanoparticle, which helps it deliver the genetic material effectively into cells.
Mechanism of Action
The mRNA vaccine instructs cells to produce a harmless piece of the virus’s spike protein. This triggers an immune response, creating antibodies and T-cells to fight off the virus if encountered later. The body learns to recognize and defend against the virus without ever having to get sick.
Clinical Trial Results
The Moderna COVID-19 vaccine demonstrated high efficacy in clinical trials. Studies showed that the vaccine was highly effective at preventing symptomatic COVID-19, reducing the risk of severe disease and hospitalization. The vaccine’s efficacy varied slightly depending on the specific trial population and the virus variant circulating at the time.
Safety Profile
The Moderna vaccine has a generally favorable safety profile. Common side effects, such as pain at the injection site, fatigue, and fever, are typically mild and temporary. Serious side effects are rare. Extensive post-authorization monitoring continues to assess long-term safety.
Reported Side Effects and Frequency
Common side effects, such as pain at the injection site, fatigue, and headache, were reported in clinical trials and post-authorization monitoring. These side effects are usually mild to moderate and resolve within a few days. Serious side effects, while rare, have been monitored and investigated.
Long-Term Effects
Long-term effects of the Moderna COVID-19 vaccine are still under investigation. Data collection is ongoing to determine the potential long-term impacts on health.
Comparison to Other COVID-19 Vaccines
Different COVID-19 vaccines employ various technologies, each with its own strengths and limitations. Some vaccines use inactivated or weakened forms of the virus, while others use viral vectors. mRNA vaccines, like Moderna, have the advantage of being adaptable to new variants. Comparative efficacy and safety data are available for different vaccines.
Dosage and Administration Schedules
| Dosage (µg) | Schedule | Notes |
|---|---|---|
| 100 | 2 doses, 28 days apart | This is the most common dosage and schedule. |
| 50 | 2 doses, 28 days apart | Some countries have used this dosage. |
| 100 | 2 doses, 4 weeks apart | This is a common dosage and schedule for the booster doses |
The table above summarizes different dosages and administration schedules for the Moderna vaccine. These schedules are based on clinical trial data and are recommended by health authorities. It’s important to note that these schedules might vary depending on the specific circumstances.
Vaccine Development and Production

The development of the Moderna COVID-19 vaccine stands as a testament to rapid scientific advancement and collaborative efforts. Leveraging innovative mRNA technology, Moderna’s approach to vaccine creation dramatically shortened the typical timeframe for vaccine development. This accelerated pace was crucial in the global fight against the pandemic.The Moderna COVID-19 vaccine utilized messenger RNA (mRNA) technology, a novel approach to vaccine design.
Getting the Moderna COVID-19 vaccine can sometimes lead to some temporary side effects, but it’s important to remember that these are generally mild and short-lived. While researching the potential side effects of the Moderna vaccine, I stumbled upon an interesting article about how certain medications, like antibiotics, can affect your digestive system, sometimes causing constipation. Understanding these potential interactions is key for managing any discomfort and knowing what to expect.
So, if you’re wondering about potential digestive issues after getting the Moderna vaccine, learning about the link between antibiotics and constipation might offer some insight. do antibiotics cause constipation Ultimately, staying informed and consulting with a healthcare professional is crucial for making informed decisions about your health.
mRNA molecules carry genetic instructions that tell cells how to make specific proteins. In this case, the mRNA coded for the SARS-CoV-2 spike protein, a key component of the virus. By introducing this mRNA into the body, the immune system was stimulated to recognize and fight the virus without actually exposing individuals to the virus itself. This method, while groundbreaking, required careful optimization and rigorous testing to ensure safety and efficacy.
Scientific Breakthroughs
The development of the Moderna COVID-19 vaccine relied heavily on advancements in mRNA technology. Researchers had been exploring mRNA vaccines for years, but the challenge was in delivering the mRNA safely and effectively to cells. Moderna’s success stemmed from their innovation in chemically modifying the mRNA to improve its stability and reduce its degradation in the body. This allowed for a more efficient delivery and expression of the spike protein.
Other key scientific breakthroughs involved optimizing the lipid nanoparticle delivery system, ensuring the mRNA reached the target cells without causing harm.
Manufacturing Process
The Moderna COVID-19 vaccine production process involves several key stages. The manufacturing process was meticulously designed to ensure quality control at each step. This was critical given the scale of production required to meet global demand.
- mRNA Synthesis: The first stage involves synthesizing the mRNA sequence that codes for the SARS-CoV-2 spike protein. This is achieved through automated processes using advanced chemical techniques. The quality and purity of the synthesized mRNA are rigorously checked to ensure the desired sequence and absence of errors.
- Lipid Nanoparticle Formation: The mRNA is encapsulated within lipid nanoparticles, a crucial component for safe and efficient delivery. These nanoparticles protect the mRNA from degradation and facilitate its entry into cells. Precise control over the lipid composition and structure is critical to optimize the delivery efficiency.
- Formulation and Filling: The formulated mRNA-lipid nanoparticle mixture is carefully filled into vials. The process is highly automated to maintain consistency and prevent contamination. Sterile conditions are maintained throughout this phase.
- Quality Control and Testing: Throughout the manufacturing process, rigorous quality control measures are in place to ensure the safety and efficacy of the vaccine. Extensive testing is performed at each stage to confirm the quality of the mRNA, lipid nanoparticles, and the final product.
Timeline, Moderna covid 19 vaccine
The rapid development of the Moderna COVID-19 vaccine was remarkable. The timeline demonstrates the power of collaboration and innovative approaches.
- Initial Research (2019-2020): Early research into mRNA technology laid the groundwork for the COVID-19 vaccine. This phase involved the optimization of mRNA stability and the design of the lipid nanoparticle delivery system.
- Clinical Trials (2020-2021): The vaccine underwent rigorous clinical trials to evaluate its safety and efficacy. The speed of these trials was unprecedented, reflecting the urgency of the pandemic.
- Emergency Use Authorization (2021): Regulatory agencies granted emergency use authorization for the vaccine, paving the way for widespread deployment.
- Widespread Deployment (2021-Present): The vaccine was distributed globally, playing a vital role in controlling the pandemic.
Key Personnel and Institutions
The development of the Moderna COVID-19 vaccine was a collaborative effort. The following table highlights key personnel and institutions involved.
| Personnel/Institution | Role |
|---|---|
| Moderna, Inc. | Lead developer and manufacturer |
| Various research institutions and universities | Contributed to mRNA technology and clinical trial participation |
| Government agencies (e.g., NIH, CDC) | Provided funding, support, and regulatory oversight |
| Clinical trial participants | Essential to evaluating vaccine safety and efficacy |
Manufacturing Stages
The manufacturing process is divided into distinct stages, each crucial for ensuring the final product’s quality and safety. Each step is meticulously controlled to maintain consistent product quality.
- mRNA Synthesis: The mRNA sequence is synthesized, validated, and purified. This step ensures the correct genetic instructions are present for protein production.
- Lipid Nanoparticle Production: Lipid nanoparticles are produced and characterized to ensure they are the right size and composition for optimal mRNA delivery.
- Mixing and Formulation: The mRNA and lipid nanoparticles are mixed and formulated to create the vaccine solution.
- Quality Control Testing: The vaccine undergoes rigorous testing at each stage to confirm its safety and effectiveness. These tests are critical to identify and eliminate any potential problems.
- Filling and Packaging: The final vaccine solution is filled into vials and packaged under sterile conditions. This process maintains the integrity of the vaccine.
Public Perception and Acceptance

Public perception of the Moderna COVID-19 vaccine played a crucial role in its adoption and ultimately, the pandemic’s trajectory. Understanding the factors driving acceptance or hesitancy is essential to future vaccine campaigns. This analysis delves into public opinion, the influence of media, and the strategies used to build trust and acceptance.The Moderna vaccine, like other COVID-19 vaccines, faced varying degrees of public acceptance and skepticism.
Public perception was shaped by a complex interplay of scientific information, personal experiences, and societal factors. Addressing concerns and building trust was paramount in ensuring widespread vaccination.
Factors Influencing Vaccine Hesitancy or Acceptance
Public trust in institutions, especially in the realm of healthcare and science, significantly influences vaccine acceptance. Perceived safety and efficacy, communicated through various channels, also play a key role. Individual beliefs, personal experiences, and the information disseminated through social networks and mainstream media contribute to the formation of opinions.
- Trust in Institutions: Public trust in healthcare providers and government agencies directly correlates with vaccination rates. When trust is high, individuals are more likely to accept recommended vaccinations. Conversely, mistrust in these institutions can lead to vaccine hesitancy.
- Perceived Safety and Efficacy: Concerns about potential side effects, even if rare, and the speed of vaccine development, have been prominent factors influencing public perception. Data on vaccine efficacy and safety, when clearly and accurately presented, can address these concerns and foster acceptance.
- Individual Beliefs and Experiences: Personal values, experiences, and social networks significantly shape individual decisions about vaccinations. Information and discussions within communities and social circles can greatly impact an individual’s willingness to get vaccinated. Pre-existing medical conditions or perceived vulnerability to severe illness may also influence decisions.
Role of Media and Social Media
The media, both traditional and social, plays a significant role in shaping public opinion about the Moderna vaccine. Accurate and balanced reporting is essential to counteract misinformation and promote trust. Social media, in particular, can be a powerful tool for disseminating information, but also a platform for the spread of misinformation.
- Media Influence: News outlets have a responsibility to present accurate and balanced information about the vaccine, including its efficacy, safety, and potential side effects. Unbiased reporting is crucial to avoid exacerbating vaccine hesitancy or acceptance based on fear-mongering or misleading information.
- Social Media Impact: Social media platforms, with their vast reach, can be significant amplifiers of both accurate and false information. Misinformation and conspiracy theories can rapidly spread, potentially undermining public trust in vaccines. Strategies to address misinformation on social media are essential to counter these effects.
Strategies for Addressing Concerns and Building Trust
Healthcare providers and public health organizations have employed various strategies to address public concerns and build trust in the Moderna vaccine. Transparency, clear communication, and personalized interactions are vital components of these efforts.
- Transparency and Open Communication: Providing readily available, accurate information about the vaccine, including its benefits and potential risks, is crucial. Clear communication, using language that is understandable to the public, fosters trust and understanding.
- Personalized Interactions: Healthcare professionals have a vital role in addressing individual concerns and answering questions. Open and honest dialogue can help build trust and reassure hesitant individuals.
- Community Engagement: Engaging with community leaders, faith-based organizations, and other influential groups can help build trust and facilitate the dissemination of accurate information.
Communicating Vaccine Information
Different approaches to communicating vaccine information to the public have been implemented. Tailoring messaging to specific audiences and using multiple communication channels are key to effective outreach.
Getting the Moderna COVID-19 vaccine was a pretty straightforward process, but I’ve been dealing with some chest discomfort lately. Turns out, it might be costochondritis. Fortunately, there are specific physical therapy exercises for managing costochondritis, like the ones detailed in this helpful guide: costochondritis physical therapy exercises. Hopefully, these exercises will help ease the pain and get me back to feeling my best, so I can focus on getting back to my normal routine after the Moderna COVID-19 vaccine.
- Targeted Messaging: Recognizing that different segments of the population may have unique concerns or needs, tailoring messages to address those concerns can improve vaccine acceptance. Understanding the perspectives and concerns of specific demographics is essential.
- Multiple Communication Channels: Utilizing various channels, including print media, online platforms, and community events, can ensure wider dissemination of information and engagement with different audiences. Using a multi-pronged approach can improve effectiveness.
Public Opinion and Beliefs Table
| Category | Beliefs/Opinions |
|---|---|
| Positive Perception | High efficacy and safety, trust in science and healthcare institutions, personal experiences supporting vaccine effectiveness. |
| Neutral Perception | Balanced views, some concerns about potential side effects, require more information and clarity. |
| Negative Perception | Skepticism regarding safety and efficacy, distrust in government and pharmaceutical companies, conspiracy theories and misinformation. |
Global Distribution and Accessibility: Moderna Covid 19 Vaccine
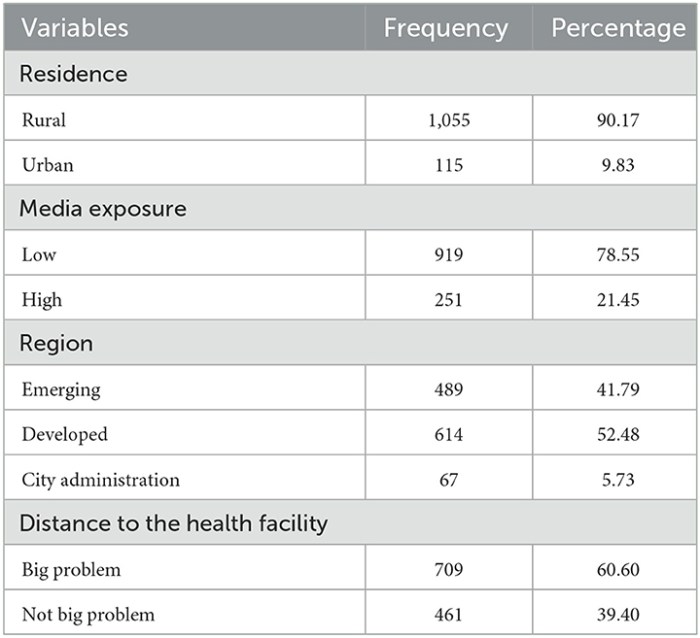
The global distribution of the Moderna COVID-19 vaccine has been a complex undertaking, shaped by factors like manufacturing capacity, logistical hurdles, and geopolitical considerations. Ensuring equitable access across diverse regions has presented significant challenges, particularly in low- and middle-income countries. This necessitates a comprehensive understanding of the distribution strategies employed, the role of international organizations, and the factors influencing distribution rates.
Overview of Global Distribution
The Moderna COVID-19 vaccine, like other vaccines, has faced challenges in reaching all corners of the world. Initial production capacity and the need for stringent cold-chain logistics have significantly impacted distribution. The distribution was heavily influenced by pre-existing healthcare infrastructure, vaccine hesitancy, and the need for robust cold-chain systems in some regions.
Challenges in Equitable Access
Several challenges have hindered equitable access to the Moderna vaccine. These include variations in healthcare infrastructure, economic disparities, political instability, and differing levels of vaccine confidence across regions. Limited cold-chain infrastructure in some developing countries, coupled with the vaccine’s need for ultra-low temperatures, has hampered distribution in these areas.
Strategies for Improved Accessibility in Low-Resource Settings
Several strategies have been implemented to improve vaccine accessibility in low-resource settings. These include partnerships with local organizations, the provision of cold-chain equipment, training programs for healthcare workers, and targeted outreach programs. Utilizing existing distribution networks, such as those employed for routine immunizations, can be a key element in improving vaccine access.
Distribution of Moderna Vaccine Doses
The distribution of Moderna vaccine doses across countries has varied considerably. Factors such as vaccination campaigns, population size, and existing healthcare infrastructure have influenced the rates. A precise breakdown of doses distributed is difficult to obtain due to varying reporting standards and data availability.
| Country | Estimated Doses Distributed | Challenges Encountered |
|---|---|---|
| United States | High | Efficient infrastructure and strong healthcare system |
| India | Moderate | Large population, varying cold chain capabilities |
| Sub-Saharan Africa | Low | Limited cold chain infrastructure, varying access to healthcare |
| South America | Moderate to High | Varying levels of infrastructure and vaccination campaigns |
Note: This table provides a simplified overview. Actual figures are often incomplete and can vary based on reporting standards and data collection methods.
Role of International Organizations
International organizations, such as the World Health Organization (WHO) and UNICEF, play a crucial role in facilitating vaccine access. These organizations provide technical support, financial assistance, and logistical guidance to countries in need. Their role is critical in coordinating global efforts and ensuring equitable distribution.
Factors Affecting Distribution Rates
Several factors influence the Moderna vaccine distribution rates in different regions. These include the availability of funding, the effectiveness of vaccination campaigns, logistical hurdles, and the presence of political or social barriers. Furthermore, the level of trust in the vaccine among the population can also impact the distribution rates. The availability of appropriate cold-chain storage and transport infrastructure is also a critical factor.
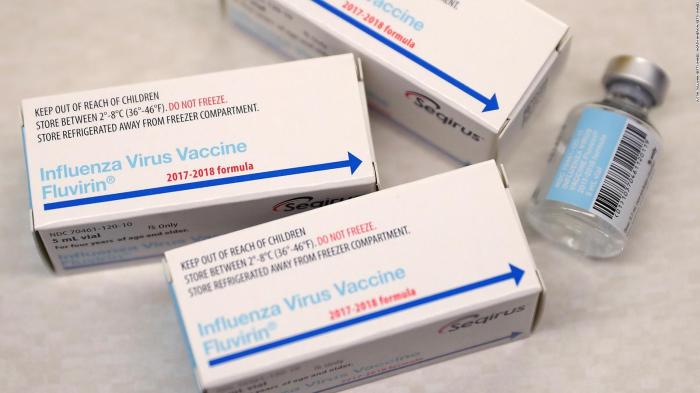
Vaccine Administration and Protocols
The safe and effective administration of the Moderna COVID-19 vaccine is crucial for achieving herd immunity and controlling the pandemic. Proper storage, handling, and injection techniques, combined with adherence to recommended protocols, minimize risks and maximize the vaccine’s efficacy. Understanding these aspects is essential for healthcare providers and individuals alike.
Recommended Dosage and Administration Schedule
The Moderna COVID-19 vaccine requires two doses administered intramuscularly. The recommended interval between doses is 28 days. Each dose contains 100 micrograms of mRNA. The administration schedule ensures a robust immune response.
Getting the Moderna COVID-19 vaccine is a crucial step in protecting yourself and others. While it’s important to be informed about potential side effects, it’s also helpful to understand similar symptoms. Sometimes, a drool rash or hand, foot, and mouth disease can present with symptoms that mimic those of vaccination reactions. For a deeper understanding of differentiating between drool rash and hand-foot-and-mouth disease, check out this helpful resource: drool rash vs hand foot mouth.
Ultimately, knowing the differences between these conditions can help you better assess any post-vaccination symptoms.
Proper Storage and Handling Procedures
Maintaining the vaccine’s integrity is critical. The Moderna COVID-19 vaccine must be stored at -20°C ( -4°F) or colder. Dedicated freezers and appropriate packaging are essential for proper storage. Strict adherence to temperature-monitoring procedures is paramount. This includes regular checks of the freezer’s temperature to ensure it remains within the required range.
Any deviation from the recommended temperature range can compromise the vaccine’s efficacy. If the vaccine is accidentally thawed, it should not be used.
Importance of Following Recommended Protocols
Adherence to the recommended protocols ensures the vaccine’s safety and effectiveness. Deviation from these protocols can introduce risks to individuals receiving the vaccine. These protocols, established by rigorous scientific studies and clinical trials, guarantee optimal immune response. Following the recommended protocols minimizes potential risks and maximizes the vaccine’s impact.
Safety Measures During Vaccine Administration
These measures aim to mitigate risks and ensure a safe experience for the recipient.
| Safety Measure | Description |
|---|---|
| Pre-Administration Screening | Thorough evaluation of the recipient’s medical history and identification of any contraindications. |
| Allergy Assessment | Identifying any known allergies to vaccine components. |
| Proper Injection Site Selection | Choosing a suitable injection site on the upper arm. |
| Post-Injection Monitoring | Observing the recipient for 15-30 minutes for any immediate adverse reactions. |
| Documentation | Maintaining accurate records of the administration, including the date, time, lot number, and any observed reactions. |
Proper Injection Technique for the Moderna COVID-19 Vaccine
The injection technique is critical for minimizing discomfort and maximizing efficacy. The vaccine should be administered intramuscularly into the deltoid muscle of the upper arm. Proper needle insertion angle and depth are vital. Using appropriate injection equipment and technique helps to minimize pain and potential complications.
Potential Adverse Reactions and Management
Common adverse reactions include pain, redness, and swelling at the injection site. These are generally mild and temporary. More severe reactions, although rare, may occur. In case of severe or persistent reactions, medical attention should be sought immediately. This proactive approach to potential adverse reactions ensures swift and appropriate management.
COVID-19 Variants and Vaccine Response
The emergence of COVID-19 variants has presented a significant challenge to global vaccination efforts. Understanding how these variants impact vaccine effectiveness is crucial for adapting strategies to maintain protection against the virus. This necessitates ongoing research and the development of updated vaccine formulations to ensure continued efficacy against the evolving viral landscape.
Variability in Vaccine Effectiveness Against Variants
The Moderna vaccine, like other mRNA vaccines, is designed to elicit an immune response against specific viral proteins. However, mutations in the virus can alter these proteins, potentially reducing the vaccine’s ability to induce a protective immune response. Different variants exhibit varying degrees of these mutations, impacting the vaccine’s effectiveness. Some variants, such as Delta and Omicron, demonstrated reduced neutralization capacity compared to earlier strains, meaning the vaccine’s ability to prevent infection was lessened.
This highlights the dynamic nature of the virus and the importance of continuous monitoring and adaptation.
Ongoing Research into Vaccine Efficacy Against Emerging Variants
Extensive research continues to assess the Moderna vaccine’s efficacy against emerging variants. Scientists analyze data from clinical trials and real-world scenarios to understand how well the vaccine performs against new variants. This includes studying antibody responses, cellular immunity, and overall protection against infection and severe disease. Studies are also focusing on the neutralization capacity of antibodies elicited by the vaccine against these variants, which is crucial for determining the efficacy of vaccine-induced immunity.
For example, laboratory experiments are carried out to assess the ability of antibodies generated by the vaccine to bind to and neutralize different variants.
Strategies for Adapting the Vaccine to New Variants
Various strategies are employed to adapt the vaccine to emerging variants. One approach involves modifying the vaccine’s target sequence to better match the variant’s mutated proteins. For instance, Moderna has developed updated formulations tailored to address specific mutations present in certain variants. Another strategy involves booster shots containing sequences targeted to more recent variants. This approach aims to enhance the immune response against these evolving strains.
Moreover, ongoing research investigates whether combining different vaccine platforms or using adjuvants can further enhance vaccine effectiveness against a wider range of variants.
Comparison of Moderna Vaccine Effectiveness Against Variants
| Variant | Moderna Vaccine Effectiveness (Approximate) | Factors Contributing to Effectiveness/Reduced Effectiveness |
|---|---|---|
| Original Strain | High | Effective neutralization of the initial virus strain. |
| Alpha | High | Strong antibody response against the mutated protein. |
| Beta | Moderate | Reduced neutralization capacity compared to the original strain, although still significant protection. |
| Delta | Moderate to Low | Significant reduction in neutralization capacity, requiring booster shots. |
| Omicron | Low | Significant reduction in neutralization capacity, leading to a need for booster shots and/or updated vaccine formulations. |
Note: Effectiveness data is approximate and based on available research. Effectiveness can vary based on factors like dosage, individual immune response, and time since vaccination.
Factors Influencing Vaccine Effectiveness
Several factors influence the vaccine’s effectiveness against different variants. These include the specific mutations in the viral proteins, the strength of the immune response elicited by the vaccine, the presence of pre-existing immunity, and the duration of protection provided by the vaccine. For example, the immune system’s response to certain variants might be less robust, leading to reduced protection compared to other variants.
Further research is crucial to identify and quantify these factors in relation to different variants.
Need for Vaccine Updates or Boosters
The emergence of variants with reduced susceptibility to existing vaccines necessitates vaccine updates or booster shots. Booster doses provide a “top-up” to the immune system, enhancing its ability to recognize and combat the evolving virus. This approach is particularly important for variants like Omicron, which exhibited significantly reduced neutralization compared to earlier variants. Regular monitoring of variant evolution and efficacy studies are critical to inform decisions about the need for updated vaccines or booster shots.
Final Review
In conclusion, the Moderna COVID-19 vaccine stands as a pivotal moment in modern medicine. Its rapid development and deployment showcased the potential of cutting-edge technologies, but also highlighted the complexities of global health challenges. The vaccine’s efficacy and safety, alongside public perception and equitable distribution, are critical factors that continue to shape its legacy. As we move forward, it’s essential to continue evaluating and adapting to the ever-changing landscape of the pandemic and the role vaccines play in its mitigation.




![Marc Ecko's Getting Up: Contents Under Pressure [Mobile] What will happen if i get a flu shot while im sick](https://healthytipp.com/wp-content/uploads/2025/06/ss_b0efcf546b861e6fbb6f6a703c2374536af761f5.1920x1080-1.jpg)